LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many patients starting GLP-1 medications like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) wonder: does your stomach shrink on GLP-1 therapy? While these medications create a powerful sensation of reduced stomach capacity, the reality involves functional rather than structural changes. GLP-1 receptor agonists work by delaying gastric emptying and enhancing satiety signals, making you feel full sooner and longer. Understanding how these medications affect your stomach—and what changes are actually occurring—helps set realistic expectations and supports successful treatment outcomes.
Quick Answer: GLP-1 medications do not cause anatomical shrinkage of the stomach but create functional changes through delayed gastric emptying and enhanced satiety signaling.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound), work through multiple mechanisms that influence gastric function. These medications mimic the naturally occurring GLP-1 hormone, which is released by intestinal cells in response to food intake. When administered therapeutically, GLP-1 receptor agonists act primarily through vagal afferent pathways and central mechanisms rather than directly on the stomach wall itself.
The primary gastric effect of GLP-1 medications is delayed gastric emptying, meaning food remains in the stomach longer than usual. This occurs because GLP-1 receptor activation reduces the coordinated muscular contractions (peristalsis) that normally propel stomach contents into the small intestine. The FDA-approved prescribing information for both semaglutide and tirzepatide specifically notes that they delay gastric emptying, which contributes to reduced appetite and caloric intake. With long-term use of these medications, this gastric emptying effect often diminishes somewhat (tachyphylaxis), though other appetite-suppressing mechanisms remain effective.
GLP-1 medications enhance satiety signaling through both peripheral and central pathways. They increase feelings of fullness by modulating signals from stretch receptors when the stomach is distended with food and by affecting appetite-regulating centers in the brain. This dual mechanism—slowed emptying combined with enhanced satiety signals—creates a powerful effect on eating behavior. Patients typically report feeling satisfied with smaller portions and experiencing reduced hunger between meals, which facilitates the caloric deficit necessary for weight loss.
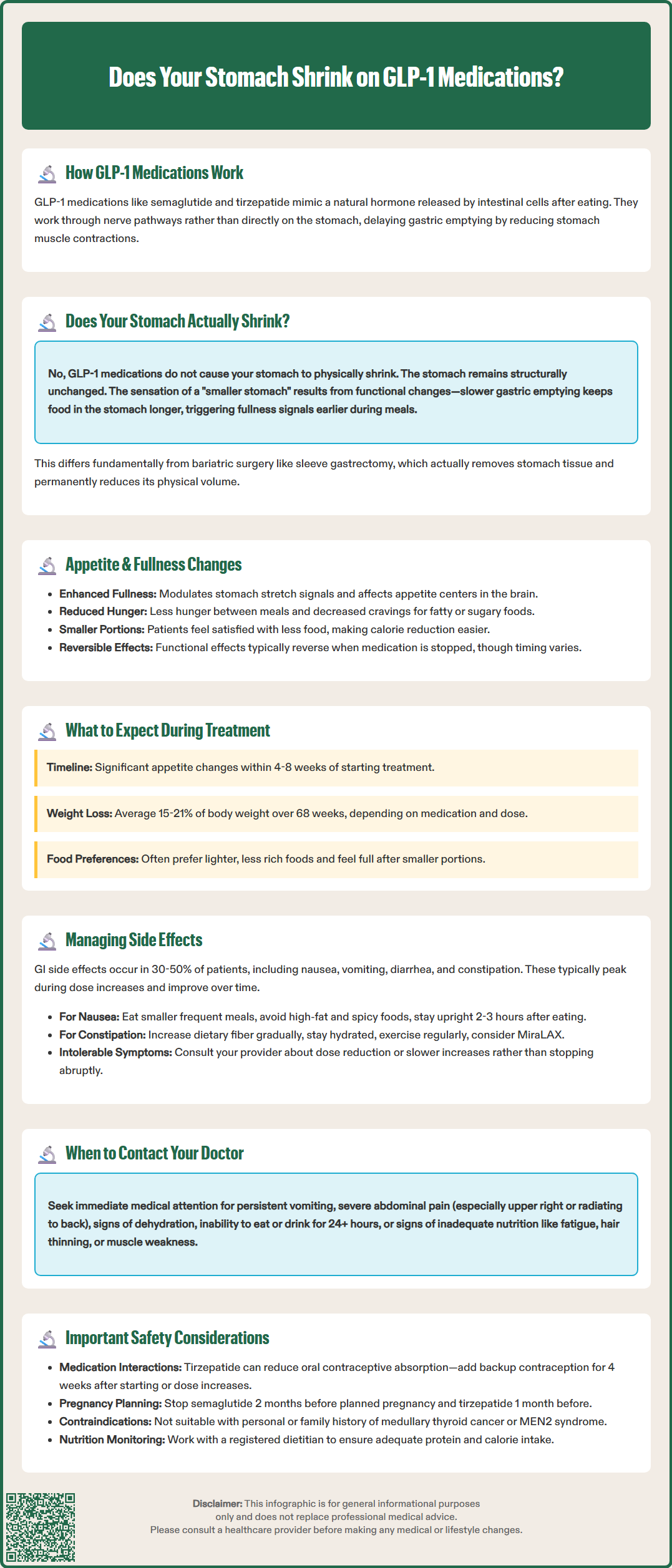
The short answer is that there is no established evidence that GLP-1 medications cause anatomical shrinkage of the stomach itself. The stomach is a muscular organ with considerable elasticity, capable of expanding to accommodate food and contracting when empty. While patients on GLP-1 therapy often report feeling full more quickly and being unable to eat as much as before treatment, this reflects functional changes rather than structural reduction in stomach size.
