LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many people taking metformin for type 2 diabetes wonder whether eggs are safe to include in their diet. The good news is that you can safely eat eggs while taking metformin—there are no direct drug-food interactions between this first-line diabetes medication and eggs. Eggs provide high-quality protein, essential vitamins, and minerals that can support a balanced diabetes management plan. While eggs themselves are compatible with metformin therapy, understanding how to incorporate them into a heart-healthy eating pattern, along with proper medication timing and overall dietary strategies, helps optimize your diabetes control and metabolic health.
Quick Answer: Yes, you can safely eat eggs while taking metformin, as there are no direct drug-food interactions between this diabetes medication and eggs.
Yes, you can safely eat eggs while taking metformin. There is no direct drug-food interaction between metformin and eggs that would require you to avoid this nutritious food. Metformin, a first-line medication for type 2 diabetes, does not interact with the proteins, fats, or other nutrients found in eggs in a way that compromises the medication's effectiveness or increases adverse effects.
Eggs are a nutrient-dense food that can be part of a balanced diet for individuals managing diabetes with metformin. They provide high-quality protein, essential vitamins including B12 and D, and minerals such as selenium and choline. While protein-containing foods like eggs may help promote satiety as part of a balanced meal, individual glycemic responses can vary.
However, dietary considerations for people taking metformin extend beyond simple drug-food interactions. The overall quality of your diet, portion sizes, and meal timing all play important roles in diabetes management. While eggs themselves are compatible with metformin therapy, how you prepare them matters. Eggs fried in excessive butter or served with high-sodium processed meats may not support optimal metabolic health.
The American Diabetes Association (ADA) emphasizes individualized nutrition therapy for diabetes management, with no single ideal eating pattern for all people with diabetes. Most people with type 2 diabetes can include eggs as part of a heart-healthy eating pattern. If you have concerns about cholesterol intake or cardiovascular risk factors, discuss your specific dietary needs with your healthcare provider or a registered dietitian who can provide personalized guidance based on your complete medical profile.
Metformin (dimethyl biguanide) works primarily by reducing hepatic glucose production and improving insulin sensitivity in peripheral tissues. The medication decreases the amount of glucose released by the liver, particularly during fasting states, and enhances glucose uptake in skeletal muscle. Unlike sulfonylureas or insulin, metformin does not typically cause hypoglycemia when used as monotherapy because it does not stimulate insulin secretion.
The medication is absorbed primarily in the small intestine, with bioavailability of approximately 50-60% under fasting conditions. Food effects vary by formulation. For immediate-release metformin, food may slow the rate but not significantly reduce the extent of absorption. For some extended-release formulations, food can actually increase drug exposure. This is why metformin is often recommended to be taken with meals—not because of specific food interactions, but to minimize gastrointestinal side effects such as nausea, diarrhea, and abdominal discomfort.
Dietary considerations when taking metformin focus more on supporting overall glycemic control rather than avoiding specific drug-food interactions. A balanced diet that emphasizes whole grains, lean proteins, healthy fats, and abundant vegetables helps optimize metformin's glucose-lowering effects. Consistent carbohydrate intake across meals can help maintain stable blood glucose levels.
One important nutritional consideration with long-term metformin use is vitamin B12 deficiency. Metformin can interfere with B12 absorption, particularly with higher doses and longer duration of therapy. The ADA recommends periodic measurement of vitamin B12 levels in metformin-treated patients, especially those with anemia or peripheral neuropathy. While eggs contain B12 (about 0.6 micrograms per large egg), dietary sources alone may not prevent metformin-related B12 deficiency since the issue involves absorption. Supplementation may be necessary if levels are low.
