LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does tirzepatide cause pancreatitis? This question concerns many patients considering this dual GIP/GLP-1 receptor agonist for type 2 diabetes or weight management. Tirzepatide, marketed as Mounjaro and Zepbound, carries an FDA warning about acute pancreatitis, similar to other incretin-based therapies. However, current clinical trial evidence does not establish a definitive causal link between tirzepatide and pancreatitis. Understanding the actual risk, warning signs, and when to seek medical attention is essential for patients and healthcare providers making informed treatment decisions about this medication.
Quick Answer: Current clinical trial evidence does not establish that tirzepatide causes pancreatitis, though the FDA includes a precautionary warning consistent with other GLP-1 receptor agonists.
Tirzepatide is a novel glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Marketed under the brand names Mounjaro (for diabetes) and Zepbound (for weight management in adults with BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity), tirzepatide represents the first dual incretin receptor agonist available in clinical practice.
The medication works through a unique dual mechanism of action. By activating both GIP and GLP-1 receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These combined effects improve glycemic control in patients with type 2 diabetes. Additionally, tirzepatide acts on appetite-regulating centers in the brain, promoting satiety and reducing caloric intake, which contributes to significant weight loss observed in clinical trials.
Tirzepatide is administered as a once-weekly subcutaneous injection, starting at 2.5 mg for treatment initiation, with maintenance doses ranging from 5 mg to 15 mg depending on the indication and individual patient response. The medication undergoes dose escalation to minimize gastrointestinal side effects, which are the most commonly reported adverse reactions. Clinical trials have demonstrated substantial improvements in hemoglobin A1c reduction (up to 2.5% decrease) in diabetes patients, while weight loss of up to 20% was observed primarily in adults with obesity without diabetes in the SURMOUNT-1 trial.
Understanding tirzepatide's mechanism is essential when evaluating potential adverse effects, including concerns about pancreatic safety, as the incretin pathway has complex interactions with pancreatic tissue.
The relationship between tirzepatide and pancreatitis remains an area of ongoing surveillance, though current evidence does not establish a definitive causal link. The FDA-approved prescribing information for tirzepatide includes a warning about acute pancreatitis, consistent with labeling for other GLP-1 receptor agonists, but this reflects precautionary monitoring rather than confirmed causation.
In the pivotal SURPASS clinical trial program evaluating tirzepatide for type 2 diabetes, pancreatitis events were rare. Across the SURPASS 1-5 trials involving over 6,000 participants, the incidence of adjudicated pancreatitis was low and comparable to control groups. The SURMOUNT trials for weight management similarly showed infrequent pancreatitis cases, with rates not significantly elevated compared to placebo. Analyses of incretin-based therapies, including tirzepatide data, have not found statistically significant increases in pancreatitis risk, though the absolute number of events was small.
However, post-marketing surveillance and real-world data collection continue to monitor this potential association. The FDA Adverse Event Reporting System (FAERS) has received reports of pancreatitis in patients taking tirzepatide, but these reports do not prove causation, as patients with type 2 diabetes and obesity have inherently elevated baseline risk for pancreatitis independent of medication use.
It is important to note that there is no proven causal mechanism in humans by which GIP/GLP-1 receptor activation directly causes pancreatic inflammation. Animal studies have shown conflicting results, with some suggesting potential pancreatic effects at suprapharmacologic doses, while others demonstrate no adverse pancreatic changes.
An additional consideration is that GLP-1 receptor agonists as a class have been associated with increased risk of gallbladder disease, which could indirectly increase pancreatitis risk. Rapid weight loss itself can also promote gallstone formation. The evidence to date has not shown a significant increase in pancreatitis with tirzepatide use, but continued monitoring is warranted.
