LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Weight loss injections like semaglutide (Wegovy) and tirzepatide (Zepbound) have become increasingly popular for chronic weight management, but many patients wonder about their side effects. Nausea and digestive discomfort are among the most common concerns with these medications. Clinical trials show that approximately 44% of patients using semaglutide experience nausea, along with other gastrointestinal symptoms. Understanding why these injections can make you feel sick—and how to manage these effects—is essential for anyone considering or currently using these FDA-approved treatments for obesity and weight-related health conditions.
Quick Answer: Weight loss injections commonly cause nausea and digestive discomfort, with approximately 44% of semaglutide users and 25-33% of tirzepatide users experiencing nausea in clinical trials.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections work by mimicking natural hormones that regulate appetite and blood sugar. The two main types are glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Wegovy) and dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonists such as tirzepatide (Zepbound).
These medications bind to receptors throughout the body, including the brain, pancreas, and gastrointestinal tract. In the brain, they act on appetite centers in the hypothalamus, reducing hunger signals and increasing feelings of fullness. In the pancreas, they stimulate insulin secretion when blood glucose levels are elevated and suppress glucagon release, helping to stabilize blood sugar. Importantly, these medications significantly slow gastric emptying—the rate at which food moves from the stomach into the small intestine—though this effect may attenuate somewhat with continued use.
This delayed gastric emptying is central to both the therapeutic effect and the side effect profile of these injections. By keeping food in the stomach longer, patients experience prolonged satiety and reduced appetite, which contributes to weight loss. Clinical trials have demonstrated that patients using semaglutide 2.4 mg weekly can achieve average weight loss of approximately 15% of body weight over 68 weeks when combined with lifestyle modifications.
The FDA has approved Wegovy (semaglutide) and Zepbound (tirzepatide) specifically for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity such as hypertension, type 2 diabetes, or dyslipidemia. Note that Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved only for type 2 diabetes management, though they contain the same active ingredients. Understanding how these medications work helps explain why gastrointestinal side effects are so common during treatment.
Nausea is the most frequently reported side effect of weight loss injections. In clinical trials of semaglutide 2.4 mg for weight management (STEP 1), approximately 44% of participants experienced nausea, compared to about 16% in placebo groups. For tirzepatide in the SURMOUNT-1 trial, nausea rates ranged from 25-33% depending on the dose, with higher doses associated with increased incidence.
Beyond nausea, patients commonly experience a constellation of gastrointestinal symptoms including:
Vomiting (reported in 24% of semaglutide users)
Diarrhea (affecting 30% of patients)
Constipation (occurring in 24% of users)
Abdominal pain or discomfort (experienced by 20% of patients)
Bloating and excessive gas
Acid reflux or heartburn
Decreased appetite (which, while therapeutic, can feel uncomfortable)
The severity of these symptoms typically ranges from mild to moderate, and most patients do not discontinue treatment due to nausea alone. However, in clinical trials, approximately 4-7% of participants stopped taking semaglutide due to gastrointestinal adverse effects. The timing of these symptoms is important: nausea and digestive issues are most pronounced during the initial weeks of treatment and following dose escalations.
Many patients report that gastrointestinal symptoms tend to improve over time as the body adapts to the medication. These side effects often follow a pattern, with symptoms frequently occurring after injections and during dose increases. Understanding this pattern helps patients anticipate and manage symptoms more effectively, reducing anxiety about the treatment experience.
Weight loss with these medications is also associated with an increased risk of gallbladder problems, including gallstones, which can cause additional digestive symptoms.
