LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Patients taking GLP-1 medications like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) often wonder how much fiber per day on GLP-1 therapy is appropriate. The recommended daily fiber intake remains consistent with general guidelines: 25–38 grams for adults under 51, and 21–30 grams for those over 51. However, GLP-1 medications slow gastric emptying, making fiber intake particularly important for managing common side effects like constipation while supporting blood sugar control and satiety. Understanding how to optimize fiber consumption during GLP-1 treatment helps patients achieve better therapeutic outcomes and improved digestive comfort throughout their medication journey.
Quick Answer: Adults taking GLP-1 medications should consume 25–38 grams of fiber daily (depending on age and sex), consistent with standard US dietary guidelines, though gradual introduction may improve tolerance.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications originally developed for type 2 diabetes management. Some are now also FDA-approved for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) works through a dual mechanism as both a GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptor agonist. These medications work by mimicking naturally occurring intestinal hormones that regulate blood glucose levels and appetite.
The mechanism of action directly affects digestive function. GLP-1 receptor agonists slow gastric emptying—the rate at which food moves from the stomach into the small intestine—which contributes to prolonged satiety and improved glycemic control. This delayed gastric emptying effect may attenuate somewhat with continued use but remains clinically significant. According to FDA prescribing information, gastrointestinal adverse effects are among the most frequently reported reactions across all these medications.
The impact on digestive motility makes dietary fiber intake particularly relevant for patients taking GLP-1 medications. Fiber plays a crucial role in maintaining regular bowel function, supporting the gut microbiome, and potentially mitigating some medication-related gastrointestinal symptoms. Understanding the relationship between GLP-1 therapy and fiber consumption helps patients optimize both therapeutic outcomes and quality of life during treatment. Healthcare providers increasingly recognize that dietary modifications, including appropriate fiber intake, constitute an essential component of comprehensive treatment management rather than an optional consideration.
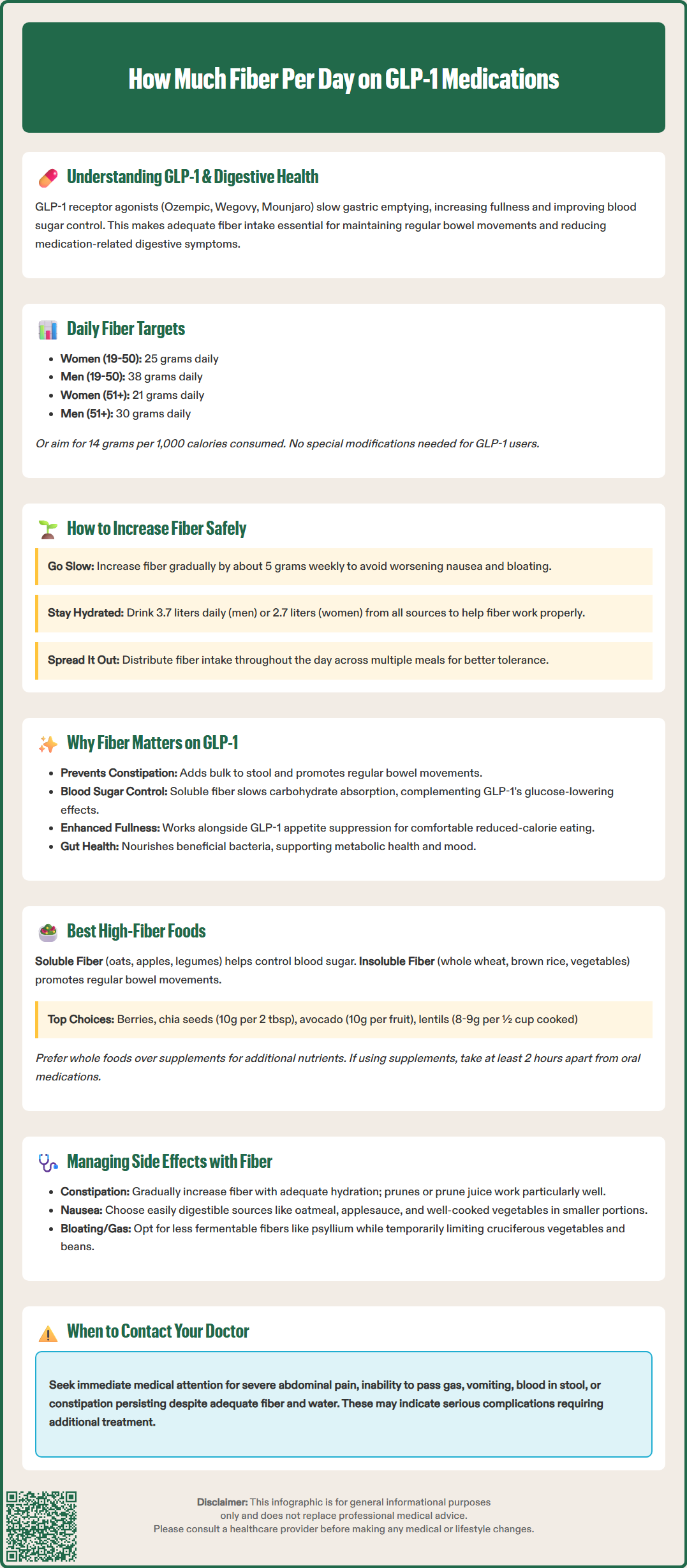
The recommended daily fiber intake for adults taking GLP-1 medications aligns with general population guidelines established by the US Dietary Guidelines for Americans and the National Academies of Sciences, Engineering, and Medicine. For adults ages 19-50, the Adequate Intake (AI) is approximately 25 grams daily for women and 38 grams daily for men. For adults over 51, the AI is 21 grams daily for women and 30 grams daily for men. Another approach is to aim for 14 grams of fiber per 1,000 calories consumed. These targets remain appropriate for patients on GLP-1 therapy, though individual tolerance and titration may be necessary.
