LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and weight management. While highly effective, many patients wonder: does semaglutide make you bloated? Understanding this common side effect is essential for setting realistic expectations and managing symptoms effectively. Semaglutide works by slowing gastric emptying, which improves blood sugar control and reduces appetite but can also cause gastrointestinal effects including bloating. This article examines the relationship between semaglutide and bloating, explains why it occurs, and provides evidence-based strategies for symptom management.
Quick Answer: Semaglutide can cause bloating due to its mechanism of slowing gastric emptying, which is a recognized adverse reaction listed in FDA prescribing information.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand names Ozempic and Rybelsus) and chronic weight management (as Wegovy). This medication works by mimicking the action of naturally occurring GLP-1, a hormone that regulates blood glucose levels by stimulating insulin secretion, suppressing glucagon release, and slowing gastric emptying.
The mechanism of delayed gastric emptying—while therapeutically beneficial for glycemic control and appetite reduction—directly affects the gastrointestinal tract and is responsible for many of the digestive side effects associated with semaglutide. According to FDA prescribing information, gastrointestinal adverse reactions are among the most commonly reported side effects across all semaglutide formulations.
Clinical trials, including the SUSTAIN and STEP programs, have documented that gastrointestinal symptoms occur in a substantial proportion of patients initiating semaglutide therapy. The most frequently reported digestive complaints include nausea (affecting approximately 15-44% of patients depending on dose and indication), vomiting, diarrhea, abdominal pain, and constipation. These effects are typically most pronounced during dose initiation and escalation, and tend to diminish over time as the body adapts to the medication.
It's important to note that semaglutide is not recommended for patients with severe gastrointestinal disease, including severe gastroparesis, as these conditions have not been studied in clinical trials and may be exacerbated by the medication's effects on gastric emptying.
Understanding the relationship between semaglutide's pharmacological action and its gastrointestinal effects is essential for both healthcare providers and patients. This knowledge helps set appropriate expectations, facilitates early recognition of side effects, and enables proactive management strategies that can improve treatment adherence and patient outcomes.
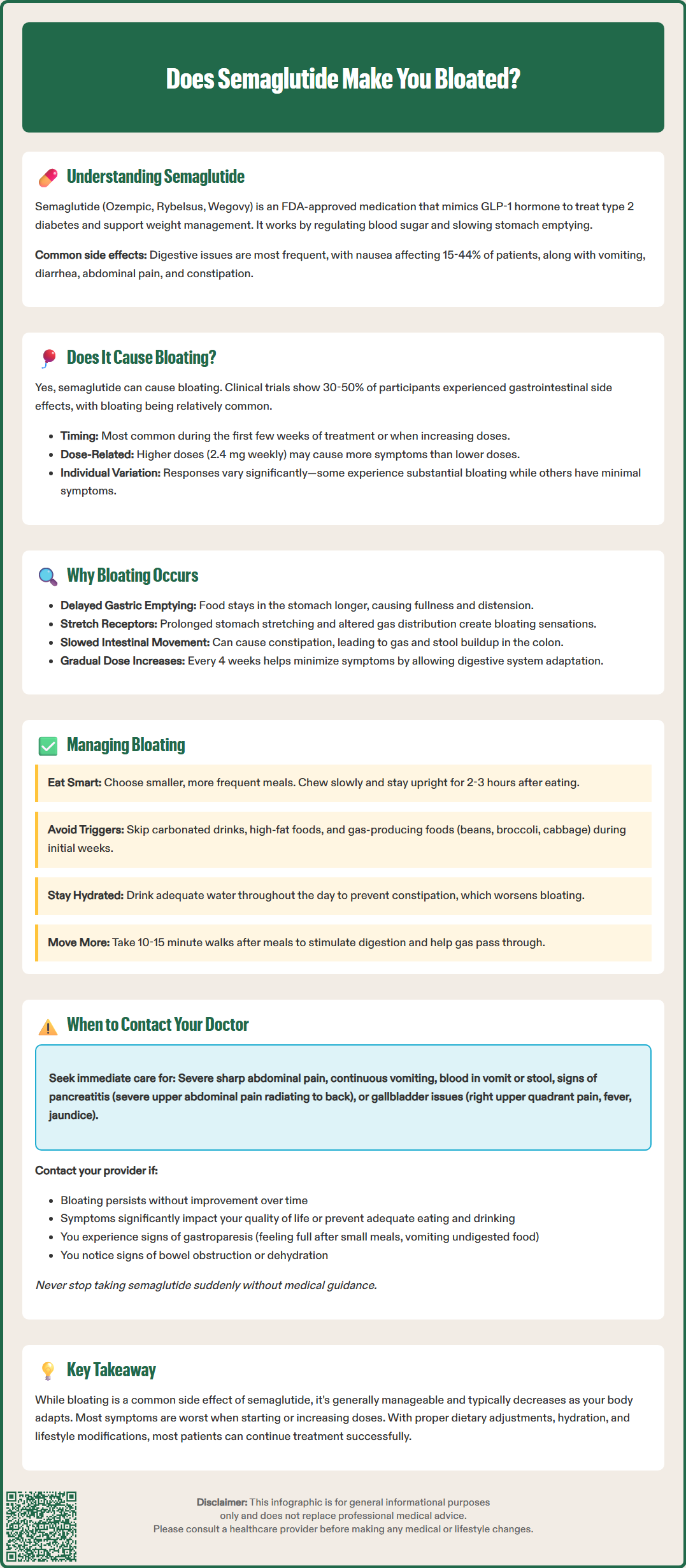
Yes, semaglutide can cause bloating. According to FDA prescribing information, abdominal distension (the medical term often used to describe bloating) is listed among the reported adverse reactions for semaglutide products. While not always separately quantified in clinical trial data, bloating—characterized by a sensation of abdominal fullness, distension, or tightness—is recognized as part of the broader spectrum of gastrointestinal side effects associated with GLP-1 receptor agonists.
In the SUSTAIN clinical trial program evaluating semaglutide for type 2 diabetes, gastrointestinal adverse events were reported by approximately 30-50% of participants, with the incidence varying by dose. Similarly, the STEP trials examining semaglutide for weight management documented comparable rates of digestive complaints. Patient reports and post-marketing surveillance data suggest that bloating is a relatively common experience, particularly during the initial weeks of treatment.
