LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Many patients taking semaglutide (Ozempic, Wegovy, Rybelsus) experience constipation as a side effect, leading to questions about whether laxatives can be safely used alongside this medication. Semaglutide, a GLP-1 receptor agonist approved for type 2 diabetes and weight management, slows gastric emptying—a mechanism that improves blood sugar control and promotes satiety but can also affect bowel function. Constipation occurs in approximately 24% of patients on weight-management doses. While there is no official contraindication to using laxatives with semaglutide, understanding which types are appropriate and when to seek medical guidance is essential for safe, effective symptom management.
Quick Answer: Yes, you can generally take laxatives while on semaglutide, as there is no official contraindication, though consultation with a healthcare provider is recommended.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the natural hormone GLP-1, which stimulates insulin secretion, suppresses glucagon release, and slows gastric emptying. While these mechanisms contribute to improved glycemic control and weight loss, they also directly affect gastrointestinal function.
Digestive side effects are among the most commonly reported adverse reactions to semaglutide therapy. According to FDA prescribing information, gastrointestinal symptoms vary by formulation and dose, with higher rates at weight-management doses. For Ozempic (diabetes dosing), nausea affects approximately 15-20% of patients, while Wegovy (weight management dosing) has higher rates of nausea (up to 44%) and constipation (approximately 24%). Other common GI effects include vomiting, diarrhea, and abdominal pain. These effects typically emerge during dose escalation periods.
Constipation rates vary by dose and indication, with higher incidence in patients taking weight-management doses. The slowed gastric emptying that contributes to satiety and weight loss can delay intestinal transit time, potentially leading to harder stools and difficulty with bowel movements. Many patients find that GI side effects improve after completing the dose escalation period, though some may experience persistent symptoms. Notably, semaglutide is not recommended for patients with severe gastroparesis or severe gastrointestinal disease. For many patients experiencing constipation, questions arise about whether over-the-counter remedies like laxatives can be safely used alongside their prescribed semaglutide therapy.
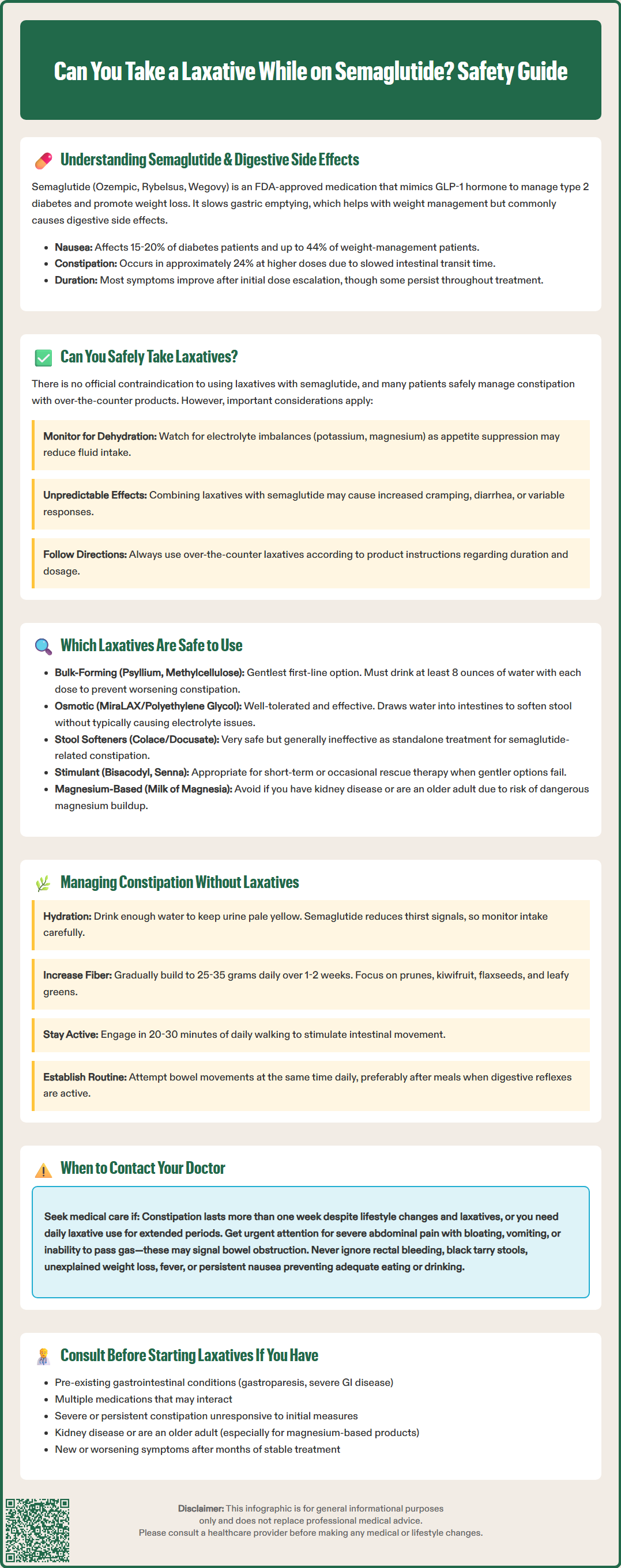
There is no official contraindication to using laxatives while taking semaglutide, and many patients safely manage constipation with over-the-counter laxative products. The FDA prescribing information for semaglutide products does not list laxatives among medications that should be avoided, nor does it warn against their concurrent use. However, the interaction between these medications requires thoughtful consideration due to semaglutide's effect on gastrointestinal motility.
The primary concern with combining laxatives and semaglutide relates to the potential for compounding gastrointestinal effects. Since semaglutide slows gastric emptying and alters gut motility, adding a laxative—particularly stimulant types—may lead to variable responses in different patients. Some may experience more pronounced laxative effects, leading to diarrhea, cramping, or electrolyte disturbances. While there is limited evidence that semaglutide specifically reduces laxative effectiveness, patients should be aware that individual responses may vary.