There is no official modification to fiber recommendations specifically for GLP-1 users in current clinical guidelines from the American Diabetes Association or the American College of Physicians. However, clinical experience suggests that patients may benefit from a gradual approach to reaching fiber targets, particularly when initiating GLP-1 therapy or during dose escalation periods. Starting with current fiber intake and increasing by approximately 5 grams weekly allows the digestive system to adapt while minimizing potential discomfort.
Key considerations for fiber intake on GLP-1 medications include:
Gradual introduction: Sudden increases in fiber can exacerbate nausea or bloating when combined with delayed gastric emptying
Adequate hydration: Consuming sufficient water (approximately 3.7 liters total daily for men and 2.7 liters for women from all sources) helps fiber function effectively and prevents constipation. Patients with kidney disease, heart failure, or other conditions requiring fluid restriction should follow their healthcare provider's guidance
Distribution throughout the day: Spreading fiber across meals rather than concentrating intake at one time
Individual tolerance: Some patients may temporarily require slightly lower fiber intake during initial treatment phases
Patients experiencing persistent constipation despite adequate fiber and hydration should consult their healthcare provider, as additional interventions such as polyethylene glycol (PEG) or other osmotic laxatives may be appropriate per American Gastroenterological Association guidelines. Conversely, those experiencing diarrhea may need to adjust the types of fiber in their diet.
Dietary fiber serves multiple critical functions that become particularly important during GLP-1 therapy. Fiber helps regulate bowel movements, which is essential given that constipation affects many patients taking GLP-1 medications, with rates varying by specific agent and dose. For example, constipation rates in clinical trials were higher with weight management doses of semaglutide (Wegovy) compared to diabetes doses (Ozempic). The gastrointestinal effects of these medications, including delayed gastric emptying, can contribute to constipation. Adequate fiber intake, especially insoluble fiber, adds bulk to stool and promotes regular elimination.
Beyond addressing constipation, fiber contributes to glycemic control—a primary therapeutic goal for many GLP-1 users. Soluble fiber forms a gel-like substance in the digestive tract that slows carbohydrate absorption and helps prevent postprandial glucose spikes. This effect complements the glucose-lowering mechanism of GLP-1 medications, potentially enhancing overall metabolic outcomes. Research published in Diabetes Care consistently demonstrates that higher fiber intake correlates with improved hemoglobin A1c levels in patients with type 2 diabetes.
Fiber also supports satiety and weight management. While GLP-1 medications reduce appetite through central and peripheral mechanisms, fiber provides additional satiety through gastric distension and prolonged digestion. This dual approach may help patients adhere to reduced-calorie eating patterns more comfortably. Furthermore, fiber-rich foods typically have lower energy density, allowing larger portion sizes with fewer calories—an important consideration for patients adjusting to appetite changes.
The gut microbiome may benefit from adequate fiber intake, as certain fibers serve as prebiotics that nourish beneficial intestinal bacteria. A healthy microbiome may influence metabolic health, inflammation, and even mood—factors relevant to comprehensive diabetes and obesity management. Emerging evidence suggests that GLP-1 medications themselves may influence gut microbiota composition, though more human studies are needed to fully understand these effects.
Selecting appropriate high-fiber foods requires consideration of both fiber content and tolerability during GLP-1 treatment. Soluble fiber sources include oats, barley, apples, citrus fruits, carrots, and legumes such as lentils and black beans. Soluble fiber dissolves in water to form a gel, which may help with glycemic control. A half-cup of cooked oatmeal provides approximately 2 grams of fiber, while one medium apple with skin contains about 4.5 grams.
