LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can you drink soda on semaglutide? While there's no official FDA prohibition against consuming soda with injectable semaglutide (Ozempic, Wegovy), this common question deserves careful consideration beyond simple safety. Semaglutide, a GLP-1 receptor agonist used for type 2 diabetes and weight management, fundamentally changes how your body processes food and beverages through delayed gastric emptying and appetite suppression. Regular soda's high sugar content can undermine blood glucose control, while carbonation may worsen common gastrointestinal side effects like nausea and bloating. Understanding how soda interacts with your treatment helps optimize therapeutic outcomes while maintaining quality of life during therapy.
Quick Answer: You can drink soda with injectable semaglutide from a safety perspective, but it may worsen gastrointestinal side effects and undermine diabetes or weight management goals.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication mimics the action of naturally occurring GLP-1, a hormone released by the intestine in response to food intake. By binding to GLP-1 receptors in the pancreas, brain, and gastrointestinal tract, semaglutide produces several metabolic effects that fundamentally alter how patients experience eating and drinking.
The primary mechanisms include enhanced glucose-dependent insulin secretion, suppression of inappropriately elevated glucagon levels, and delayed gastric emptying. This slowed movement of food from the stomach into the small intestine is particularly significant for dietary tolerance, though this effect may diminish somewhat with continued use. Patients commonly report reduced appetite, earlier satiety with smaller portions, and decreased food cravings—effects mediated through central appetite regulation in the hypothalamus.
Importantly, oral semaglutide (Rybelsus) has specific administration requirements: it must be taken with no more than 4 ounces of plain water only, followed by at least 30 minutes without any food, beverages, or other oral medications. This restriction is critical for proper absorption of the medication.
While semaglutide does not prohibit specific foods or beverages outside these administration windows, its effects on gastric motility and satiety signals can make certain dietary patterns more or less tolerable. Understanding this interaction is essential for optimizing both therapeutic outcomes and quality of life, as poor dietary choices may exacerbate common adverse effects or undermine the metabolic benefits that semaglutide provides.
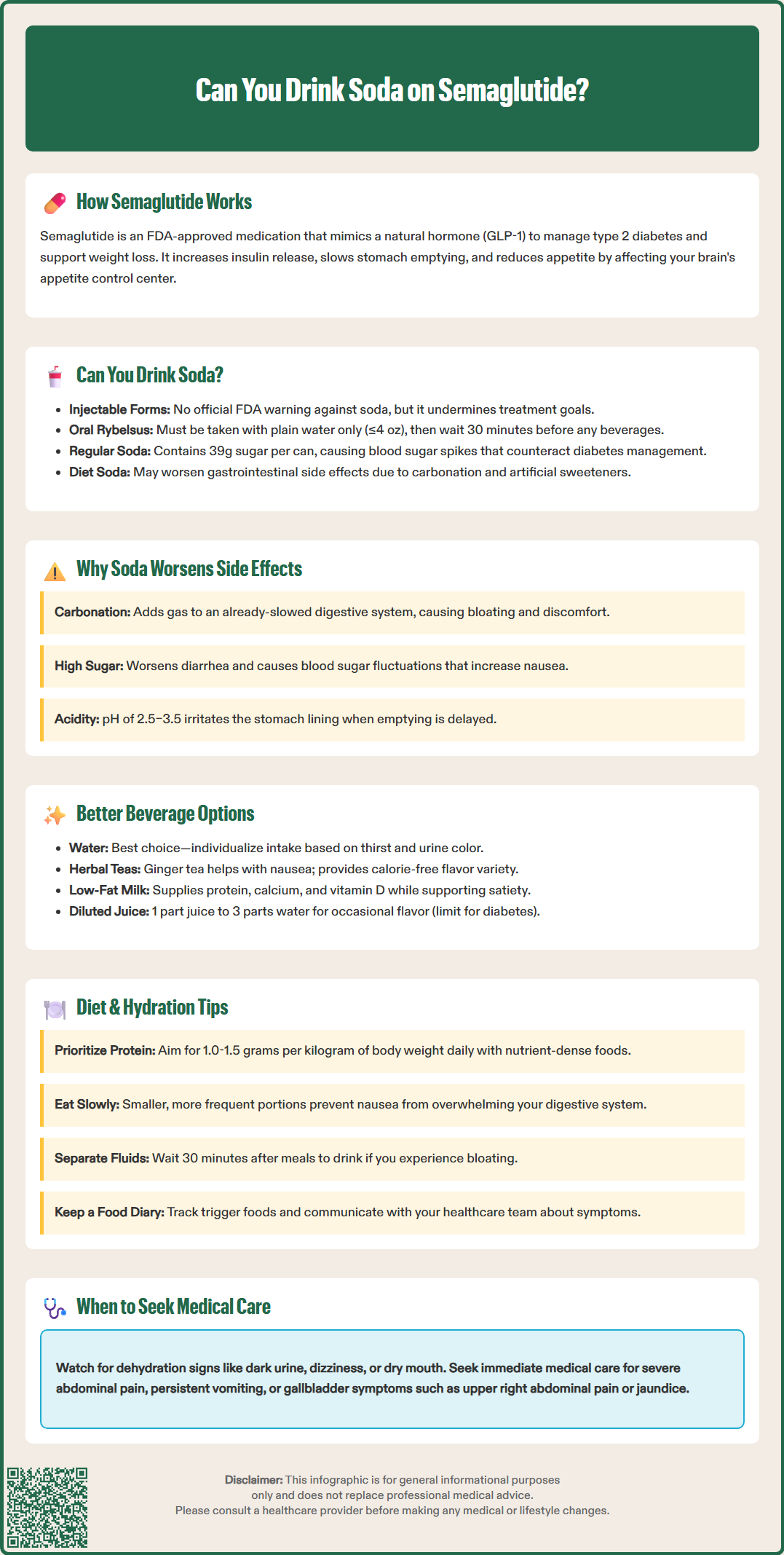
For injectable semaglutide (Ozempic, Wegovy), there is no official contraindication or FDA warning against drinking soda. The prescribing information does not list carbonated beverages or sugar-sweetened drinks as substances that must be avoided, and injectable semaglutide does not have known drug-nutrient interactions that would make soda consumption dangerous from a safety standpoint.
However, for oral semaglutide (Rybelsus), the FDA label explicitly states it must be taken with no more than 4 ounces of plain water only, with no food or beverages for at least 30 minutes afterward. Consuming soda at or near the time of dosing will significantly reduce medication absorption and effectiveness.
