LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do GLP-1 medications speed up metabolism? This common question reflects widespread interest in how drugs like Ozempic, Wegovy, and Mounjaro facilitate weight loss. Contrary to popular belief, GLP-1 receptor agonists do not function as metabolic stimulants or significantly increase resting metabolic rate. Instead, these FDA-approved medications work primarily by reducing appetite, slowing gastric emptying, and decreasing caloric intake. Understanding the actual mechanisms behind GLP-1 therapy helps patients and clinicians set realistic expectations for treatment outcomes and recognize that successful weight management with these agents requires active participation in dietary modifications alongside medication use.
Quick Answer: GLP-1 receptor agonists do not significantly speed up metabolism or increase resting metabolic rate.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications that mimic the action of naturally occurring GLP-1, an incretin hormone produced in the intestinal L-cells. These medications—including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—bind to GLP-1 receptors distributed throughout multiple organ systems, triggering a cascade of metabolic effects. Tirzepatide (Mounjaro, Zepbound) works similarly but is classified as a dual GIP/GLP-1 receptor agonist.
The primary mechanism involves glucose-dependent insulin secretion from pancreatic beta cells. When blood glucose levels rise after eating, these medications enhance insulin release while simultaneously suppressing glucagon secretion from alpha cells. This dual action helps normalize blood glucose with lower risk of hypoglycemia compared to some older diabetes medications, though the risk increases when combined with insulin or sulfonylureas. The FDA has approved these agents for type 2 diabetes management (not type 1 diabetes or diabetic ketoacidosis), with select formulations also approved for chronic weight management in adults with obesity or overweight with weight-related comorbidities.
Beyond pancreatic effects, these medications significantly slow gastric emptying, which prolongs the sensation of fullness after meals. This effect may diminish over time with continued use and requires caution in patients with severe gastrointestinal disease or gastroparesis. They also act on receptors in the central nervous system, particularly in hypothalamic regions that regulate appetite and satiety. These neurological effects reduce hunger signals and food cravings, contributing substantially to the weight loss observed in clinical trials. The medications do not directly target metabolic rate or thermogenesis as their primary mechanism, which distinguishes them from stimulant-based weight loss agents. Understanding this distinction is essential for setting appropriate patient expectations regarding how these medications facilitate weight reduction.
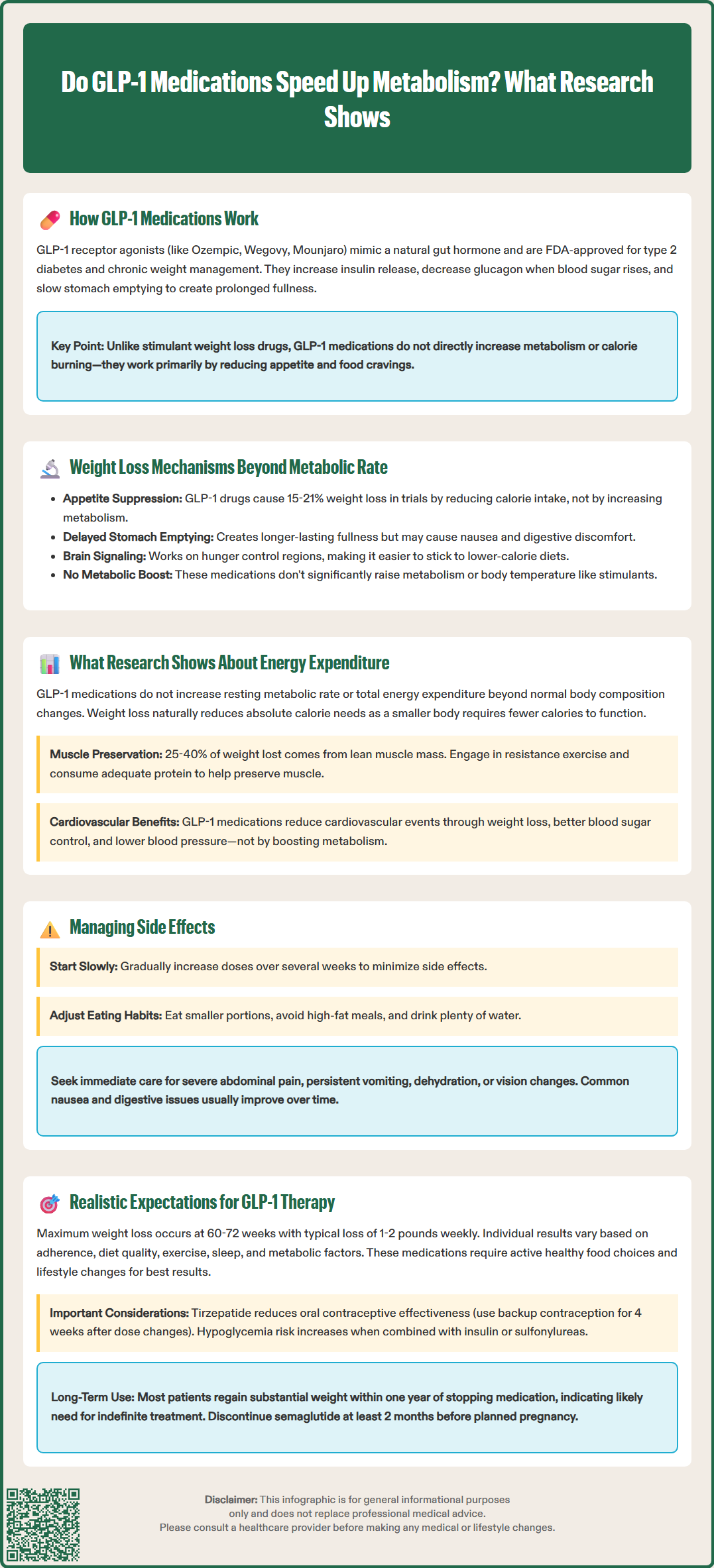