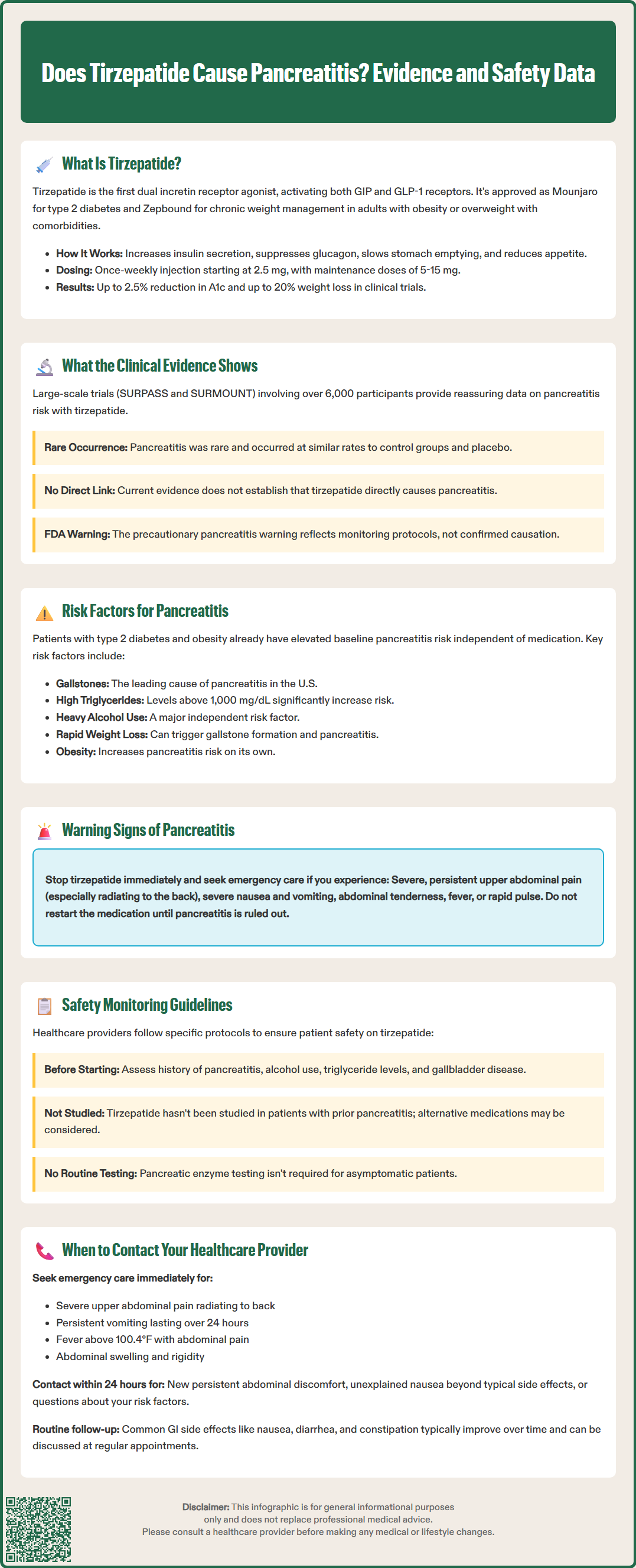
Patients with type 2 diabetes and obesity—the primary populations receiving tirzepatide—have multiple independent risk factors for acute pancreatitis that exist regardless of medication use. Understanding these baseline risk factors is crucial for appropriate patient counseling and risk stratification.
Key risk factors for pancreatitis include:
Gallstones (cholelithiasis): The most common cause of acute pancreatitis in the United States, accounting for approximately 40% of cases
Hypertriglyceridemia: Triglyceride levels above 1,000 mg/dL significantly increase pancreatitis risk
Alcohol consumption: Heavy alcohol use is the second leading cause of acute pancreatitis
History of pancreatitis: Prior episodes substantially increase recurrence risk
Obesity: Independent risk factor for both gallstone formation and pancreatitis severity
Rapid weight loss: Can precipitate gallstone formation and subsequent pancreatitis
Other factors: Hypercalcemia, certain medications, smoking, and genetic predisposition
Patients and healthcare providers should be aware of the characteristic warning signs of acute pancreatitis, which require immediate medical evaluation:
Classic symptoms include:
Severe, persistent abdominal pain: Typically located in the upper abdomen (epigastric region), often radiating to the back
Nausea and vomiting: Usually severe and persistent
Abdominal tenderness: Pain worsens with palpation
Fever: May develop as inflammation progresses
Rapid pulse: Tachycardia often accompanies acute episodes
The pain associated with pancreatitis is typically sudden in onset, constant rather than intermittent, and may be partially relieved by leaning forward. Patients experiencing these symptoms while taking tirzepatide should discontinue the medication and seek immediate medical attention. Diagnosis typically requires clinical evaluation, laboratory testing (serum lipase is the preferred diagnostic enzyme, typically elevated to three times the upper limit of normal), and imaging studies such as CT scan or abdominal ultrasound.