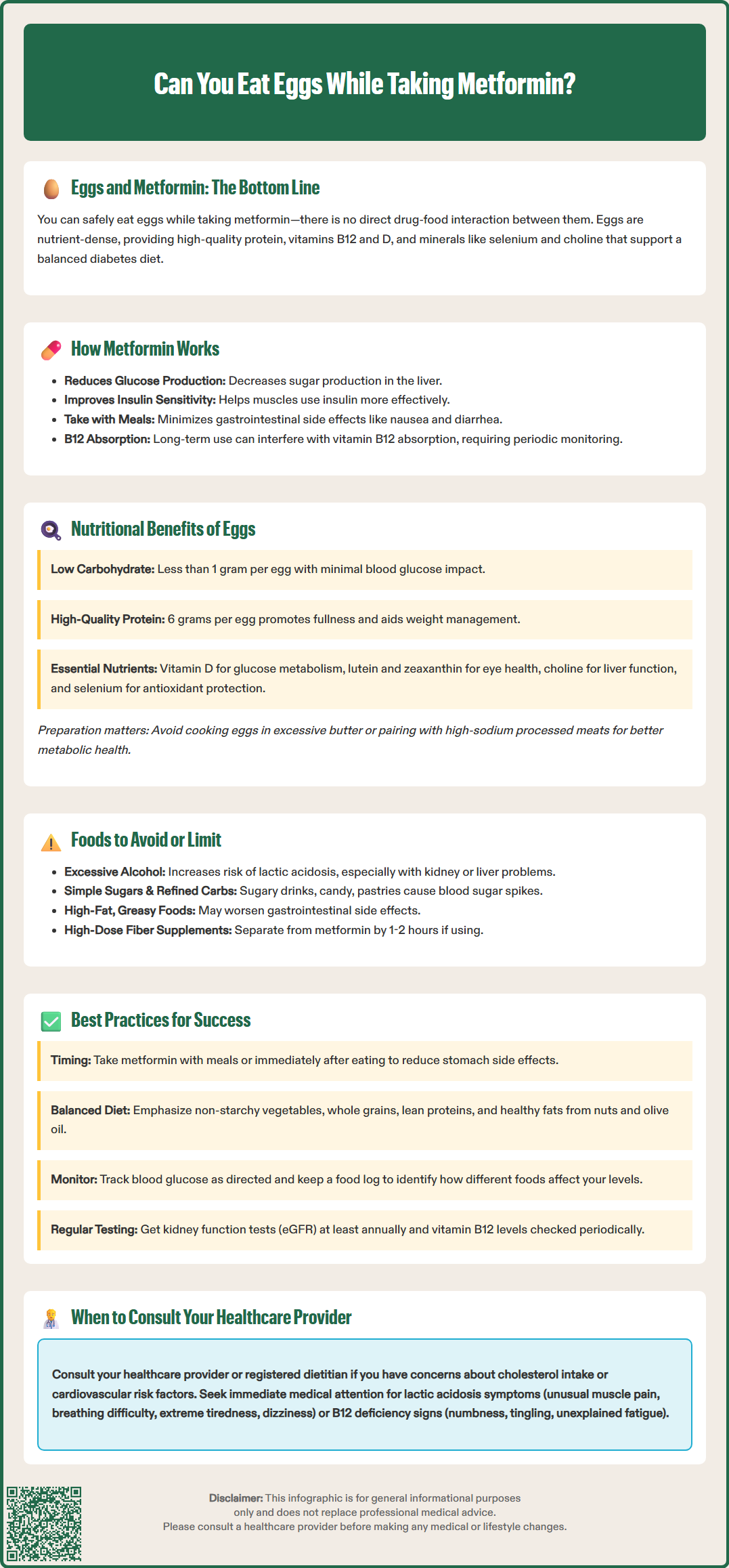
Eggs offer several nutritional advantages for individuals managing type 2 diabetes with metformin. One large egg contains approximately 6 grams of high-quality protein, 5 grams of fat, and less than 1 gram of carbohydrate, making eggs a low-glycemic food that has minimal direct impact on blood glucose levels. This macronutrient profile can support glucose control when eggs are incorporated into balanced meals.
The protein content in eggs promotes satiety and can help with weight management, which is particularly relevant for people with type 2 diabetes. Research suggests that higher protein intake at breakfast, such as from eggs, may help with glycemic control throughout the day. Protein also helps preserve lean muscle mass during weight loss, which is important for maintaining insulin sensitivity.
Eggs contain several micronutrients that may support metabolic health. They provide vitamin D, which has been associated with glucose metabolism, though evidence for direct glycemic benefits remains inconsistent. Eggs also contain lutein and zeaxanthin, carotenoids that have antioxidant properties and are being studied for potential benefits in eye health, including in diabetes. The choline in eggs supports liver health and lipid metabolism, while selenium contributes to antioxidant defense systems.
Regarding dietary cholesterol, the 2020-2025 Dietary Guidelines for Americans no longer include a specific limit on dietary cholesterol, though they advise keeping intake as low as possible while consuming a healthy dietary pattern. Evidence on egg consumption and cardiovascular risk in people with diabetes is mixed, with some studies showing neutral effects and others suggesting potential concerns in certain subgroups. Those with established cardiovascular disease or multiple risk factors should discuss individualized recommendations with their healthcare provider.