Beyond administration requirements, the absence of a formal restriction does not mean soda is advisable or compatible with treatment goals. For patients using semaglutide for type 2 diabetes, regular soda presents a significant concern: a typical 12-ounce can contains approximately 39 grams of rapidly absorbed simple sugars, causing substantial postprandial glucose excursions that directly counteract the medication's glycemic benefits. The American Diabetes Association consistently recommends limiting sugar-sweetened beverages as a core dietary strategy for diabetes management.
For those using semaglutide for weight management, soda contributes empty calories without nutritional value or satiety benefit. A single can of regular soda provides 140–150 calories that do not trigger the fullness signals semaglutide enhances, potentially displacing more nutrient-dense options and slowing weight loss progress. Even diet sodas, while calorie-free, may present tolerability issues due to carbonation and artificial sweeteners.
The practical answer is nuanced: while you can drink soda on injectable semaglutide from a safety perspective (and with oral semaglutide outside the administration window), doing so may undermine your therapeutic goals and worsen treatment-related side effects.
Gastrointestinal adverse effects are the most common side effects of semaglutide, with rates varying by product and dose. For Wegovy (weight management), nausea occurs in up to 44% of patients, with diarrhea, vomiting, and constipation also commonly reported. Ozempic (diabetes) has somewhat lower rates, though still significant. These effects result partly from the delayed gastric emptying that contributes to semaglutide's efficacy, creating a physiological environment where certain foods and beverages are poorly tolerated.
Carbonation introduces gas into an already-slowed digestive system. When gastric emptying is delayed, carbonated beverages can increase gastric distension, bloating, and discomfort. Patients frequently report that carbonation feels "trapped" or causes uncomfortable pressure, particularly when consumed with or shortly after meals. This mechanical effect is independent of whether the soda is regular or diet.
High sugar content in regular soda presents additional concerns. Concentrated simple sugars can draw water into the intestinal lumen through osmotic effects, potentially triggering or worsening diarrhea—already a common semaglutide side effect. The rapid glucose load may also cause blood sugar fluctuations, particularly in patients taking concurrent diabetes medications like insulin or sulfonylureas, which could compound feelings of nausea or discomfort.
Most diet sodas contain non-nutritive sweeteners such as aspartame, sucralose, acesulfame K, or stevia rather than sugar alcohols. While generally recognized as safe, these sweeteners can cause gastrointestinal distress in some individuals. Some patients report that artificial sweeteners trigger nausea or alter taste perception, which is already affected in some semaglutide users. The acidity of most sodas (pH 2.5–3.5) may also irritate the gastric mucosa and contribute to dyspepsia, especially when gastric emptying is prolonged and acid exposure time is extended.