The sensation of a "smaller stomach" stems from altered gastric accommodation and heightened sensitivity to fullness cues. When GLP-1 receptor agonists slow gastric emptying, food remains in the stomach longer, triggering stretch receptors earlier in the meal. This creates the perception that the stomach has less capacity, even though its physical dimensions remain unchanged.
Behavioral changes associated with GLP-1 treatment may potentially influence gastric capacity over time. When patients consistently consume smaller portions for extended periods, the stomach may adapt to this pattern—though this adaptive response would be similar to what occurs with any sustained reduction in meal size, regardless of the method used.
It's important to distinguish between functional changes (how the stomach works) and structural changes (the stomach's physical size). This is notably different from bariatric surgical procedures like sleeve gastrectomy, which physically reduce stomach volume. GLP-1 medications primarily alter gastric function through delayed emptying and enhanced satiety signaling, not by causing the organ to physically shrink. The functional effects on appetite and satiety typically diminish when medication is discontinued, though the timeline and extent of this reversal vary between individuals.
Delayed gastric emptying represents one of the most clinically significant effects of GLP-1 receptor agonists. Under normal circumstances, the stomach empties approximately 50% of a meal within 2-3 hours. GLP-1 medications can significantly extend this timeline, with studies showing substantial prolongation of gastric emptying, particularly during initial therapy. This delayed transit has important implications for both appetite regulation and medication absorption.
The mechanism involves GLP-1 receptor activation on vagal afferent nerves and effects on gastric smooth muscle. When these receptors are stimulated, they reduce the frequency and amplitude of antral contractions—the muscular waves that normally grind food and push it through the pyloric sphincter into the duodenum. Additionally, GLP-1 may increase pyloric sphincter tone, creating a functional barrier that further slows gastric outflow. The FDA prescribing information for these medications specifically warns about this effect, particularly regarding the timing of oral medications that require predictable absorption.
Importantly, tirzepatide can reduce the absorption of oral contraceptives, particularly during dose initiation and escalation. The FDA label recommends using additional non-hormonal contraception for 4 weeks after initiating or increasing the dose of tirzepatide.
Appetite suppression through GLP-1 therapy operates through complementary pathways beyond delayed emptying alone. These medications affect appetite centers in the brain, primarily through areas where the blood-brain barrier is more permeable, and by modulating vagal signaling. They enhance satiety by influencing neural pathways associated with food intake and reward.
Key appetite-related changes patients typically experience include:
Reduced hunger between meals
Earlier onset of fullness during eating
Decreased food cravings, particularly for high-fat or high-sugar foods
Reduced interest in eating overall
These combined effects create a powerful tool for weight management but require careful monitoring, as excessive appetite suppression can lead to inadequate nutrition or dehydration if patients struggle to meet basic caloric and fluid needs.
Patients initiating GLP-1 therapy should anticipate a range of physical changes, most notably affecting eating patterns and digestive sensations. During the first 4-8 weeks, as the medication reaches therapeutic levels and the body adapts, many individuals report significant changes in their relationship with food. The most common experience is feeling satisfied after consuming smaller portions than previously required, though the exact reduction varies considerably between individuals.