While metformin does not have extensive food-drug interactions requiring strict dietary restrictions, certain foods and beverages warrant caution or moderation. Alcohol consumption is the most important dietary consideration with metformin therapy. The FDA advises against excessive alcohol intake (acute or chronic) while taking metformin, as it can increase the risk of lactic acidosis, a rare but serious complication, particularly in individuals with kidney or liver impairment. Avoid binge drinking, and if you do consume alcohol, discuss safe limits with your healthcare provider based on your individual health status.
Very high doses of fiber supplements (such as psyllium) taken simultaneously with metformin might theoretically affect absorption. However, normal dietary fiber from whole foods is beneficial for diabetes management and should not be avoided. If you use fiber supplements, consider separating them from metformin doses by 1-2 hours, though this is not typically a significant concern for most patients.
Foods high in simple sugars and refined carbohydrates can counteract metformin's glucose-lowering effects. While these foods do not directly interact with the medication, they can cause rapid blood glucose spikes that make diabetes management more challenging. Limiting sugar-sweetened beverages, candy, pastries, and highly processed snacks supports better glycemic control when combined with metformin therapy.
Certain foods may exacerbate metformin's gastrointestinal side effects. High-fat, greasy, or spicy foods can worsen nausea and diarrhea, particularly when initiating metformin or increasing the dose. Gradually introducing metformin and taking it with meals can help minimize these effects. If gastrointestinal symptoms persist, extended-release formulations of metformin may be better tolerated. Regarding vitamin B12, be aware that metformin can reduce absorption despite adequate dietary intake; periodic monitoring and possible supplementation may be necessary.
Optimizing metformin therapy involves coordinating medication timing with meals and following evidence-based dietary patterns. Take metformin with meals or immediately after eating to minimize gastrointestinal side effects. If you are prescribed immediate-release metformin twice daily, taking it with breakfast and dinner provides consistent medication levels throughout the day. Extended-release formulations should be taken with a meal as directed on the product label.
Adopt a balanced eating pattern that emphasizes nutrient-dense, minimally processed foods. The ADA recognizes a variety of eating patterns for diabetes management, including Mediterranean-style, DASH (Dietary Approaches to Stop Hypertension), and plant-based diets. These approaches share common elements: abundant non-starchy vegetables, whole grains, lean proteins (including eggs), healthy fats from sources like nuts and olive oil, and limited added sugars and sodium. Portion control and consistent meal timing help maintain stable blood glucose levels.
Monitor your blood glucose levels as recommended by your healthcare provider to understand how different foods affect your individual response. This information helps you make informed dietary choices that complement metformin therapy. Keep a food and glucose log if you are experiencing difficulty achieving glycemic targets, as this can reveal patterns and guide adjustments to your eating plan.
Regular follow-up with your healthcare team is essential for successful diabetes management. Schedule periodic appointments to assess your A1C, kidney function, and vitamin B12 levels. Your healthcare provider should check your kidney function (eGFR) before starting metformin and at least annually thereafter. Metformin is typically not recommended for initiation in patients with an eGFR between 30-45 mL/min/1.73m² unless benefits outweigh risks, and is contraindicated if eGFR is below 30. If you need an imaging procedure with iodinated contrast, metformin may need to be temporarily discontinued, especially if you have reduced kidney function.
Discuss any persistent gastrointestinal symptoms with your provider, as dose adjustments or formulation changes may improve tolerance. If you experience symptoms of lactic acidosis (unusual muscle pain, difficulty breathing, stomach discomfort, unusual tiredness, dizziness, or cold/blue skin), seek immediate medical attention. Report any signs of vitamin B12 deficiency, such as numbness, tingling, or unexplained fatigue, to your healthcare provider for appropriate evaluation and management.
Take metformin with meals or immediately after eating to minimize gastrointestinal side effects such as nausea and diarrhea. Whether your meal includes eggs or other foods does not affect this recommendation, as the timing relates to reducing side effects rather than specific food interactions.
Eggs have minimal direct impact on blood glucose levels because they contain less than 1 gram of carbohydrate per large egg. The high-quality protein in eggs may actually help promote satiety and support stable blood sugar when incorporated into balanced meals alongside metformin therapy.
Avoid excessive alcohol consumption while taking metformin, as it increases the risk of lactic acidosis, particularly in those with kidney or liver impairment. Limit foods high in simple sugars and refined carbohydrates, as they can counteract metformin's glucose-lowering effects and make diabetes management more challenging.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.