LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 receptor agonists have emerged as powerful tools in managing obesity and type 2 diabetes, but do GLP-1 reduce visceral fat specifically? Visceral fat—the metabolically active adipose tissue surrounding internal organs—poses greater health risks than subcutaneous fat, driving insulin resistance, cardiovascular disease, and metabolic dysfunction. Clinical trials using imaging techniques demonstrate that GLP-1 medications significantly reduce visceral adipose tissue alongside overall weight loss. This article examines the evidence for visceral fat reduction with GLP-1 therapy, the mechanisms involved, and clinical implications for patients with central obesity and cardiometabolic disease.
Quick Answer: Yes, GLP-1 receptor agonists effectively reduce visceral fat, as demonstrated by clinical trials using CT and MRI imaging showing significant decreases in visceral adipose tissue volume alongside improvements in waist circumference and cardiometabolic markers.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Visceral fat refers to adipose tissue stored deep within the abdominal cavity, surrounding vital organs including the liver, pancreas, and intestines. Unlike subcutaneous fat, which lies directly beneath the skin and can be pinched, visceral fat is not visible from the outside but poses significantly greater health risks.
This type of fat is metabolically active, releasing inflammatory cytokines and free fatty acids directly into the portal circulation. These substances contribute to insulin resistance, dyslipidemia, and systemic inflammation—key drivers of type 2 diabetes, cardiovascular disease, and metabolic dysfunction-associated steatotic liver disease (MASLD, formerly known as NAFLD). Excess visceral adiposity is strongly associated with increased risk of cardiovascular events and all-cause mortality, even after accounting for body mass index (BMI).
Clinically, visceral fat accumulation is often assessed through waist circumference measurements, with values exceeding 40 inches (102 cm) in men and 35 inches (88 cm) in women indicating increased cardiometabolic risk according to the American Heart Association/National Heart, Lung, and Blood Institute criteria. These thresholds may vary by ethnicity, with lower cutoffs for certain populations, particularly those of Asian descent. More precise quantification can be achieved through imaging modalities such as magnetic resonance imaging (MRI) or computed tomography (CT), though these are typically reserved for research settings or specific clinical indications due to cost and, in the case of CT, radiation exposure.
The preferential accumulation of visceral fat is influenced by genetics, hormonal factors (particularly cortisol and sex hormones), dietary patterns, physical inactivity, and aging. Reducing visceral adiposity has been shown to improve insulin sensitivity, lipid profiles, and inflammatory markers, making it a critical therapeutic target in metabolic disease management.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of endogenous GLP-1, an incretin hormone secreted by intestinal L-cells in response to nutrient intake. These agents bind to GLP-1 receptors expressed throughout the body, including pancreatic beta cells, the gastrointestinal tract, and central nervous system regions involved in appetite regulation.
Centrally, GLP-1 receptor activation in hypothalamic and brainstem nuclei reduces appetite and food intake. This effect appears to involve modulation of reward pathways and satiety signaling, leading to decreased caloric consumption. The combination of reduced appetite, delayed gastric emptying, and improved glucose metabolism results in significant weight loss in many patients.
Currently available GLP-1 receptor agonists include shorter-acting formulations such as exenatide (administered twice daily), daily options like liraglutide, and longer-acting agents like semaglutide and dulaglutide (weekly injections). Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, not a pure GLP-1 agonist. Oral semaglutide (Rybelsus) represents the first oral GLP-1 formulation but is FDA-approved only for type 2 diabetes, not weight management.
Common adverse effects include nausea, vomiting, diarrhea, and constipation, typically most pronounced during dose titration. These gastrointestinal effects can lead to dehydration and acute kidney injury in some patients. Rare but serious risks include pancreatitis (requiring immediate medical attention if severe abdominal pain occurs), gallbladder disease, and potential thyroid C-cell tumors (based on rodent studies). Semaglutide carries a specific warning about potential worsening of diabetic retinopathy in patients with pre-existing disease. These medications are contraindicated during pregnancy and should be discontinued before planned conception. Careful patient selection, monitoring, and gradual dose titration are essential for safe use.
