LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does semaglutide show up in blood test results? This common question arises among patients using Ozempic, Wegovy, or Rybelsus for diabetes or weight management. Semaglutide, a GLP-1 receptor agonist, does not appear on standard blood tests like complete blood counts, metabolic panels, or lipid profiles. These routine laboratory tests are not designed to detect the medication itself. However, semaglutide can influence certain blood test results—including glucose, HbA1c, and lipid levels—due to its therapeutic effects. Understanding what semaglutide does and doesn't show on blood work helps patients and clinicians interpret laboratory results accurately and manage treatment effectively.
Quick Answer: Semaglutide does not appear on standard blood tests unless a specialized assay specifically designed to detect the medication is performed, which is uncommon in routine clinical practice.
Semaglutide, a glucagon-like peptide-1 (GLP-1) receptor agonist marketed as Ozempic, Wegovy, and Rybelsus, does not typically appear on standard blood tests ordered during routine medical care. Standard laboratory panels—including complete blood counts (CBC), basic metabolic panels (BMP), comprehensive metabolic panels (CMP), and lipid profiles—are not designed to detect or measure semaglutide levels. These tests evaluate blood cell counts, electrolytes, kidney and liver function, glucose, and cholesterol, none of which directly identify the presence of semaglutide in the bloodstream.
Semaglutide is a peptide medication administered subcutaneously (Ozempic, Wegovy) or orally (Rybelsus). While it circulates in the blood after administration, specialized assays would be required to detect the drug itself. Such tests are not part of routine clinical care and are uncommon outside research or specialized laboratory settings. According to FDA prescribing information, semaglutide has a half-life of approximately one week, meaning it remains in the system for several weeks after the last dose, but this persistence does not translate to detection on standard laboratory work.
Patients often wonder whether their use of semaglutide will be revealed through routine blood work ordered by their primary care physician or specialist. The straightforward answer is no—semaglutide will not show up unless a specific, targeted test for the medication is performed, which is uncommon in standard clinical practice. However, semaglutide can influence certain blood test results, which is an important distinction for patients and clinicians to understand.
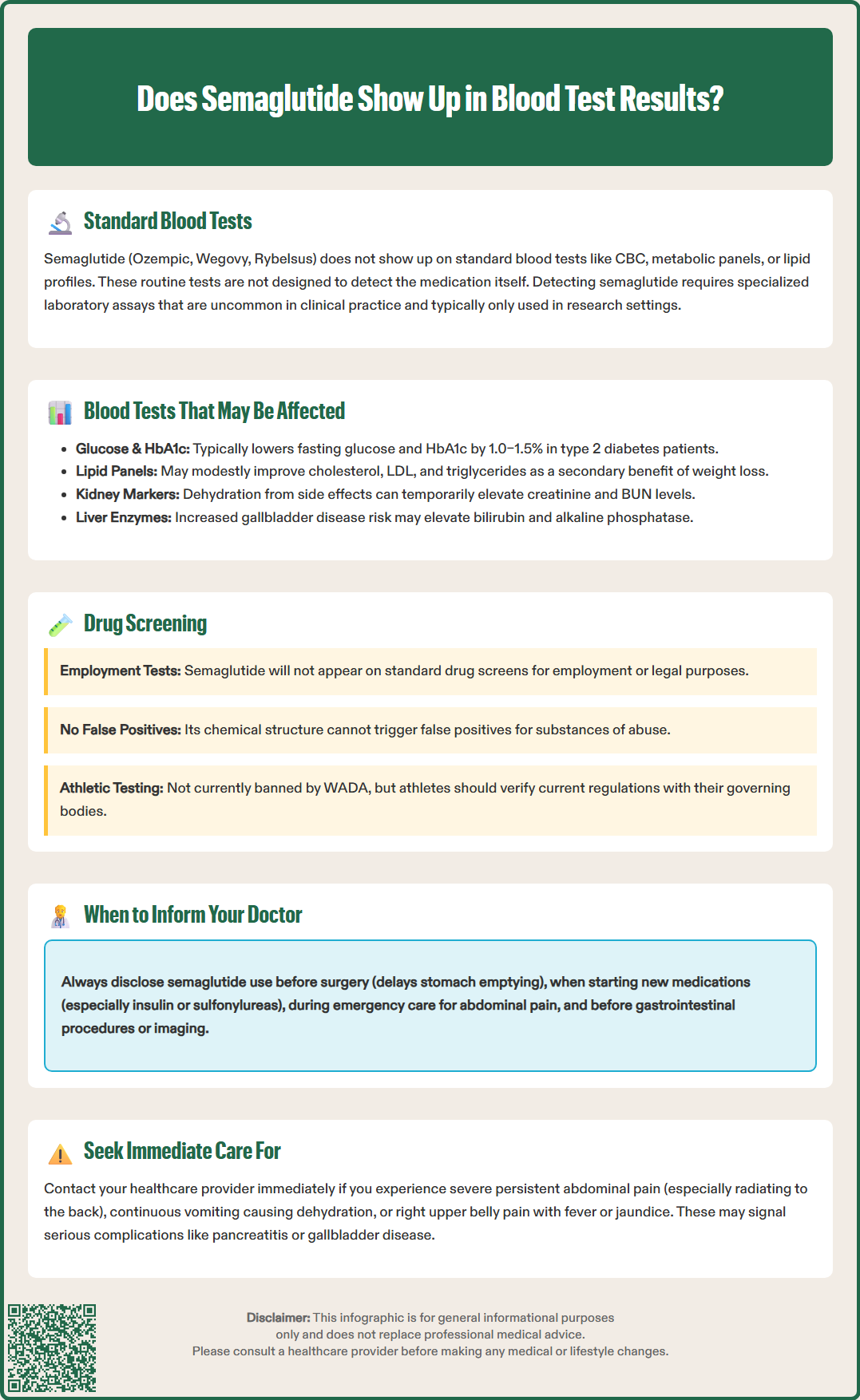
While semaglutide itself does not appear on standard blood tests, the medication can influence several laboratory values due to its pharmacological effects. Understanding these potential changes is essential for accurate interpretation of test results and appropriate clinical decision-making.
