LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 medications like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) have transformed type 2 diabetes and weight management. While these medications typically reduce blood pressure modestly—a benefit for many patients—some individuals may experience low blood pressure (hypotension) or related symptoms like dizziness and lightheadedness. Understanding the relationship between GLP-1 therapy and blood pressure changes is essential for safe use, particularly for patients taking antihypertensive medications or experiencing significant weight loss. This article explores how GLP-1 medications affect blood pressure, identifies risk factors for hypotension, and provides practical management strategies to optimize treatment outcomes.
Quick Answer: GLP-1 medications typically cause modest blood pressure reductions of 2-6 mmHg, but some patients may experience symptomatic low blood pressure, particularly when combined with antihypertensive medications, significant weight loss, or dehydration from gastrointestinal side effects.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily prescribed for type 2 diabetes management and, more recently, for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound)—though tirzepatide is technically a dual GIP/GLP-1 receptor agonist, not a pure GLP-1 agonist. They work by mimicking the action of naturally occurring GLP-1, an incretin hormone released by the intestine in response to food intake.
The primary mechanism of action involves binding to GLP-1 receptors on pancreatic beta cells, which stimulates glucose-dependent insulin secretion and suppresses inappropriate glucagon release. This glucose-dependent mechanism significantly reduces the risk of hypoglycemia when used alone, though this risk increases when combined with insulin or sulfonylureas. Beyond glycemic control, these medications slow gastric emptying, which prolongs satiety and reduces appetite through central nervous system pathways. These effects contribute to weight loss that varies by agent and dose—typically ranging from 5-8% with liraglutide 3 mg (Saxenda), up to 15% with semaglutide 2.4 mg (Wegovy), and potentially up to 20% with higher doses of tirzepatide (Zepbound).
Cardiovascular benefits have been demonstrated in clinical trials, with specific agents showing reductions in major adverse cardiovascular events. The FDA has approved certain medications (Victoza, Ozempic, Trulicity) for cardiovascular risk reduction in patients with established cardiovascular disease and type 2 diabetes, and Wegovy for cardiovascular risk reduction in adults with established cardiovascular disease who have overweight or obesity. While these medications offer significant therapeutic advantages, they can influence blood pressure through multiple mechanisms, including weight loss and potentially natriuresis (increased sodium excretion), typically producing modest reductions of 2-6 mmHg in systolic blood pressure. They may also slightly increase heart rate. Understanding these cardiovascular effects is essential for safe prescribing and monitoring, particularly in patients with baseline hypotension or those taking antihypertensive medications.