The substantial weight loss achieved with GLP-1 receptor agonists and dual GIP/GLP-1 agonists—approximately 15% with semaglutide 2.4 mg (Wegovy) and up to 21% with higher doses of tirzepatide (Zepbound) in clinical trials—occurs primarily through appetite suppression and reduced caloric intake rather than increased metabolic rate. Patients consistently report decreased hunger, earlier satiety during meals, and reduced preoccupation with food. These subjective changes translate to measurable reductions in daily caloric consumption, which can vary considerably between individuals.
The delayed gastric emptying induced by these medications creates a mechanical component to satiety. Food remains in the stomach longer, triggering stretch receptors that signal fullness to the brain. This effect can occasionally cause gastrointestinal adverse effects—nausea, vomiting, and abdominal discomfort—particularly during dose escalation. The FDA-approved prescribing information recommends gradual dose titration over several weeks to minimize these symptoms. Patients should be counseled to eat smaller portions, avoid high-fat meals, and stay adequately hydrated.
Central nervous system effects represent another critical mechanism. GLP-1 receptors in the hypothalamus, brainstem, and reward pathways modulate eating behavior at multiple levels. Research demonstrates reduced activation in brain regions associated with food reward when patients view images of palatable foods. This neurobiological change helps explain why patients find it easier to adhere to reduced-calorie diets while taking these medications.
Unlike stimulant-based weight loss medications, GLP-1 and dual GIP/GLP-1 agonists do not function primarily as metabolic stimulants or thermogenic agents. While they may cause modest increases in heart rate (typically 2-4 beats per minute) and modest decreases in blood pressure, they do not significantly raise core body temperature or substantially accelerate metabolic rate. This cardiovascular profile has been extensively studied, with certain agents (liraglutide, semaglutide, dulaglutide) demonstrating cardiovascular outcome benefits in patients with established cardiovascular disease or multiple risk factors.
Clinical studies examining the effects of GLP-1 receptor agonists on resting metabolic rate (RMR) and total energy expenditure have produced consistent findings: these medications do not significantly increase metabolic rate. Multiple controlled trials using indirect calorimetry—the gold standard for measuring energy expenditure—have demonstrated that GLP-1 therapy does not elevate RMR beyond what would be expected from changes in body composition.
A critical consideration in interpreting metabolism studies is that substantial weight loss from any method typically results in decreased absolute energy expenditure. As body mass declines, fewer calories are required to maintain basic physiological functions and support daily activities. Research indicates that GLP-1-associated weight loss follows this expected pattern. When adjusted for changes in lean body mass and fat mass, metabolic rate remains proportional to body composition. There is no evidence of metabolic acceleration that would offset the natural decline in energy requirements accompanying weight reduction.