Glucose and Hemoglobin A1c (HbA1c): Semaglutide's primary mechanism involves enhancing glucose-dependent insulin secretion and suppressing glucagon release. Patients taking semaglutide typically experience reductions in fasting plasma glucose and HbA1c levels. According to FDA labeling and clinical trials, HbA1c reductions of 1.0–1.5% are common in patients with type 2 diabetes, though the exact reduction varies by baseline A1c, dose, and individual response. These improvements reflect the medication's therapeutic effect rather than a direct interference with the assay itself. Clinicians should interpret lower glucose values in the context of semaglutide therapy and adjust diabetes management accordingly.
Lipid Panel: Clinical studies have demonstrated that semaglutide may modestly improve lipid profiles, including reductions in total cholesterol, LDL cholesterol, and triglycerides. These changes are secondary to weight loss and improved glycemic control rather than direct lipid-lowering effects. When reviewing lipid panels in patients on semaglutide, providers should consider these potential improvements when assessing cardiovascular risk.
Liver Function Tests: Semaglutide generally has neutral or beneficial effects on liver enzymes, particularly in patients with metabolic dysfunction-associated steatotic liver disease who may show improvements due to weight loss. Rare cases of drug-induced liver injury have been reported, but routine hepatotoxicity is not characteristic of semaglutide. Clinical monitoring rather than routine liver enzyme testing is appropriate for most patients.
Renal Function Tests: Dehydration from semaglutide-associated gastrointestinal side effects (nausea, vomiting, diarrhea) may temporarily affect kidney function tests, potentially increasing creatinine and BUN levels. Patients with chronic kidney disease or those experiencing significant GI symptoms should be monitored appropriately.
Gallbladder-Related Tests: Semaglutide carries a risk of gallbladder disease, including cholelithiasis and cholecystitis, which may affect liver function tests (particularly bilirubin and alkaline phosphatase). Patients experiencing right upper quadrant pain, fever, or jaundice should seek prompt medical evaluation.
Pancreatic Enzymes: Semaglutide carries a warning regarding pancreatitis risk. Elevated lipase and amylase levels may occur, though routine monitoring of these enzymes is not recommended unless clinical symptoms suggest pancreatitis. Patients experiencing severe, persistent abdominal pain, especially if radiating to the back, should seek urgent medical care for appropriate evaluation, including pancreatic enzyme testing.
