LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How long does semaglutide take to suppress appetite? Most patients begin experiencing noticeable appetite suppression within one to four weeks of starting semaglutide, a GLP-1 receptor agonist FDA-approved for chronic weight management and type 2 diabetes. This medication works by activating appetite-regulating centers in the brain and slowing gastric emptying, creating sustained feelings of fullness. Individual response varies based on dosing schedule, metabolic factors, and adherence to the prescribed titration protocol. Understanding the expected timeline helps patients set realistic expectations during treatment initiation and optimize therapeutic outcomes through proper medical supervision.
Quick Answer: Semaglutide typically begins suppressing appetite within one to four weeks of treatment initiation, with more pronounced effects emerging after four to five weeks at therapeutic doses.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that mimics the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake. By binding to GLP-1 receptors in multiple tissues, semaglutide exerts several complementary effects that collectively reduce appetite and promote weight loss.
The primary mechanism involves direct action on appetite-regulating centers in the hypothalamus and brainstem. When semaglutide activates GLP-1 receptors in these brain regions, it enhances satiety signals and reduces hunger perception. Additionally, the medication slows gastric emptying—the rate at which food leaves the stomach—which prolongs the feeling of fullness after meals and reduces the desire to eat between meals. This gastric emptying effect is typically most pronounced during early treatment and may attenuate somewhat with continued therapy.
Semaglutide may also influence reward pathways in the brain that govern food-seeking behavior and cravings, particularly for high-calorie, palatable foods. This neurological effect may help patients resist impulse eating and make more deliberate dietary choices. The medication's half-life of approximately one week allows for once-weekly subcutaneous administration, maintaining steady drug levels that provide consistent appetite suppression throughout the dosing interval.
It is important to note that while semaglutide is FDA-approved for chronic weight management (as Wegovy) and type 2 diabetes treatment (as Ozempic), its appetite-suppressing effects are dose-dependent. The weight management formulation uses higher doses specifically to optimize these anorectic effects, whereas diabetes-focused dosing prioritizes glycemic control with appetite suppression as a beneficial secondary effect.
Most patients begin experiencing noticeable appetite suppression within the first one to four weeks of initiating semaglutide therapy, though individual responses vary considerably. Some patients may notice reduced hunger and increased satiety relatively early in treatment, while others require several weeks at therapeutic doses before experiencing significant appetite changes.
The standard titration schedule for semaglutide involves starting at a low dose—typically 0.25 mg weekly for the first four weeks—and gradually increasing every four weeks until reaching the maintenance dose. This stepwise approach minimizes gastrointestinal side effects but means that full appetite-suppressing effects may not manifest until patients reach higher doses, often at 1.7 mg or 2.4 mg weekly for weight management indications.
Pharmacokinetic studies demonstrate that semaglutide reaches steady-state concentrations in the bloodstream after approximately four to five weeks of consistent weekly dosing. This pharmacological timeline correlates with clinical observations that appetite suppression tends to become more pronounced and consistent after the first month of treatment, particularly as doses escalate during the titration phase. However, some appetite effects can occur before steady state is reached due to the medication's pharmacodynamic properties.
Patients should understand that the timeline for appetite suppression does not necessarily correlate directly with weight loss, which typically becomes evident after eight to twelve weeks of treatment, as demonstrated in clinical trials. Early appetite changes represent the initial pharmacological effect, while measurable weight reduction reflects the cumulative impact of sustained caloric deficit over time. Healthcare providers should counsel patients that patience during the titration period is essential for both tolerability and optimal therapeutic outcomes.