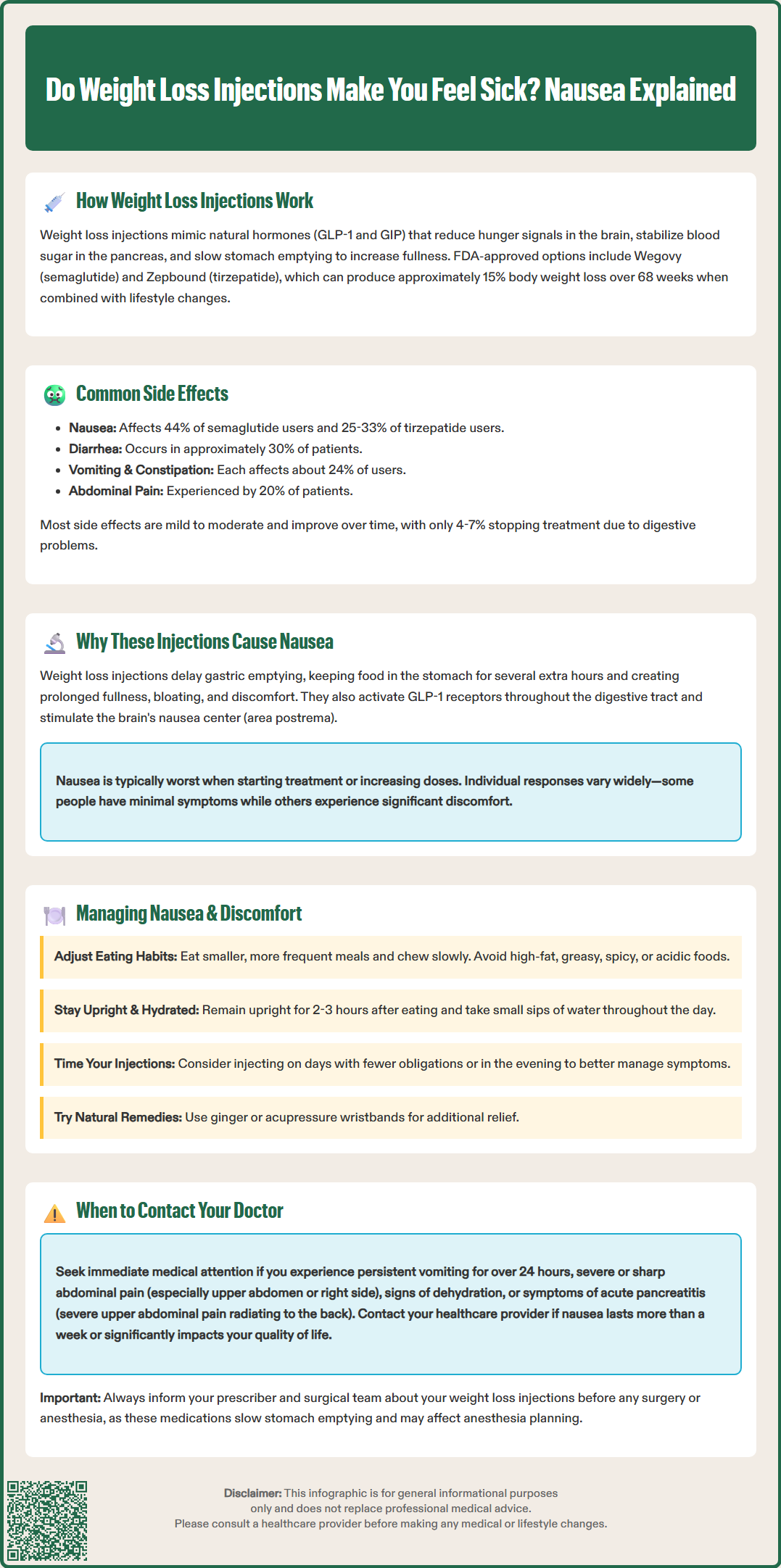
The nausea and digestive discomfort associated with weight loss injections stem directly from their pharmacological mechanism. The primary culprit is delayed gastric emptying—food remains in the stomach significantly longer than normal, sometimes for several additional hours. This prolonged retention can create sensations of fullness, bloating, and nausea, particularly after eating. This effect is typically most pronounced during initial treatment and may diminish somewhat with continued use.
GLP-1 receptors are densely distributed throughout the gastrointestinal tract, and when activated by these medications, they affect multiple aspects of digestive function. The slowed movement of food through the digestive system can lead to feelings of excessive fullness (early satiety), discomfort, and in some cases, nausea that persists between meals. Additionally, these medications affect the area postrema in the brainstem—a region involved in triggering nausea and vomiting responses.
Dose-dependent effects play a significant role in symptom severity. Weight loss injections are typically initiated at low doses and gradually increased over several weeks or months according to FDA-approved product labeling. This titration schedule aims to minimize side effects while allowing the body to adapt. However, each dose increase can trigger a recurrence of nausea and digestive symptoms.
Individual variation in response is considerable. Some patients experience minimal discomfort, while others find the nausea significantly impacts their quality of life. Factors that may influence susceptibility include baseline gastrointestinal sensitivity, history of motion sickness or migraine, concurrent medications, and dietary habits. There is no definitive way to predict who will experience more severe symptoms. According to FDA labeling, these medications are not recommended for patients with severe gastrointestinal disease, including severe gastroparesis, as they may worsen symptoms.
Effective management strategies can significantly reduce nausea and improve tolerability of weight loss injections. Dietary modifications are the cornerstone of symptom management. Patients should focus on eating smaller, more frequent meals rather than three large meals daily. Portion sizes should be reduced, as the delayed gastric emptying means less food is needed to achieve fullness.