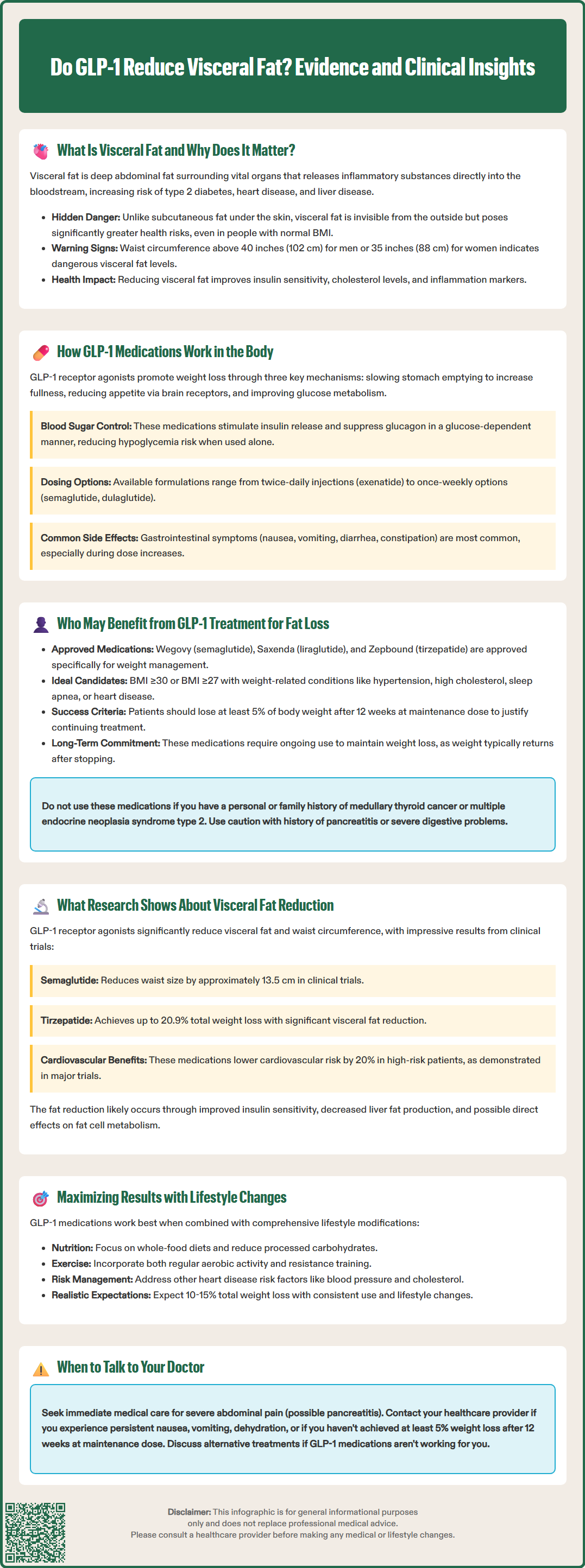
GLP-1 receptor agonists are FDA-approved for two primary indications: type 2 diabetes management and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. For weight management specifically, semaglutide (Wegovy®, also approved for adolescents ≥12 years), liraglutide 3 mg (Saxenda®), and tirzepatide (Zepbound®) have received FDA approval. Other formulations like Ozempic, Mounjaro, and Rybelsus are approved for diabetes but not specifically for weight management.
Patients most likely to benefit from GLP-1 therapy for fat reduction include those with a BMI of 30 kg/m² or greater, or a BMI of 27 kg/m² or greater with weight-related conditions such as hypertension, dyslipidemia, obstructive sleep apnea, or cardiovascular disease. Individuals with type 2 diabetes and concurrent obesity represent an ideal population, as these medications address both hyperglycemia and excess adiposity. Those with evidence of central obesity and elevated waist circumference may particularly benefit given the metabolic risks associated with visceral fat accumulation, though this is not an FDA-labeled selection criterion.
Clinicians should consider GLP-1 therapy when lifestyle modifications—including dietary changes and increased physical activity—have proven insufficient to achieve weight loss goals. The American Diabetes Association supports the use of GLP-1 receptor agonists as part of comprehensive diabetes management, particularly in patients requiring weight reduction.