Optimal hydration is essential during semaglutide therapy, both for general health and to mitigate gastrointestinal side effects. Water remains the gold standard beverage choice—calorie-free, well-tolerated, and essential for preventing dehydration that can occur with nausea, vomiting, or diarrhea. Rather than aiming for a fixed amount like 64 ounces daily, patients should individualize fluid intake based on thirst, urine color (pale yellow indicates good hydration), climate, activity level, and medical conditions. Those with heart failure, kidney disease, or other conditions requiring fluid restriction should follow their healthcare provider's specific guidance.
For those seeking flavor variety, several alternatives provide better compatibility with semaglutide therapy:
Herbal and caffeine-free teas offer flavor without calories or carbonation. Ginger tea may help with nausea for some patients, though evidence is limited. Note that peppermint tea, while soothing for some, may worsen reflux symptoms in others.
Infused water with fresh fruit, cucumber, or herbs provides subtle flavor enhancement without added sugars or artificial ingredients. This approach maintains hydration while making water consumption more appealing for patients who struggle with plain water.
Low-fat or skim milk provides protein, calcium, and vitamin D while contributing to satiety—important when appetite is suppressed and nutrient intake may be reduced. For lactose-intolerant patients, lactose-free milk or fortified plant-based alternatives (unsweetened almond, soy, or oat milk) offer similar benefits.
Diluted fruit juice (one part juice to three parts water) can provide flavor while limiting sugar concentration. However, even diluted juice can raise blood glucose levels, so patients with diabetes should monitor their response and consider this an occasional option rather than a regular substitute.
Remember that oral semaglutide (Rybelsus) must be taken with plain water only (≤4 oz) and followed by at least 30 minutes without any food or beverages to ensure proper absorption.
Successful dietary management during semaglutide therapy requires attention to both what and how you consume foods and beverages. These strategies can help optimize treatment outcomes while minimizing adverse effects:
Prioritize protein and nutrient density. With reduced appetite and smaller portion tolerance, every bite and sip should contribute meaningful nutrition. Focus on lean proteins, vegetables, whole grains, and healthy fats rather than empty calories from sugary beverages. Protein needs vary by individual—generally 1.0-1.5 grams per kilogram of body weight daily is appropriate during weight loss, but consult your healthcare provider or dietitian for personalized recommendations, especially if you have kidney disease or other conditions affecting protein metabolism.
Eat and drink slowly. Delayed gastric emptying means your stomach needs more time to process intake. Sip beverages gradually rather than drinking large volumes quickly, which can trigger nausea and discomfort. Similarly, eat smaller, more frequent meals rather than large portions that may overwhelm your slowed digestive system.
Consider separating eating and drinking. Some patients find that consuming beverages with meals increases bloating and fullness to uncomfortable levels. If this affects you, try drinking fluids 30 minutes before or after meals rather than during eating to improve tolerance.
Monitor for dehydration. Gastrointestinal side effects can lead to fluid losses. Watch for signs including dark urine, dizziness, dry mouth, or decreased urination. If vomiting or diarrhea occurs, increase fluid intake and consider electrolyte replacement solutions. Contact your healthcare provider if you cannot maintain adequate hydration.
Know the warning signs. Seek immediate medical attention for severe or persistent abdominal pain (especially if radiating to the back), which could indicate pancreatitis; persistent vomiting or signs of severe dehydration; or symptoms of gallbladder disease such as upper right abdominal pain, fever, or yellowing of the skin or eyes.
Keep a symptom diary. Track which foods and beverages worsen or improve your symptoms. Individual tolerance varies significantly, and identifying your personal triggers allows for tailored dietary adjustments.
Communicate with your healthcare team. Report persistent nausea, vomiting, or inability to maintain adequate nutrition or hydration. Dose adjustments, anti-nausea medications, or dietary counseling with a registered dietitian may be appropriate. Never discontinue semaglutide without medical guidance, as abrupt cessation can affect glycemic control in diabetes patients.
Injectable semaglutide (Ozempic, Wegovy) has no official FDA restriction against soda consumption. However, oral semaglutide (Rybelsus) must be taken with plain water only, and soda can undermine treatment goals for both diabetes and weight management regardless of formulation.
Carbonation increases gastric distension and bloating when stomach emptying is already delayed by semaglutide. High sugar content can trigger diarrhea through osmotic effects, while acidity may irritate the stomach lining and worsen nausea.
Water remains the best choice for hydration during semaglutide therapy. Other well-tolerated options include herbal teas, infused water with fresh fruit, low-fat milk, and diluted fruit juice, all of which provide better nutritional value without worsening gastrointestinal side effects.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.