Dietary recommendations include:
Eating slowly and chewing food thoroughly
Avoiding high-fat, greasy, or fried foods that delay gastric emptying further
Limiting spicy, acidic, or heavily seasoned foods that may irritate the stomach
Staying well-hydrated with small sips of water throughout the day
Avoiding lying down immediately after eating (remain upright for 2-3 hours)
Choosing bland, easily digestible foods during periods of increased nausea
Limiting alcohol and caffeine, which can exacerbate symptoms
For constipation, increasing fiber intake gradually, ensuring adequate hydration, and occasionally using osmotic laxatives or stool softeners may help. For diarrhea, avoiding trigger foods, replacing lost fluids and electrolytes, and judicious use of over-the-counter anti-diarrheal medications (after consulting a healthcare provider) can provide relief.
Timing considerations can also help. Some patients find that injecting the medication on a specific day of the week when they have fewer obligations allows them to rest if nausea occurs. Taking the injection in the evening rather than morning may help some individuals, though there is no official guidance suggesting one time is superior.
Non-pharmacological approaches such as ginger (in tea, capsules, or candies) and acupressure wristbands may provide relief for some patients, though evidence for these specific to GLP-1 medications is limited. Staying in well-ventilated areas and avoiding strong odors can prevent triggering nausea.
If symptoms persist despite these measures, healthcare providers may recommend anti-nausea medications such as ondansetron or metoclopramide for short-term use, though these should only be taken under medical supervision. Slowing the dose escalation schedule, temporarily returning to a lower dose, or holding at the current dose longer than recommended are options that can improve tolerability while still achieving therapeutic benefits.
For patients taking tirzepatide (Zepbound) who also use oral contraceptives, it's important to note that during dose escalation, exposure to oral contraceptives may be reduced. Additional contraceptive methods are recommended during this period.
While nausea and digestive discomfort are expected side effects of weight loss injections, certain symptoms warrant immediate medical attention. Patients should contact their healthcare provider promptly if they experience persistent vomiting that prevents them from keeping down food or fluids for more than 24 hours, as this can lead to dehydration and electrolyte imbalances.
Seek medical evaluation for:
Severe abdominal pain, particularly if sharp, persistent, or localized to the upper abdomen or right side, which could indicate pancreatitis or gallbladder disease
Signs of dehydration including decreased urination, dark urine, dizziness, rapid heartbeat, or extreme thirst
Symptoms of hypoglycemia such as sweating, shakiness, confusion, irritability, dizziness, or blurred vision (risk is low with these medications alone but increases when combined with insulin or sulfonylureas)
Persistent nausea lasting more than a week despite dietary modifications
Inability to tolerate any food or liquids
Symptoms of gastroparesis such as severe bloating, early satiety with very small amounts of food, or vomiting undigested food hours after eating
Signs of gallbladder problems including right upper quadrant pain, fever, or yellowing of the skin or eyes (jaundice)
Rare but serious complications require emergency care. Acute pancreatitis, though rare, presents with severe upper abdominal pain radiating to the back, often accompanied by nausea and vomiting. Symptoms of bowel obstruction or ileus—severe cramping, inability to pass gas or stool, and progressive abdominal distension—require immediate evaluation.
Patients should also inform their healthcare provider if side effects significantly impact quality of life or ability to function, even if not medically dangerous. Dose adjustments, slower titration schedules, or switching to alternative medications may be appropriate. Regular follow-up appointments allow providers to monitor weight loss progress, assess tolerability, and adjust treatment plans accordingly. Open communication about symptom severity helps optimize both safety and effectiveness of weight loss injection therapy.
If scheduled for surgery or procedures requiring anesthesia, patients should discuss their medication with both their prescriber and surgical team, as delayed gastric emptying may affect anesthesia planning.
Nausea is typically most pronounced during the first few weeks of treatment and following dose increases, with symptoms often improving as the body adapts to the medication. Most patients experience reduced nausea over time, though individual responses vary considerably.
While nausea cannot always be completely prevented, eating smaller and more frequent meals, avoiding high-fat and greasy foods, staying well-hydrated, and following a gradual dose escalation schedule can significantly reduce symptoms and improve tolerability.
Contact your healthcare provider if you experience persistent vomiting for more than 24 hours, severe abdominal pain, signs of dehydration, or if nausea significantly impacts your quality of life. Your provider may adjust your dose, slow titration, or recommend alternative treatments rather than stopping abruptly.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.