Contraindications include personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Caution is warranted in patients with a history of pancreatitis, severe gastrointestinal disease including gastroparesis, or diabetic retinopathy. According to obesity treatment guidelines, patients should demonstrate approximately 5% weight loss after 12 weeks at the maintenance dose to continue therapy. Patients should be counseled about the need for ongoing treatment, as weight regain commonly occurs upon discontinuation. Realistic expectations regarding weight loss magnitude (typically 10-15% of body weight with higher-dose formulations) and the importance of concurrent lifestyle modification should be established before initiating therapy.
Evidence suggests that GLP-1 receptor agonists can effectively reduce visceral adipose tissue, though the degree to which this reduction is preferential compared to subcutaneous fat continues to be investigated. Several clinical trials utilizing imaging-based assessments have demonstrated significant reductions in visceral fat volume among patients treated with GLP-1 agonists.
Studies published in Diabetes Care have examined patients with type 2 diabetes treated with liraglutide, demonstrating reductions in visceral adipose tissue measured by CT scan compared to placebo. Similarly, trials of semaglutide have shown substantial reductions in waist circumference—a clinical surrogate for visceral adiposity—alongside improvements in cardiometabolic markers including hemoglobin A1c, blood pressure, and lipid profiles.
The STEP 1 trial (published in the New England Journal of Medicine) documented mean weight reductions of 14.9% with once-weekly semaglutide 2.4 mg compared to 2.4% with placebo, with corresponding improvements in waist circumference of approximately 13.5 cm with semaglutide versus 4.1 cm with placebo after 68 weeks. The SURMOUNT-1 trial showed that tirzepatide, a dual GIP/GLP-1 receptor agonist, produced even greater weight loss (up to 20.9% at the highest dose) with proportional reductions in waist circumference.
The mechanisms underlying visceral fat reduction likely involve multiple pathways. Improved insulin sensitivity may reduce hepatic lipogenesis and visceral fat accumulation. Additionally, GLP-1 receptor activation may influence adipocyte metabolism and lipolysis, though direct effects on adipose tissue remain an area of active investigation.
Importantly, the clinical benefits of GLP-1 therapy extend beyond fat loss alone. Cardiovascular outcomes trials have demonstrated reduced rates of major adverse cardiovascular events in high-risk patients treated with liraglutide (LEADER trial) and semaglutide (SUSTAIN-6 trial). More recently, the SELECT trial showed that semaglutide 2.4 mg reduced cardiovascular events by 20% in patients with established cardiovascular disease and overweight/obesity without diabetes. While these cardiovascular benefits may be related to multiple mechanisms, including weight loss, the specific contribution of visceral fat reduction has not been definitively established.
Clinicians should recognize that while GLP-1 receptor agonists effectively reduce visceral fat, they represent one component of comprehensive metabolic disease management. Optimal outcomes require integration with dietary modification emphasizing whole foods and reduced processed carbohydrate intake, regular physical activity including both aerobic and resistance training, and management of other cardiovascular risk factors. Patients should be monitored for treatment response through serial measurements of weight, waist circumference, glycemic parameters, and lipid profiles. According to obesity treatment guidelines, patients should demonstrate approximately 5% weight loss after 12 weeks at the maintenance dose to continue therapy. Those not meeting this threshold may require alternative or adjunctive interventions. Referral to endocrinology or obesity medicine specialists should be considered for complex cases or when treatment goals are not achieved with standard approaches.
Clinical trials show GLP-1 receptor agonists reduce waist circumference by approximately 13.5 cm with semaglutide after 68 weeks, with imaging studies demonstrating significant decreases in visceral adipose tissue volume. The reduction correlates with overall weight loss, typically 10-15% of body weight with higher-dose formulations.
Research shows GLP-1 receptor agonists effectively reduce visceral fat, though whether this reduction is preferential compared to subcutaneous fat continues to be investigated. Clinical benefits include improved insulin sensitivity, lipid profiles, and cardiovascular outcomes associated with visceral fat reduction.
FDA-approved candidates include adults with BMI ≥30 kg/m² or BMI ≥27 kg/m² with weight-related comorbidities such as hypertension, dyslipidemia, or cardiovascular disease. Patients with type 2 diabetes and central obesity particularly benefit, though contraindications include personal or family history of medullary thyroid carcinoma.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.