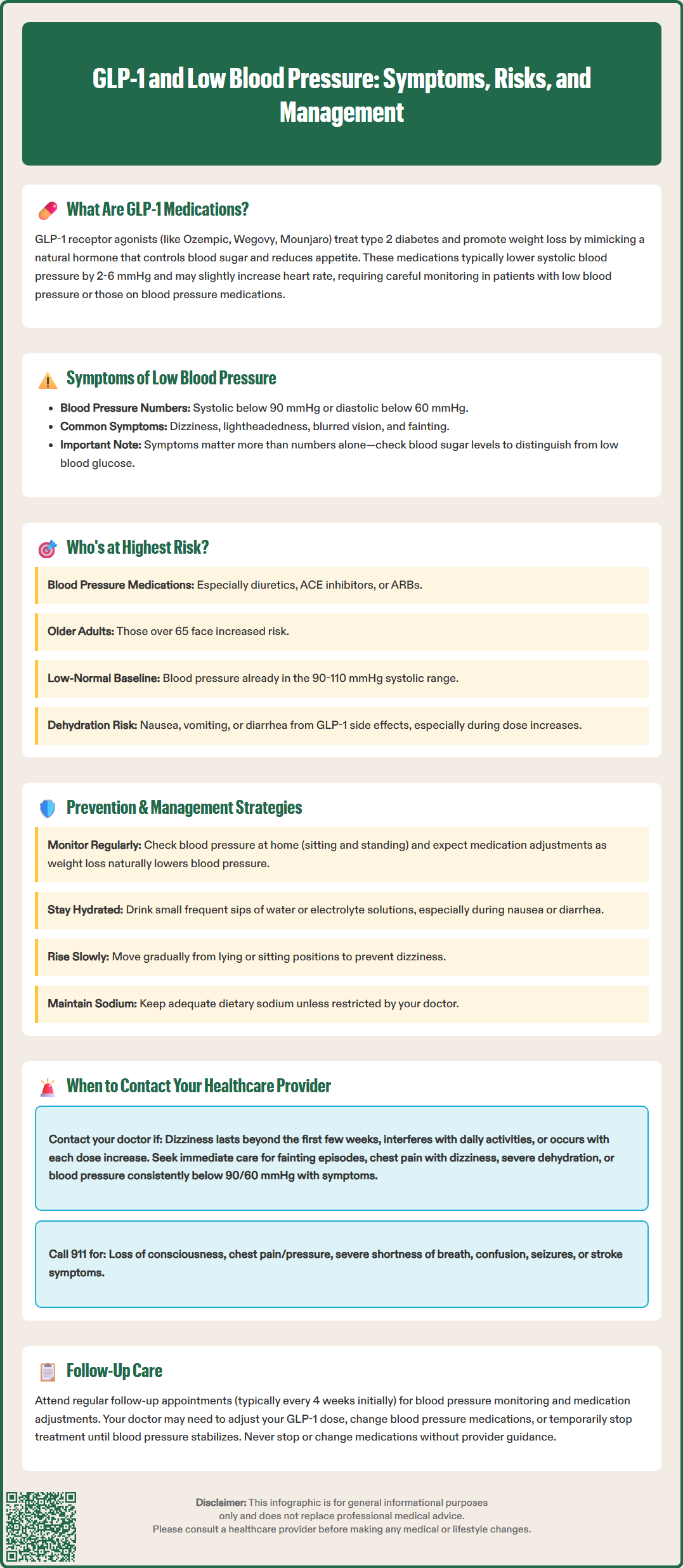
Low blood pressure, or hypotension, is generally defined as a systolic blood pressure below 90 mmHg or diastolic pressure below 60 mmHg, though symptoms matter more than absolute numbers. Orthostatic hypotension is specifically defined as a drop of ≥20 mmHg in systolic or ≥10 mmHg in diastolic blood pressure within 3 minutes of standing. Patients on GLP-1 therapy may experience orthostatic hypotension or symptomatic hypotension at any position. Common symptoms include dizziness, lightheadedness, blurred vision, fatigue, nausea, difficulty concentrating, and in severe cases, syncope (fainting). These symptoms often occur when transitioning from sitting or lying to standing, particularly in the morning or after prolonged rest.
While GLP-1 medications themselves do not typically cause significant hypotension directly, several mechanisms may contribute to blood pressure reduction. Substantial weight loss—a primary effect of these medications—typically leads to decreased blood pressure, which is generally beneficial for patients with hypertension. However, patients with normal or low-normal baseline blood pressure may experience symptomatic drops. Dehydration represents an important factor, as GLP-1 medications can cause nausea, vomiting, and diarrhea, particularly during dose escalation, leading to volume depletion. FDA labels note that dehydration from gastrointestinal adverse effects can contribute to acute kidney injury in some cases.
Key risk factors for developing hypotension on GLP-1 therapy include:
Concurrent use of antihypertensive medications, especially diuretics, ACE inhibitors, or ARBs
Concomitant use of SGLT2 inhibitors, which can cause osmotic diuresis and volume depletion
Baseline blood pressure in the low-normal range (systolic 90-110 mmHg)
Advanced age (65 years and older)
Autonomic dysfunction or diabetic neuropathy
Rapid or substantial weight loss
Inadequate fluid intake or gastrointestinal side effects causing dehydration
Concomitant use of other medications that lower blood pressure
Patients with type 1 diabetes using off-label GLP-1 therapy or those with longstanding type 2 diabetes and cardiovascular autonomic neuropathy may be at higher risk for orthostatic hypotension. When experiencing symptoms of dizziness or lightheadedness, patients should check their blood glucose to differentiate hypotension from hypoglycemia, as symptoms can overlap. Clinical vigilance is particularly important during the initial weeks of therapy and following dose increases.
Proactive blood pressure management is essential for patients initiating or continuing GLP-1 therapy, particularly those with risk factors for hypotension. Before starting treatment, healthcare providers should obtain baseline blood pressure measurements in both sitting and standing positions to identify pre-existing orthostatic hypotension. A comprehensive medication review is critical to identify drugs that may contribute to blood pressure reduction, including antihypertensives, alpha-blockers, tricyclic antidepressants, and certain medications for benign prostatic hyperplasia.