The incidence of bloating appears to be dose-dependent, with higher doses generally associated with increased gastrointestinal symptoms. Patients receiving the 2.4 mg weekly dose (Wegovy) for weight management may experience more pronounced digestive effects compared to those on lower doses used for diabetes management. However, individual susceptibility varies considerably, and some patients may experience significant bloating even at lower doses.
It is important to note that while bloating can be uncomfortable and may affect quality of life, it is generally considered a manageable side effect rather than a serious safety concern. Many patients find that symptoms improve over time as their digestive system adapts to the medication's effects on gastric motility, though the timeline for improvement varies among individuals.
The primary mechanism underlying bloating with semaglutide relates to its effect on gastric emptying. As a GLP-1 receptor agonist, semaglutide slows the rate at which food moves from the stomach into the small intestine. This delayed gastric emptying is therapeutically beneficial—it contributes to improved glycemic control and enhanced satiety—but it also means that food remains in the stomach for extended periods, potentially leading to sensations of fullness, distension, and bloating. It's worth noting that with continued use, some patients develop tolerance to this gastric-slowing effect (tachyphylaxis).
When gastric emptying is delayed, the stomach remains distended for longer after meals. This mechanical distension can trigger stretch receptors in the gastric wall, producing the uncomfortable sensation of bloating. Additionally, prolonged retention of food in the stomach may alter normal digestive processes, potentially affecting gas distribution within the gastrointestinal tract.
Semaglutide also affects gastrointestinal motility more broadly, not just gastric emptying. Changes in intestinal transit time can influence digestive processes. Some patients may experience constipation as a side effect of semaglutide, which can further contribute to bloating by causing accumulation of gas and stool in the colon.
Individual factors also play a significant role in determining who experiences bloating and to what degree. Patients with pre-existing gastrointestinal conditions may experience different responses to semaglutide, though specific susceptibility patterns have not been well-established in clinical studies. Dietary habits, eating patterns, and the rate of dose escalation can all influence the severity of bloating symptoms. The standard dose titration schedule—starting at a low dose and gradually increasing every 4 weeks—is specifically designed to minimize gastrointestinal side effects by allowing the digestive system time to adapt.
Importantly, the FDA labels for semaglutide products note that these medications have not been studied in patients with severe gastrointestinal disease, including severe gastroparesis, and are not recommended for use in these populations.
Several evidence-based strategies can help minimize bloating while taking semaglutide. Dietary modifications are often the most effective first-line approach. Patients should consider eating smaller, more frequent meals rather than large portions, as this reduces the volume of food in the stomach at any given time and may decrease the sensation of distension. Eating slowly and chewing food thoroughly can also help, as can avoiding lying down immediately after meals—remaining upright for at least 2-3 hours after eating allows gravity to assist with gastric emptying.
