LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
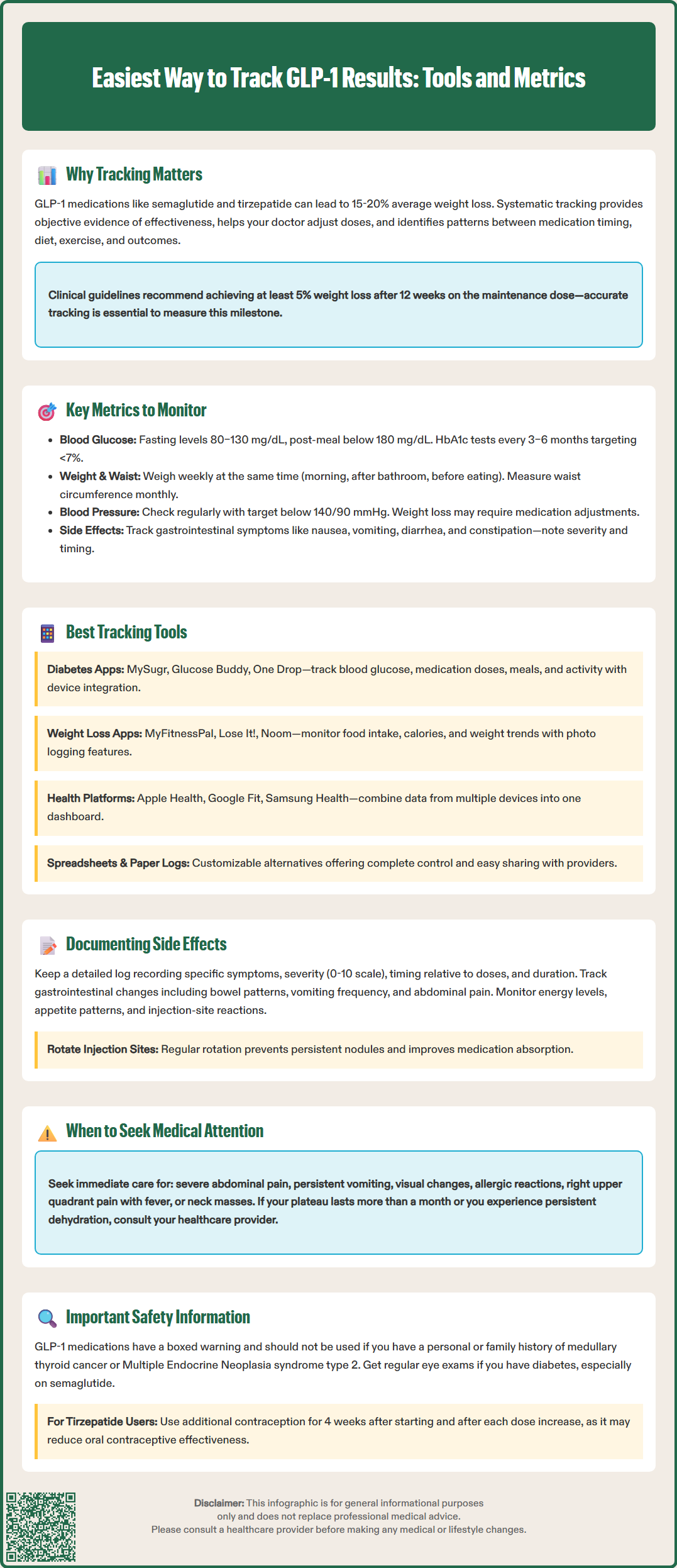
Tracking your progress on GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) is essential for optimizing treatment outcomes and safety. The easiest way to track GLP-1 results combines simple digital tools or paper logs with systematic monitoring of key metrics including blood glucose, weight, side effects, and cardiovascular parameters. Consistent documentation provides objective evidence of medication efficacy, helps identify patterns between lifestyle factors and outcomes, and enables early recognition of adverse effects requiring intervention. Whether you're managing type 2 diabetes or obesity, structured tracking supports evidence-based treatment decisions and shared decision-making with your healthcare provider, ensuring your GLP-1 therapy achieves therapeutic goals while minimizing risks.