The FDA-approved Prescribing Information for tirzepatide (Mounjaro and Zepbound) includes specific warnings and precautions regarding pancreatic safety, reflecting ongoing pharmacovigilance for this medication class.
Key safety information in the Prescribing Information includes:
Use in patients with prior pancreatitis: Tirzepatide has not been studied in patients with a history of pancreatitis. Consider other antidiabetic therapies in patients with a history of pancreatitis.
Discontinuation guidance: If pancreatitis is suspected, promptly discontinue tirzepatide. If pancreatitis is confirmed, do not restart tirzepatide.
Patient education: Healthcare providers should inform patients about pancreatitis symptoms and the importance of immediate reporting.
The FDA does not require routine pancreatic enzyme monitoring in asymptomatic patients taking tirzepatide, as elevated lipase or amylase levels without clinical symptoms do not predict pancreatitis and may occur for various benign reasons. However, clinical best practice includes baseline assessment of pancreatitis risk factors before initiating therapy.
Pre-treatment evaluation should consider:
Comprehensive medical history, specifically asking about prior pancreatitis episodes
Assessment of alcohol consumption patterns
Lipid panel to identify hypertriglyceridemia (triglycerides ≥500 mg/dL warrant management to reduce risk)
Evaluation for gallbladder disease, particularly in patients with obesity
The FDA continues post-marketing surveillance through the FAERS database, and healthcare providers are encouraged to report any suspected pancreatitis cases to the FDA MedWatch program. The American Diabetes Association Standards of Care acknowledge the theoretical pancreatitis concern with incretin-based therapies but do not recommend avoiding these medications based on current evidence, emphasizing individualized risk-benefit assessment.
Patients taking tirzepatide should maintain open communication with their healthcare team and understand when immediate medical attention is necessary versus when routine follow-up is appropriate. Clear guidance on symptom recognition can prevent delays in diagnosis and treatment of serious complications.
Seek emergency medical care immediately if you experience:
Severe abdominal pain: Particularly sudden-onset, persistent pain in the upper abdomen that may radiate to your back
Persistent nausea and vomiting: Especially if unable to keep down food or liquids for more than 24 hours
Fever with abdominal pain: Temperature above 100.4°F (38°C) accompanied by abdominal symptoms
Abdominal distension or rigidity: Swelling or hardness of the abdomen with severe tenderness
If you develop severe, persistent upper abdominal pain (with or without vomiting), stop tirzepatide and seek urgent medical evaluation. Do not restart unless your clinician rules out pancreatitis; if pancreatitis is confirmed, do not restart tirzepatide.
Contact your healthcare provider within 24 hours for:
New or worsening abdominal discomfort that is persistent but not severe
Unexplained nausea or changes in appetite beyond typical medication side effects
Questions about your risk factors for pancreatitis
Concerns about medication interactions or other health changes
Schedule routine follow-up to discuss:
Expected gastrointestinal side effects (nausea, diarrhea, constipation) that are common with tirzepatide but typically improve over time
Weight loss progress and metabolic parameter monitoring
Dose adjustments based on efficacy and tolerability
Any new medications or supplements you're considering
Patients with known risk factors for pancreatitis—including history of gallstones, elevated triglycerides, or prior pancreatitis—should have more frequent monitoring and lower thresholds for evaluation of abdominal symptoms. Your healthcare provider can help establish an individualized monitoring plan based on your specific risk profile.
Warning signs include severe, persistent upper abdominal pain that may radiate to the back, persistent nausea and vomiting, fever, and abdominal tenderness. If you experience these symptoms, stop tirzepatide immediately and seek emergency medical care.
The FDA prescribing information recommends considering other antidiabetic therapies in patients with a history of pancreatitis, as tirzepatide has not been studied in this population. Discuss your individual risk-benefit profile with your healthcare provider.
Pancreatitis was rare in the SURPASS and SURMOUNT clinical trials involving over 6,000 participants, with incidence rates comparable to control groups and not significantly elevated compared to placebo.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.