Insoluble fiber sources promote bowel regularity and include whole wheat products, wheat bran, brown rice, quinoa, nuts, seeds, and many vegetables including broccoli, cauliflower, and green beans. These fibers add bulk to stool and speed intestinal transit. One slice of whole wheat bread typically provides 2–3 grams of fiber, while a half-cup of cooked broccoli offers approximately 3 grams.
Practical high-fiber food choices for GLP-1 users include:
Berries: Raspberries (8 grams per cup), blackberries (7.6 grams per cup), and strawberries (3 grams per cup) provide fiber with relatively low volume
Chia and flax seeds: Two tablespoons of chia seeds deliver 10 grams of fiber and can be added to yogurt or smoothies
Avocado: One medium avocado contains approximately 10 grams of fiber with healthy fats that support nutrient absorption
Split peas and lentils: A half-cup cooked provides 8–9 grams of fiber with substantial protein
Artichokes: One medium artichoke offers 7 grams of fiber
Pears: One medium pear with skin contains about 6 grams of fiber
Patients should prioritize whole food sources over fiber supplements when possible, as whole foods provide additional nutrients, phytochemicals, and varied fiber types. However, supplements such as psyllium husk or methylcellulose may be appropriate for patients struggling to meet fiber goals through diet alone, particularly during periods of reduced appetite.
Patients taking oral semaglutide (Rybelsus) should note that this medication must be taken on an empty stomach with a small amount of water, at least 30 minutes before the first food, beverage, or other oral medications of the day. Fiber supplements should be separated from any oral medications by at least 2 hours to avoid potential interference with absorption.
Strategic fiber intake can help manage several common GLP-1-related gastrointestinal side effects, though the approach must be individualized. For constipation—one of the most frequent complaints—gradually increasing fiber while ensuring adequate hydration typically provides relief. Prunes or prune juice, which contain both fiber and sorbitol (a natural laxative), may be particularly effective. Patients should aim for consistent daily fiber intake rather than sporadic high-fiber days, as regularity supports predictable bowel function.
For nausea and early satiety, the relationship with fiber is more nuanced. While fiber is essential, consuming large volumes of high-fiber foods when nausea is prominent may worsen discomfort. During symptomatic periods, patients might focus on easily digestible fiber sources in smaller, more frequent portions. Oatmeal, applesauce, and well-cooked vegetables are often better tolerated than raw vegetables or large salads. As nausea improves—which typically occurs within 4–8 weeks of starting or increasing GLP-1 doses, though this timeline varies between individuals—fiber intake can be gradually expanded.
For bloating and gas, the fermentability of fiber matters significantly. Less fermentable fibers like psyllium and methylcellulose typically produce less gas than highly fermentable fibers found in some fruits, legumes, and certain grains. Additionally, certain high-fiber foods are more likely to cause gas, including cruciferous vegetables (broccoli, cabbage, Brussels sprouts), beans, and some whole grains. Patients experiencing problematic bloating might temporarily reduce these foods while maintaining fiber intake from better-tolerated sources such as rice, bananas, and cooked carrots.
Important safety considerations include:
Separate fiber supplements from medications: Take fiber supplements at least 2 hours apart from oral medications to avoid potential interference with absorption
Monitor for obstruction symptoms: Severe abdominal pain, inability to pass gas, or vomiting requires immediate medical evaluation, as FDA labels for GLP-1 medications include rare postmarketing reports of intestinal obstruction (ileus)
Coordinate with healthcare providers: Patients with inflammatory bowel disease, diverticulitis history, or other gastrointestinal conditions need individualized fiber recommendations
Adjust fluid intake appropriately: Follow medical guidance if you have conditions requiring fluid restriction
Patients should contact their healthcare provider if gastrointestinal symptoms persist despite dietary modifications, worsen significantly, or include warning signs such as blood in stool, unintentional weight loss beyond expected therapeutic effects, or severe abdominal pain. While fiber optimization helps many patients, it does not replace medical evaluation when symptoms suggest complications.
Maintain standard fiber recommendations (25–38 grams daily for most adults) but increase gradually by approximately 5 grams weekly to allow your digestive system to adapt. Sudden fiber increases combined with GLP-1's delayed gastric emptying may worsen nausea or bloating.
Prioritize easily digestible options like oatmeal, berries, cooked vegetables, lentils, and chia seeds. These provide substantial fiber with good tolerability during GLP-1 treatment, though individual responses vary.
Yes, adequate fiber intake (especially insoluble fiber from whole grains and vegetables) combined with proper hydration typically helps manage GLP-1-related constipation. If symptoms persist despite dietary modifications, consult your healthcare provider about additional interventions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.