Quick Answer: The easiest way to track GLP-1 results is using digital apps or simple spreadsheets to systematically monitor weight, blood glucose, side effects, and cardiovascular parameters at consistent intervals.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists such as semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound)—a dual GIP/GLP-1 receptor agonist—have transformed the management of type 2 diabetes and obesity. These medications work by mimicking incretin hormones, enhancing insulin secretion, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. Clinical trials demonstrate significant efficacy, with semaglutide showing average weight loss of approximately 15% in the STEP trials and tirzepatide achieving up to 20% weight loss in the SURMOUNT trials, though individual responses vary considerably.
Systematic tracking of your GLP-1 results serves multiple critical purposes. First, it provides objective evidence of treatment efficacy, helping you and your healthcare provider determine whether the medication is achieving therapeutic goals or whether dose adjustments are needed. Second, tracking creates a comprehensive record that can identify patterns between medication timing, dietary choices, physical activity, and outcomes. Third, documentation of side effects enables early recognition of adverse events that may require intervention, such as persistent nausea, dehydration, or signs of pancreatitis.
From a clinical perspective, consistent monitoring supports shared decision-making. The American Diabetes Association emphasizes individualized glycemic targets, and tracking data allows for personalized adjustments rather than population-based protocols. For weight management, FDA labeling and Endocrine Society guidelines recommend evaluating whether patients achieve at least 5% weight loss after approximately 12 weeks on the maintenance dose—a benchmark that requires accurate baseline and follow-up measurements. Without systematic tracking, these evidence-based treatment decisions become guesswork rather than precision medicine.
Importantly, these medications carry a boxed warning and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Effective GLP-1 tracking requires monitoring both primary therapeutic outcomes and safety parameters. The specific metrics depend on your treatment indication—diabetes management versus weight loss—though considerable overlap exists.
For diabetes management, the most important metric is blood glucose control. Home glucose monitoring frequency should follow your provider's recommendations, with targeted monitoring typically sufficient for those on GLP-1 therapy alone, while more frequent checks are needed when combined with insulin or sulfonylureas (which increase hypoglycemia risk). Per ADA guidelines, typical targets include fasting glucose of 80–130 mg/dL and 1–2 hour postprandial values below 180 mg/dL for most adults. HbA1c measurements, performed every 3–6 months, provide the gold standard for long-term glycemic control, with a general target of <7% for most adults with diabetes, though this may be individualized. Additionally, track episodes of hypoglycemia (blood glucose <70 mg/dL), noting severity, timing, and potential triggers.
Weight and body composition matter for all GLP-1 users. Weekly weight measurements, taken at the same time of day under consistent conditions (e.g., morning, after voiding, before eating), minimize variability. While scale weight provides useful trending data, waist circumference measured monthly offers additional metabolic information, as visceral adiposity reduction correlates with cardiovascular risk improvement.
Cardiovascular parameters warrant attention. Blood pressure should be monitored regularly, with targets generally <140/90 mmHg per ADA/ACC-AHA guidelines, particularly as weight loss may necessitate adjustment of antihypertensive medications. Heart rate changes, though typically modest with GLP-1 therapy, deserve documentation if symptomatic.
Gastrointestinal tolerance requires careful tracking, as nausea, vomiting, diarrhea, and constipation represent the most common adverse effects. Document frequency, severity, relationship to dosing or meals, and impact on nutrition and hydration. Persistent or severe symptoms may indicate the need for dose modification or additional supportive care, and can lead to dehydration and acute kidney injury if severe.
Additional monitoring should include regular eye examinations for people with diabetes, especially those on semaglutide, which can potentially worsen existing diabetic retinopathy with rapid glucose improvement. Also watch for symptoms of gallbladder disease (right upper quadrant pain, fever, jaundice), which has been associated with GLP-1 medications and weight loss.
The easiest way to track GLP-1 results combines digital tools with traditional methods, selecting approaches that match your technical comfort and lifestyle.
Dedicated diabetes management apps offer comprehensive tracking for patients using GLP-1 medications for glycemic control. Examples include MySugr, Glucose Buddy, and One Drop, which allow logging of blood glucose readings, medication doses, meals, and physical activity in a single platform. Many integrate with certain continuous glucose monitors (CGMs) and smart glucometers, automatically importing data and generating trend reports (check compatibility with your specific devices). These apps typically include reminder functions for medication administration and glucose testing, supporting adherence. Note that these apps are adjuncts to, not replacements for, medical advice or regulated device functions.
Weight loss and nutrition apps serve patients primarily using GLP-1 therapy for obesity management. Examples like MyFitnessPal, Lose It!, and Noom provide food logging, calorie tracking, and weight trending features. While not GLP-1-specific, these platforms help identify dietary patterns that optimize medication response. The ability to photograph meals creates a visual record that may reveal portion size changes or food tolerance issues related to delayed gastric emptying.