Semaglutide does not appear on standard drug screening panels used for employment, legal, or clinical purposes. These screenings typically test for substances of abuse, including opioids, amphetamines, benzodiazepines, cannabinoids, and cocaine metabolites. Semaglutide is a prescription peptide medication with no abuse potential and is not classified as a controlled substance by the Drug Enforcement Administration (DEA).
Standard immunoassay-based drug screens and confirmatory tests using gas chromatography-mass spectrometry (GC-MS) or liquid chromatography-mass spectrometry (LC-MS) are designed to detect specific drug classes and their metabolites. Semaglutide's chemical structure—a modified GLP-1 peptide—bears no resemblance to substances typically screened in these panels. There is no published evidence of false-positive cross-reactivity and low plausibility given semaglutide's peptide structure.
Patients undergoing pre-employment drug screening, athletic drug testing, or legal drug testing should not be concerned about semaglutide detection. The medication is a legitimate prescription therapy for type 2 diabetes and chronic weight management, approved by the FDA for these indications. However, patients should always disclose all medications to testing facilities and Medical Review Officers when appropriate, particularly in contexts where comprehensive medication histories are requested.
For athletes subject to anti-doping regulations, semaglutide is not currently listed as a prohibited substance by the World Anti-Doping Agency (WADA). However, regulations evolve, and athletes should verify current status with their governing bodies and follow Therapeutic Use Exemption processes if policies change. The medication's use for weight management in competitive sports may raise ethical questions separate from formal prohibition.
Transparent communication with healthcare providers about semaglutide use is essential for safe, effective care. Patients should inform all treating physicians about semaglutide therapy in several specific circumstances.
Before Any Surgical Procedure: Semaglutide delays gastric emptying, which can affect anesthesia risk. According to 2024 multi-society guidance (including the American Society of Anesthesiologists), most patients can continue GLP-1 receptor agonists before elective procedures. However, additional precautions may be recommended for patients with significant gastrointestinal symptoms, recent dose escalation, or gastroparesis. These may include a 24-hour liquid diet, gastric ultrasound, or procedure delay. Patients should inform their surgeon and anesthesiologist about semaglutide use well in advance of any planned surgery to allow for individualized planning.
When Starting New Medications: Semaglutide can interact with certain medications. Injectable semaglutide generally has limited clinical impact on most oral drugs, but patients starting insulin, sulfonylureas, or other diabetes medications require careful dose adjustments to prevent hypoglycemia. Oral semaglutide (Rybelsus) has specific considerations for medications like levothyroxine. Inform prescribers about semaglutide when receiving new prescriptions, particularly for medications with a narrow therapeutic index.
During Emergency Care: Emergency department physicians and urgent care providers need complete medication lists to make informed decisions. Semaglutide use is particularly relevant when evaluating abdominal pain (pancreatitis risk), severe nausea or vomiting (common adverse effects), or hypoglycemia.
For Imaging Studies: Patients undergoing gastrointestinal imaging or procedures should disclose semaglutide use, as delayed gastric emptying may affect study interpretation or preparation requirements.
Routine Laboratory Monitoring: While semaglutide doesn't require specific blood test monitoring beyond standard diabetes care, informing your primary care physician ensures appropriate interpretation of glucose, HbA1c, and other metabolic parameters.
When to Seek Urgent Care: Patients should seek immediate medical attention for severe, persistent abdominal pain (especially if radiating to the back), persistent vomiting leading to dehydration, or right upper quadrant pain with fever or jaundice. These symptoms could indicate serious conditions like pancreatitis, severe dehydration with acute kidney injury, or gallbladder disease.
Patients should maintain an updated medication list and bring it to all appointments, including those with specialists who may not have access to complete medical records.
No, semaglutide does not appear on standard employment drug screening panels, which test for substances of abuse like opioids, amphetamines, and cannabinoids. Semaglutide is a prescription peptide medication with no abuse potential and is not a controlled substance.
Semaglutide typically lowers fasting glucose and HbA1c levels by 1.0–1.5% in patients with type 2 diabetes through enhanced insulin secretion and reduced glucagon release. These changes reflect the medication's therapeutic effect and should be considered when interpreting blood sugar results.
Yes, you should inform your surgeon and anesthesiologist about semaglutide use before any surgical procedure. Semaglutide delays gastric emptying, which may require additional precautions or timing adjustments to reduce anesthesia-related risks.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.