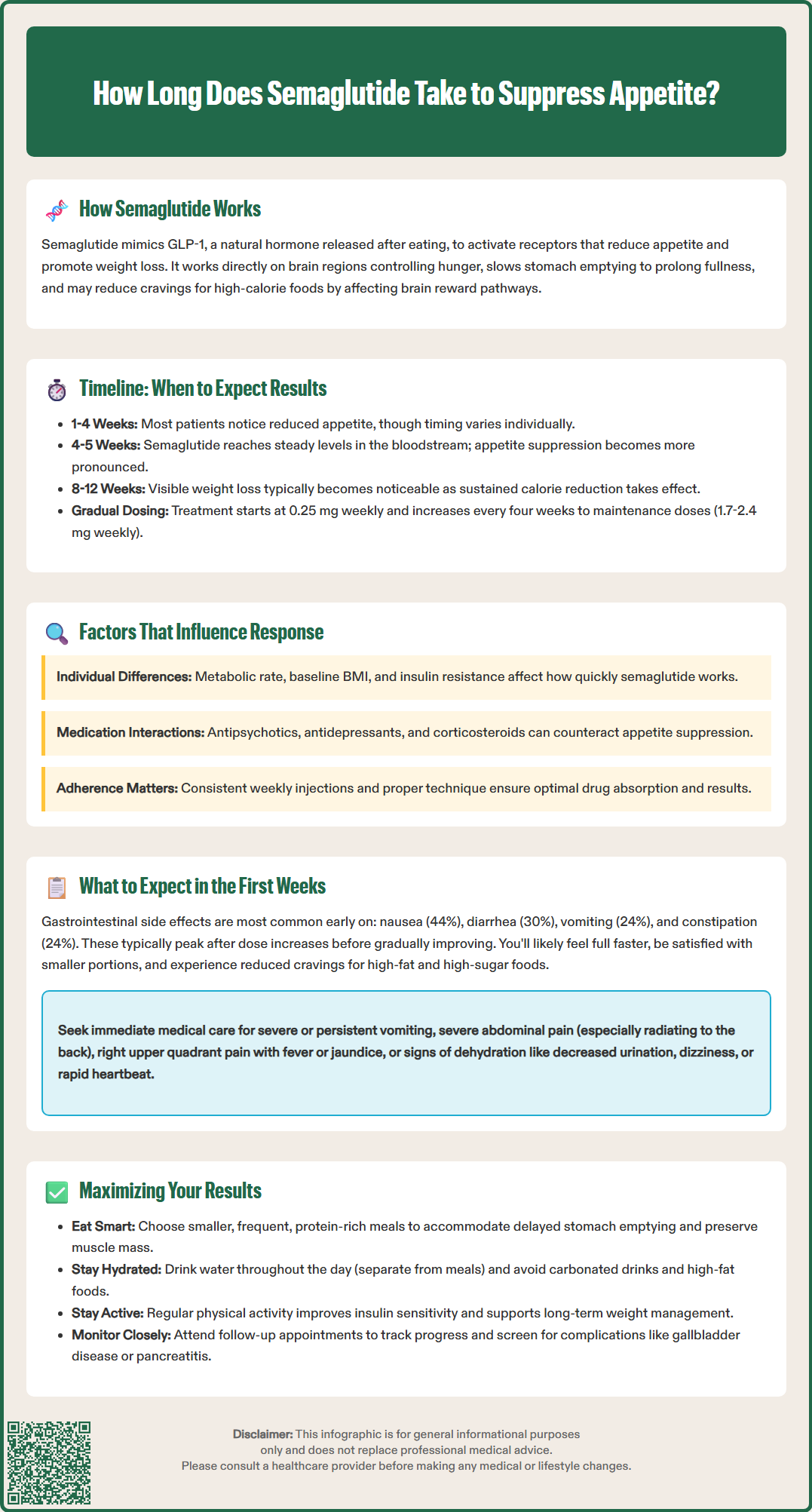
Several patient-specific and treatment-related factors influence the onset and intensity of semaglutide's appetite-suppressing effects. Individual metabolic differences may explain why some patients experience rapid appetite reduction while others have a more gradual response.
Baseline body weight and metabolic health status significantly impact treatment response. Patients with higher body mass index (BMI) or more severe insulin resistance may experience different responses to treatment. However, all patients should follow FDA-approved dosing schedules, which are designed to optimize both efficacy and tolerability.
Concomitant medications can influence semaglutide's effectiveness and tolerability. Medications that stimulate appetite—including certain antipsychotics, antidepressants, and corticosteroids—may partially offset semaglutide's anorectic effects. Importantly, when semaglutide is used with insulin or sulfonylureas in patients with diabetes, there is an increased risk of hypoglycemia that may require dose adjustments of these medications.
Adherence to the prescribed dosing schedule is critical for maintaining therapeutic drug levels. Missing doses or inconsistent injection timing can result in subtherapeutic concentrations and diminished appetite control. Proper injection technique and site rotation are also important; proper subcutaneous administration ensures optimal absorption, while injection-site reactions may occur if proper rotation is not practiced. Patients should receive thorough injection training and follow-up assessment to ensure proper technique throughout treatment.