Weight loss typically follows a pattern observed in clinical trials, though individual responses vary considerably. In the STEP 1 trial, semaglutide 2.4 mg (Wegovy) demonstrated average weight loss of approximately 15% of body weight over 68 weeks. The SURMOUNT-1 trial showed tirzepatide produced mean weight loss ranging from 15% to 21% depending on dose. Individual results vary based on baseline weight, adherence, dietary choices, and metabolic factors.
Physical changes commonly reported include:
Reduced meal portion sizes without feeling deprived
Prolonged sensation of fullness after eating
Changes in food preferences, often favoring lighter, less rich foods
Gradual reduction in abdominal circumference as visceral fat decreases
Patients should monitor for signs of inadequate nutrition, including fatigue, hair thinning, or muscle weakness, which may indicate insufficient protein or caloric intake. The American Diabetes Association Standards of Care emphasize the importance of ongoing nutrition therapy for patients using weight loss medications. Working with a registered dietitian can help ensure adequate nutrient intake despite reduced appetite.
Important safety considerations include:
Pregnancy planning: Discontinue semaglutide at least 2 months before a planned pregnancy and tirzepatide at least 1 month before attempting conception
Boxed warning: These medications are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2)
Hypoglycemia risk: Patients taking insulin or sulfonylureas may need dose adjustments to prevent low blood sugar
Gastric effects may intensify temporarily after dose escalations, which typically occur every 4 weeks during the titration phase. Patients should expect their tolerance for food volume to fluctuate during these adjustments, with gradual stabilization as the body adapts to each new dose level.
Gastrointestinal side effects represent the most common adverse events associated with GLP-1 therapy, affecting 30-50% of patients to varying degrees. The FDA prescribing information for semaglutide and tirzepatide lists nausea, vomiting, diarrhea, constipation, and abdominal pain as frequent adverse reactions. These effects typically peak during dose escalation periods and often diminish with continued use as physiological adaptation occurs.
Nausea management strategies include:
Eating smaller, more frequent meals rather than three large meals
Avoiding high-fat, greasy, or heavily spiced foods that delay gastric emptying further
Staying upright for 2-3 hours after eating to facilitate gastric emptying
Ensuring adequate hydration throughout the day
Considering anti-nausea medications if symptoms are severe (note: if metoclopramide is used, it should be short-term only under medical supervision due to risk of tardive dyskinesia)
Constipation affects approximately 20-30% of patients and results from slowed gastrointestinal transit throughout the digestive tract. Management includes increasing dietary fiber gradually (to avoid worsening bloating), maintaining adequate hydration based on individual needs, and incorporating regular physical activity. Polyethylene glycol (MiraLAX) is generally the preferred over-the-counter option for constipation, as recommended by gastroenterology guidelines. Patients should consult their healthcare provider before starting any new medications.
Some patients experience diarrhea, particularly after meals. This may reflect altered gut motility or sensitivity. Dietary modifications emphasizing lean proteins, complex carbohydrates, and limiting fat intake often provide relief. Starting with small, simple meals and gradually advancing the diet can help minimize symptoms.
When to seek medical attention:
Persistent vomiting preventing adequate fluid intake
Severe abdominal pain, particularly if localized to the upper right quadrant (potential gallbladder issues)
Severe pain in the upper abdomen radiating to the back (possible pancreatitis)
Signs of dehydration (dark urine, dizziness, decreased urination)
Inability to tolerate any food or liquids for more than 24 hours
Severe constipation with abdominal distension or vomiting (possible ileus/obstruction)
Yellowing of skin/eyes with fever and abdominal pain
Patients with significant vomiting or diarrhea should be monitored for signs of acute kidney injury, particularly those with pre-existing renal impairment or taking medications that affect kidney function.
Patients experiencing intolerable side effects should not discontinue medication abruptly without medical guidance. Dose reduction or temporary treatment interruption, followed by slower re-titration, often allows continued therapy with improved tolerance. The prescribing provider may also consider switching between different GLP-1 formulations, as individual responses can vary between medications in this class.
Most patients experience the most significant gastric adjustment during the first 4-8 weeks of GLP-1 therapy, with side effects typically peaking during dose escalations and diminishing as the body adapts to each new dose level.
The functional effects of GLP-1 medications on appetite and gastric emptying typically diminish when treatment is discontinued, though the timeline varies between individuals. Since these medications cause functional rather than structural changes, gastric function generally returns to baseline.
There is no established evidence that GLP-1 medications cause permanent anatomical changes to stomach size. Unlike bariatric surgery procedures that physically reduce stomach volume, GLP-1 therapy primarily alters gastric function through delayed emptying and enhanced satiety signaling.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.