Specific foods and beverages may exacerbate bloating and should be limited or avoided, particularly during the initial weeks of treatment. These include:
Carbonated beverages, which introduce additional gas into the digestive system
High-fat foods, which further slow gastric emptying beyond semaglutide's effect
Foods that commonly produce gas, such as beans, lentils, cruciferous vegetables (broccoli, cabbage, Brussels sprouts), and certain artificial sweeteners
Large amounts of fiber introduced suddenly, though adequate fiber intake remains important for overall digestive health
Maintaining adequate hydration is essential, as it helps prevent constipation, which can worsen bloating. Most patients should aim for sufficient fluid intake throughout the day rather than consumed in large amounts at once. However, patients with conditions requiring fluid restriction (such as heart failure or advanced kidney disease) should follow their healthcare provider's specific guidance regarding fluid intake.
If constipation occurs alongside bloating, over-the-counter osmotic laxatives (such as polyethylene glycol) or stool softeners may be helpful, but should be discussed with your healthcare provider first.
Physical activity can significantly improve gastrointestinal motility and reduce bloating. Even gentle movement such as a 10-15 minute walk after meals can help stimulate digestion and gas passage. Regular exercise also supports overall treatment goals for both diabetes management and weight loss.
If bloating persists despite lifestyle modifications, discuss with your healthcare provider whether adjusting the dose escalation schedule might be appropriate. Some patients benefit from a slower titration, spending additional time at each dose level before increasing. Over-the-counter remedies such as simethicone may provide symptomatic relief for some patients, though evidence for their effectiveness is limited.
While mild to moderate bloating is a common and generally manageable side effect of semaglutide, certain symptoms warrant prompt medical evaluation. Contact your healthcare provider if you experience:
Severe or worsening abdominal pain, particularly if it is persistent, sharp, or localized to a specific area
Bloating accompanied by persistent vomiting, especially if you are unable to keep down fluids or medications
Signs of gastroparesis (severely delayed gastric emptying), including feeling full after eating only small amounts, persistent nausea, vomiting undigested food several hours after eating, or unintentional weight loss beyond expected therapeutic effects
Symptoms suggesting bowel obstruction or ileus, such as inability to pass gas or stool, severe abdominal distension, or cramping pain
Blood in vomit or stool, which could indicate gastrointestinal bleeding
Signs of pancreatitis, including severe, persistent upper abdominal pain that may radiate to the back, accompanied by nausea and vomiting
Right upper quadrant pain, fever, or yellowing of the skin or eyes, which could indicate gallbladder disease (cholelithiasis or cholecystitis), a known risk with GLP-1 receptor agonists
Signs of dehydration such as excessive thirst, dry mouth, dizziness, or decreased urination, which could lead to acute kidney injury if severe
Additionally, seek medical advice if bloating significantly impairs your quality of life or prevents you from maintaining adequate nutrition and hydration. Your healthcare provider can assess whether the symptoms represent expected side effects or indicate a more serious complication requiring intervention.
It is also important to discuss bloating with your provider if it persists without improvement despite continued treatment, as gastrointestinal side effects typically improve over time for many patients. Persistent symptoms may indicate the need for dose adjustment, additional diagnostic evaluation to rule out other gastrointestinal conditions, or consideration of alternative treatment options.
Never discontinue semaglutide abruptly without consulting your healthcare provider, as this could affect your diabetes control or weight management progress. If side effects are intolerable, your provider can work with you to develop an appropriate management plan, which might include temporary dose reduction, extended time at a lower dose, or transition to an alternative medication if necessary. The American Diabetes Association emphasizes the importance of individualized treatment approaches that balance therapeutic benefits with tolerability and patient preferences.
Bloating from semaglutide is typically most pronounced during the initial weeks of treatment and dose escalation periods. For many patients, symptoms improve over time as the digestive system adapts to the medication, though the timeline varies among individuals.
Over-the-counter remedies such as simethicone may provide symptomatic relief for some patients, though evidence for effectiveness is limited. If constipation contributes to bloating, osmotic laxatives or stool softeners may help, but you should discuss any over-the-counter medications with your healthcare provider first.
Never discontinue semaglutide abruptly without consulting your healthcare provider, as this could affect your diabetes control or weight management progress. If bloating is severe or accompanied by persistent vomiting, inability to pass gas, or severe abdominal pain, contact your provider immediately for evaluation and guidance.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.