Patient safety considerations include monitoring for dehydration, especially if laxative use leads to loose stools or diarrhea in someone already experiencing nausea or reduced fluid intake. Electrolyte imbalances, particularly involving potassium and magnesium, can occur with prolonged or excessive laxative use. These concerns are heightened in patients taking semaglutide who may have reduced oral intake due to appetite suppression.
Before starting any laxative while on semaglutide, patients should consult their healthcare provider or pharmacist. This is particularly important for individuals with pre-existing gastrointestinal conditions, those taking multiple medications, or anyone experiencing severe or persistent constipation that may indicate a more serious underlying issue. Patients should also follow the directions on over-the-counter laxative products regarding duration of use and when to seek medical advice.
When laxative use becomes necessary for patients on semaglutide, certain types are generally considered safer and more appropriate than others. Bulk-forming laxatives such as psyllium (Metamucil), methylcellulose (Citrucel), and wheat dextrin represent the gentlest first-line option. These products work by absorbing water and increasing stool bulk, which stimulates natural peristalsis. They typically produce effects within 12-72 hours and are less likely to cause cramping or urgent bowel movements. However, adequate fluid intake is essential—patients should consume at least 8 ounces of water with each dose to prevent paradoxical worsening of constipation or potential bowel obstruction.
Osmotic laxatives including polyethylene glycol 3350 (MiraLAX), lactulose, and magnesium hydroxide (Milk of Magnesia) are another reasonable option. These agents draw water into the intestinal lumen, softening stool and promoting bowel movements. Polyethylene glycol is particularly well-tolerated and does not typically cause electrolyte disturbances when used as directed. While effective, patients should follow OTC labeling (generally limiting use to 7 days unless directed by a healthcare provider). Magnesium-containing products should be avoided in patients with kidney disease due to the risk of hypermagnesemia, particularly in older adults.
Stool softeners such as docusate sodium (Colace) have limited evidence for effectiveness. They work by allowing water and fats to penetrate the stool, making it easier to pass. While very safe, they are generally insufficient as monotherapy for semaglutide-related constipation.
Stimulant laxatives like bisacodyl (Dulcolax) and senna are effective for short-term or occasional use. According to recent American Gastroenterological Association guidelines, stimulant laxatives can be appropriate for rescue therapy when other methods fail. Patients should follow package directions regarding duration of use and consult their healthcare provider for ongoing needs. For some patients, rectal options like glycerin or bisacodyl suppositories may provide more predictable, localized relief for occasional constipation.