Some studies have examined whether GLP-1 medications might preserve lean muscle mass during weight loss, which could theoretically maintain higher metabolic rates. The data suggest that GLP-1-induced weight loss includes both fat mass and lean mass reduction, with approximately 25-40% of total weight loss coming from lean tissue. This proportion is comparable to or slightly better than that observed with caloric restriction alone, but it underscores the importance of resistance exercise and adequate protein intake during treatment. Clinical nutrition guidelines recommend that patients on weight loss therapy engage in regular physical activity and consume sufficient protein to help preserve muscle mass.
Cardiovascular outcome trials (including LEADER, SUSTAIN-6, REWIND, and SELECT) have demonstrated that certain GLP-1 receptor agonists reduce major adverse cardiovascular events in patients with established cardiovascular disease or multiple risk factors. These benefits appear to result from weight loss, improved glycemic control, modest blood pressure reduction, and potential direct cardioprotective effects—not from metabolic rate enhancement.
Patients considering GLP-1 receptor agonist or dual GIP/GLP-1 therapy should understand that these medications facilitate weight loss through appetite reduction and decreased food intake, not by "speeding up metabolism" or burning additional calories at rest. This mechanism requires active patient participation: the medication reduces hunger and makes dietary adherence easier, but patients must still make conscious food choices and maintain lifestyle modifications for optimal results.
Clinical trial data from the STEP and SURMOUNT programs demonstrate that maximum weight loss typically occurs between 60-72 weeks of treatment, with most patients losing 1-2 pounds per week during the active weight loss phase. Individual responses vary considerably, with some patients achieving dramatic results while others experience more modest weight reduction. Factors influencing response include baseline body weight, adherence to therapy, dietary quality, physical activity levels, sleep patterns, and metabolic factors. Patients should be counseled that weight loss plateaus are normal and do not indicate medication failure.
Adverse effects require careful monitoring and patient education. The most common side effects—nausea, diarrhea, constipation, and abdominal pain—are generally mild to moderate and improve with continued treatment. However, serious adverse effects can occur, including pancreatitis (severe persistent abdominal pain), gallbladder disease, and acute kidney injury (typically related to dehydration from gastrointestinal symptoms). Patients should seek immediate medical attention for severe abdominal pain, persistent vomiting, signs of dehydration, or vision changes (particularly with semaglutide, which carries a diabetic retinopathy warning). The risk of hypoglycemia increases when these medications are combined with insulin or sulfonylureas, often requiring dose adjustments of these agents. Tirzepatide can reduce oral contraceptive effectiveness, necessitating backup contraception for 4 weeks after starting or increasing doses.
Long-term success with these therapies requires ongoing treatment in most cases. Discontinuation studies show that patients typically regain a substantial portion of lost weight within one year of stopping medication, accompanied by return of appetite and metabolic parameters toward baseline. This pattern reflects the chronic nature of obesity as a disease and suggests that therapy may need to be continued indefinitely for sustained weight management. Healthcare providers should discuss this likelihood during shared decision-making conversations, along with considerations of cost, insurance coverage, medication availability, and perioperative management (as these agents delay gastric emptying). For patients planning pregnancy, medications like semaglutide should be discontinued at least 2 months before planned conception. Combining therapy with behavioral interventions, nutritional counseling, and regular physical activity optimizes outcomes and may help patients maintain weight loss if medication discontinuation becomes necessary.
GLP-1 receptor agonists cause weight loss primarily by suppressing appetite, slowing gastric emptying to increase fullness, and acting on brain regions that regulate hunger and food cravings. These effects lead to reduced caloric intake rather than increased calorie burning through metabolic acceleration.
Metabolic rate typically decreases proportionally as body mass declines during GLP-1 therapy, following the same pattern as weight loss from other methods. Clinical studies show no evidence of metabolic acceleration that would offset the natural decline in energy requirements accompanying weight reduction.
Most patients regain a substantial portion of lost weight within one year of discontinuing GLP-1 therapy, as appetite and metabolic parameters return toward baseline. This reflects obesity's chronic nature and suggests that ongoing treatment may be necessary for sustained weight management in many individuals.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.