Comprehensive health tracking apps like Apple Health, Google Fit, or Samsung Health aggregate data from multiple sources—smart scales, fitness trackers, blood pressure monitors, and glucometers—into unified dashboards. This integration proves particularly valuable for patients monitoring multiple parameters, as it eliminates the need to consult separate platforms. Review privacy settings carefully before linking sensitive health data.
Simple spreadsheet tracking remains highly effective for those preferring non-app solutions. A basic spreadsheet with columns for date, weight, glucose readings, medication dose, side effects, and notes provides complete customization and easy sharing with healthcare providers. Many patients find the act of manual entry increases awareness and engagement.
Paper logs should not be dismissed, particularly for older adults or those with limited technology access. Structured logbooks designed for diabetes management work well for GLP-1 tracking, and many endocrinology practices provide templates. The key advantage is portability to appointments without device dependence.
The mention of specific apps does not constitute endorsement; patients should select tools based on individual needs and privacy preferences.
Systematic documentation of adverse effects and physical changes enables early problem recognition and supports clinical decision-making. The FDA-approved labeling for GLP-1 medications lists gastrointestinal symptoms as the most frequent adverse reactions, but comprehensive tracking should capture the full spectrum of potential effects.
Create a structured side effect log that records the specific symptom, severity (mild/moderate/severe), timing relative to medication dose, duration, and any interventions attempted. For nausea—the most common GLP-1 side effect—note whether it occurs primarily after injections, with meals, or throughout the day. Document dietary modifications that help or worsen symptoms, as this information guides practical management strategies. Rate severity using a 0–10 scale for consistency over time.
Gastrointestinal symptoms beyond nausea warrant detailed tracking. Document bowel movement frequency and consistency, as both diarrhea and constipation occur with GLP-1 therapy. Severe or persistent vomiting requires immediate attention due to dehydration risk, potential medication malabsorption, and risk of acute kidney injury. Abdominal pain, particularly if severe, persistent, or radiating to the back, may indicate pancreatitis—a rare but serious adverse effect requiring emergency evaluation. Note that routine amylase/lipase monitoring is not recommended in asymptomatic patients.
Physical changes extend beyond weight loss. Track energy levels, as some patients report fatigue during initial treatment or dose escalation. Changes in appetite and satiety patterns provide insight into medication effect; many patients describe prolonged fullness or reduced food cravings. Document injection-site reactions (redness, itching, nodules) and rotate injection sites regularly. Persistent nodules should be evaluated by your healthcare provider.
Red flag symptoms require immediate medical attention and should be clearly distinguished in your tracking system. These include severe abdominal pain, persistent vomiting with inability to tolerate fluids, visual changes (especially for people with diabetes and existing retinopathy), signs of allergic reaction (rash, difficulty breathing, facial swelling), right upper quadrant pain with fever or jaundice (possible gallbladder disease), or symptoms of thyroid tumors (neck mass, hoarseness, difficulty swallowing). These medications carry a boxed warning and are contraindicated in patients with personal or family history of medullary thyroid carcinoma or MEN2 syndrome.
Special considerations: For patients taking tirzepatide (Mounjaro, Zepbound), note that it may reduce the effectiveness of oral contraceptives during initiation and dose escalation. Additional contraceptive methods are recommended for 4 weeks after starting treatment and after each dose increase.
Share your tracking data with your healthcare provider at each visit, either through patient portal uploads, printed summaries, or app-generated reports. This documentation transforms subjective impressions into objective evidence, facilitating collaborative treatment optimization and ensuring that your GLP-1 therapy achieves maximum benefit with minimal adverse effects.
Track blood glucose levels (if managing diabetes), weekly weight measurements, gastrointestinal side effects, blood pressure, and any symptoms requiring medical attention such as severe abdominal pain or persistent vomiting. HbA1c should be measured every 3–6 months to assess long-term glycemic control.
Diabetes management apps like MySugr or Glucose Buddy work well for glycemic tracking, while weight loss apps like MyFitnessPal help monitor nutrition and weight trends. Comprehensive health platforms like Apple Health or simple spreadsheets also provide effective tracking solutions based on individual preferences.
Weigh yourself weekly at the same time of day under consistent conditions, such as in the morning after voiding and before eating. This frequency provides useful trending data while minimizing normal daily weight fluctuations that can obscure true progress.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.