Non-pharmacological approaches should be the foundation of constipation management for patients taking semaglutide, with laxatives reserved for situations where lifestyle modifications prove insufficient. Adequate hydration is important—patients should maintain fluid intake sufficient to produce pale yellow urine. Individual needs vary based on activity level, climate, and other factors. The appetite suppression caused by semaglutide may reduce thirst cues, so conscious attention to fluid intake becomes especially important.
Dietary fiber intake should be gradually increased to 25-35 grams daily through whole grains, fruits, vegetables, legumes, and nuts, in line with the Dietary Guidelines for Americans. Sudden increases in fiber without adequate hydration can worsen constipation, so incremental adjustments over 1-2 weeks are advisable. Foods particularly helpful for promoting regularity include prunes, kiwifruit, flaxseeds, and leafy greens. Patients should be counseled that while semaglutide reduces appetite, maintaining adequate nutritional intake—including fiber-rich foods—remains important for overall health and bowel function.
Regular physical activity stimulates intestinal motility and can significantly improve constipation. Even moderate exercise such as 20-30 minutes of daily walking can be beneficial. The American College of Gastroenterology recommends regular physical activity as part of comprehensive constipation management.
Establishing consistent bowel habits helps train the digestive system. Patients should attempt bowel movements at the same time daily, ideally after meals when the gastrocolic reflex naturally stimulates colonic activity. Allowing adequate time without rushing and responding promptly to the urge to defecate are important behavioral strategies.
Patients should adhere to the prescribed dose escalation schedule for semaglutide, as this is designed to improve GI tolerability. If constipation or other GI symptoms are severe or persistent despite these measures, patients should discuss potential dose adjustments with their healthcare provider rather than modifying the regimen independently.
While mild constipation on semaglutide can often be managed with over-the-counter measures, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if constipation persists for more than one week despite lifestyle modifications and appropriate laxative use, as this may indicate inadequate treatment or an underlying condition requiring investigation.
Severe abdominal pain, particularly if accompanied by distension, vomiting, or inability to pass gas, requires urgent medical attention. These symptoms could indicate bowel obstruction or ileus, which have been reported in postmarketing surveillance of semaglutide. Similarly, rectal bleeding or black, tarry stools should never be attributed to constipation alone and necessitate prompt evaluation to rule out gastrointestinal bleeding or other pathology.
Patients experiencing unintentional weight loss beyond expected therapeutic effects, fever, or night sweats alongside digestive symptoms should seek medical assessment, as these may suggest conditions unrelated to semaglutide. Persistent nausea and vomiting that prevents adequate oral intake or leads to dehydration requires medical intervention, as this may indicate gastroparesis or other complications requiring dose adjustment or alternative management strategies.
New or worsening symptoms after months of stable semaglutide therapy should also prompt evaluation, as these may not be medication-related. New-onset constipation in patients over age 50 or accompanied by iron-deficiency anemia warrants evaluation to rule out colorectal pathology, per gastroenterology guidelines.
Additionally, patients should inform their healthcare provider if they find themselves requiring daily laxative use for extended periods, as this may indicate the need for prescription medications, dose adjustment of semaglutide, or further diagnostic evaluation. Chronic constipation requiring ongoing intervention deserves comprehensive assessment rather than indefinite self-management. Healthcare providers can offer additional strategies including prescription medications, referral to gastroenterology if indicated, or consideration of alternative diabetes or weight management therapies if gastrointestinal side effects significantly impair quality of life.
Bulk-forming laxatives such as psyllium (Metamucil) and osmotic laxatives like polyethylene glycol (MiraLAX) are generally the safest first-line options. These work gently by increasing stool bulk or drawing water into the intestines, and are less likely to cause cramping or electrolyte disturbances when used as directed with adequate fluid intake.
Constipation often emerges during dose escalation periods and may improve after completing the titration schedule. Some patients experience persistent symptoms that require ongoing management through lifestyle modifications, dietary changes, or occasional laxative use under healthcare provider guidance.
Contact your healthcare provider if constipation persists for more than one week despite treatment, if you experience severe abdominal pain or distension, rectal bleeding, persistent vomiting, or if you require daily laxative use for extended periods. These symptoms may indicate complications requiring medical evaluation or treatment adjustment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.