The initial weeks of semaglutide therapy represent a critical adjustment period during which patients experience both therapeutic effects and potential adverse reactions. Gastrointestinal symptoms are the most common early side effects, with nausea affecting approximately 44% of patients, vomiting 24%, diarrhea 30%, and constipation 24% during dose escalation according to clinical trials. These symptoms typically peak within the first few days after each dose increase and gradually diminish as the body adapts to the medication.
Patients often report subtle changes in eating patterns before recognizing overt appetite suppression. Early signs include feeling satisfied with smaller portion sizes, reduced interest in snacking between meals, and decreased cravings for specific foods, particularly those high in fat and sugar. Some individuals describe a sensation of food sitting heavily in the stomach or feeling full more quickly during meals—direct consequences of delayed gastric emptying.
It is essential to distinguish between therapeutic appetite reduction and problematic gastrointestinal intolerance. While mild nausea and early satiety are expected and generally manageable, patients should seek immediate medical attention for severe or persistent vomiting, severe abdominal pain (especially if radiating to the back), right upper quadrant pain with fever or jaundice, or inability to maintain adequate hydration. Signs of dehydration requiring urgent care include decreased urine output, dizziness, or rapid heartbeat.
Patients with diabetes who take insulin or sulfonylureas should monitor blood glucose levels closely, as semaglutide may increase the risk of hypoglycemia when used with these medications. Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, and is not recommended during pregnancy or breastfeeding.
During this initiation phase, patients should maintain regular follow-up appointments to assess tolerability, review injection technique, and monitor for adverse effects. Healthcare providers should evaluate weight trends, vital signs, and metabolic parameters while providing ongoing education about realistic expectations. Patients should understand that the first month primarily focuses on establishing tolerance rather than achieving dramatic weight loss, and that therapeutic benefits accumulate progressively over subsequent months of treatment.
While semaglutide provides pharmacological appetite suppression, patients achieve optimal outcomes by combining medication with evidence-based lifestyle modifications. Dietary strategies that complement semaglutide's mechanism include consuming smaller, more frequent meals to accommodate delayed gastric emptying and reduced stomach capacity. Emphasizing protein-rich foods at each meal enhances satiety and helps preserve lean muscle mass during weight loss, addressing a common concern with rapid weight reduction.
Hydration management requires particular attention, as reduced appetite may inadvertently decrease fluid intake. Patients should aim for adequate water consumption throughout the day, separate from meals to avoid premature fullness. Avoiding carbonated beverages, high-fat foods, and large meal volumes can minimize gastrointestinal discomfort and optimize medication tolerability. Moderate alcohol consumption is advisable, as excessive intake may increase the risk of pancreatitis. Some patients benefit from keeping a food diary to identify patterns between dietary choices and symptom severity.
Physical activity enhances semaglutide's weight management effects through multiple mechanisms beyond caloric expenditure. Regular exercise improves insulin sensitivity, preserves metabolic rate during weight loss, and provides psychological benefits that support long-term adherence. Patients should work with healthcare providers to develop individualized activity plans appropriate for their fitness level and medical conditions, gradually increasing intensity as weight loss progresses and functional capacity improves.
Ongoing medical supervision ensures safe and effective treatment. Patients should attend scheduled follow-up appointments for monitoring of weight trends, metabolic parameters, and potential adverse effects. Healthcare providers should assess for signs of gallbladder disease, pancreatitis, or other serious complications throughout treatment. Patients with diabetes and pre-existing diabetic retinopathy should be monitored for worsening of this condition. Dose adjustments may be necessary based on individual response, tolerability, and achievement of therapeutic goals.
Many patients benefit from referrals to registered dietitians for personalized nutrition guidance, and some may require consultation with endocrinology or obesity medicine specialists for comprehensive care. Patients experiencing inadequate appetite suppression after reaching maintenance doses should undergo comprehensive evaluation for factors that may impair treatment response, including medication interactions, adherence issues, or underlying medical conditions requiring additional intervention.
Most patients do not experience immediate appetite suppression. Noticeable effects typically begin within one to four weeks, with more consistent suppression emerging after reaching higher maintenance doses during the gradual titration schedule.
The stepwise titration schedule minimizes gastrointestinal side effects such as nausea and vomiting, which are most common during dose escalation. Starting at 0.25 mg weekly and increasing every four weeks allows the body to adapt while optimizing tolerability and therapeutic outcomes.
Patients experiencing inadequate appetite suppression after reaching maintenance doses should consult their healthcare provider for comprehensive evaluation. Factors such as medication interactions, adherence issues, or underlying medical conditions may require assessment and potential intervention.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.