For patients taking antihypertensive medications, dose adjustments may be necessary as weight loss progresses and blood pressure naturally declines. The American Diabetes Association recommends regular blood pressure monitoring and medication titration to maintain blood pressure targets while avoiding symptomatic hypotension. Patients should be counseled to monitor their blood pressure at home if possible, recording measurements at consistent times and noting any symptoms. For orthostatic assessment, measure blood pressure after lying for 5 minutes, then again at 1 and 3 minutes after standing. A blood pressure log can help identify patterns and guide medication adjustments.
Practical strategies to minimize hypotension risk include:
Adequate hydration: Maintain consistent fluid intake throughout the day based on individual needs and medical conditions (consult your provider for personalized recommendations, especially if you have heart failure or kidney disease)
Gradual position changes: Rise slowly from lying to sitting, then sitting to standing, pausing between transitions
Dietary sodium: Unless contraindicated, maintain adequate sodium intake as directed by your healthcare provider
Compression stockings: Knee-high or thigh-high compression garments (20-30 mmHg) may help prevent blood pooling; waist-high garments may be more effective for severe symptoms
Meal timing: Avoid prolonged standing after meals when blood pressure naturally drops
Medication timing: Discuss with your healthcare provider whether adjusting the timing of antihypertensive medications might help manage symptoms
Patients experiencing gastrointestinal side effects should prioritize fluid and electrolyte replacement. Small, frequent sips of water, electrolyte solutions, or clear broths can help maintain hydration when nausea limits intake. During episodes of significant vomiting or diarrhea, patients should discuss with their provider whether to temporarily hold medications that can worsen volume depletion or affect kidney function (diuretics, ACE inhibitors, ARBs, SGLT2 inhibitors). If vomiting or diarrhea persists beyond 24 hours or if unable to keep fluids down for 4-6 hours, medical evaluation is warranted to assess for dehydration and potential need for temporary medication adjustment or intravenous fluid replacement.
While mild dizziness during the initial adjustment period may be common, certain symptoms warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience recurrent dizziness or lightheadedness that interferes with daily activities, particularly if symptoms persist beyond the first few weeks of therapy or occur with each dose increase. Any episode of syncope (loss of consciousness) requires immediate medical assessment, as this may indicate significant hypotension or other serious conditions requiring investigation.
Contact your healthcare provider promptly if you experience:
Persistent dizziness lasting more than a few seconds when standing
Fainting or near-fainting episodes
Falls or loss of balance attributed to dizziness
Chest pain, palpitations, or irregular heartbeat accompanying low blood pressure symptoms
Severe or persistent nausea, vomiting, or diarrhea leading to dehydration
Confusion, difficulty concentrating, or unusual fatigue
Blood pressure readings consistently below 90/60 mmHg with symptoms
New or worsening shortness of breath
Seek emergency care (call 911) if you experience:
Loss of consciousness
Chest pain or pressure
Severe shortness of breath
Confusion or altered mental status
Seizures
Signs of stroke (facial drooping, arm weakness, speech difficulty)
Your healthcare provider may need to adjust your GLP-1 medication dose, modify or discontinue antihypertensive medications, or investigate other potential causes of hypotension. In some cases, temporary discontinuation of GLP-1 therapy may be necessary until blood pressure stabilizes. If you experience syncope or near-syncope, avoid driving or operating machinery until evaluated by your healthcare provider. Regular follow-up appointments are essential during GLP-1 therapy, typically aligning with the medication's titration schedule (often every 4 weeks initially) and as clinically indicated. These visits allow for blood pressure monitoring, medication adjustments, and assessment of weight loss progress. Patients should never discontinue or adjust medications without provider guidance, as abrupt changes can lead to worsening or uncontrolled blood pressure or loss of glycemic control. Open communication with your healthcare team ensures safe, effective use of GLP-1 medications while minimizing the risk of hypotension and other adverse effects.
GLP-1 medications typically cause modest blood pressure reductions of 2-6 mmHg, which is generally beneficial. However, some patients may experience symptomatic low blood pressure, particularly when combined with antihypertensive medications, during significant weight loss, or when dehydrated from gastrointestinal side effects.
Common symptoms include dizziness, lightheadedness, blurred vision, fatigue, nausea, and difficulty concentrating, often occurring when standing up. Severe cases may cause fainting (syncope), which requires immediate medical evaluation.
Never adjust medications without consulting your healthcare provider. As GLP-1 therapy progresses and weight loss occurs, your provider may need to reduce or discontinue some antihypertensive medications to prevent symptomatic low blood pressure, but this decision requires medical supervision and regular blood pressure monitoring.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.