LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

How much GLP-1 do you take depends on the specific medication prescribed, your treatment indication (type 2 diabetes or weight management), and your individual response to therapy. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda) follow gradual dose-escalation protocols to minimize side effects while achieving therapeutic goals. Dosing ranges from 0.25 mg to 2.4 mg weekly for semaglutide, 0.75 mg to 4.5 mg weekly for dulaglutide, and 0.6 mg to 3 mg daily for liraglutide, with your healthcare provider determining the optimal dose based on glycemic control, tolerability, renal function, and cardiovascular risk factors.
Quick Answer: GLP-1 receptor agonist doses vary by medication and indication, typically starting low and gradually increasing—semaglutide ranges from 0.25 mg to 2.4 mg weekly, dulaglutide from 0.75 mg to 4.5 mg weekly, and liraglutide from 0.6 mg to 3 mg daily.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are injectable medications primarily prescribed for type 2 diabetes management and, in some formulations, for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity. These medications are not indicated for type 1 diabetes or diabetic ketoacidosis (DKA).
The mechanism of action involves several pathways that improve glycemic control and support weight loss. GLP-1 receptor agonists stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they promote insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications. Additionally, these agents suppress glucagon secretion, slow gastric emptying, and act on central appetite centers in the brain to increase satiety and reduce food intake.
Currently available GLP-1 medications in the United States include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), exenatide (Byetta, Bydureon), and tirzepatide (Mounjaro, Zepbound)—though tirzepatide is technically a dual GLP-1/GIP receptor agonist. Each formulation has distinct dosing schedules, with some administered daily and others weekly.
Important safety considerations include a boxed warning for medullary thyroid carcinoma (MTC) risk with most GLP-1 medications, which are contraindicated in patients with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Other potential risks include pancreatitis, gallbladder disease, diabetic retinopathy complications (with semaglutide), and acute kidney injury if dehydration occurs.
The American Diabetes Association (ADA) guidelines recommend GLP-1 receptor agonists as preferred agents for patients with type 2 diabetes who have established atherosclerotic cardiovascular disease or indicators of high cardiovascular risk, or for those requiring additional glucose-lowering beyond metformin. Understanding the specific medication prescribed and its intended purpose helps patients appreciate why dosing varies considerably between individuals and formulations.
GLP-1 receptor agonist dosing varies significantly depending on the specific medication, indication (diabetes versus weight management), and formulation. All injectable GLP-1 medications follow a gradual dose-escalation approach to minimize gastrointestinal side effects, which are the most common adverse reactions.
Weekly Injectable Formulations:
Semaglutide (Ozempic) for type 2 diabetes typically starts at 0.25 mg once weekly for four weeks, then increases to 0.5 mg weekly. If additional glycemic control is needed, the dose may be increased to 1 mg weekly after at least four weeks, and potentially to a maximum of 2 mg weekly.
Semaglutide (Wegovy) for chronic weight management follows a different escalation: 0.25 mg weekly for four weeks, then 0.5 mg for four weeks, 1 mg for four weeks, 1.7 mg for four weeks, and finally a maintenance dose of 2.4 mg weekly.
Dulaglutide (Trulicity) begins at 0.75 mg once weekly, with potential increases to 1.5 mg, 3 mg, or a maximum of 4.5 mg weekly based on glycemic response.
Exenatide extended-release (Bydureon) is administered as 2 mg once weekly without dose titration. Not recommended in patients with severe renal impairment (CrCl <30 mL/min).
Tirzepatide (Mounjaro) for type 2 diabetes starts at 2.5 mg once weekly for four weeks, then increases to 5 mg. Dose can be increased in 2.5 mg increments every four weeks to a maximum of 15 mg weekly.
Tirzepatide (Zepbound) for weight management follows the same initial titration as Mounjaro but with a maintenance dose of 15 mg weekly for maximum effect.
Daily Injectable Formulations:
Liraglutide (Victoza) for diabetes starts at 0.6 mg daily for one week, then increases to 1.2 mg daily, with a possible increase to 1.8 mg if needed.
Liraglutide (Saxenda) for weight management escalates weekly from 0.6 mg to a maintenance dose of 3 mg daily.
Exenatide (Byetta) is initiated at 5 mcg twice daily, with a potential increase to 10 mcg twice daily after one month. Should be administered before meals and is not recommended in patients with severe renal impairment (CrCl <30 mL/min).
Oral Formulation:
Importantly, different formulations of the same medication (e.g., Ozempic, Wegovy, and Rybelsus) are not interchangeable despite containing semaglutide. These FDA-approved dosing schedules represent standard protocols, though individual patient circumstances may necessitate modifications under physician guidance.
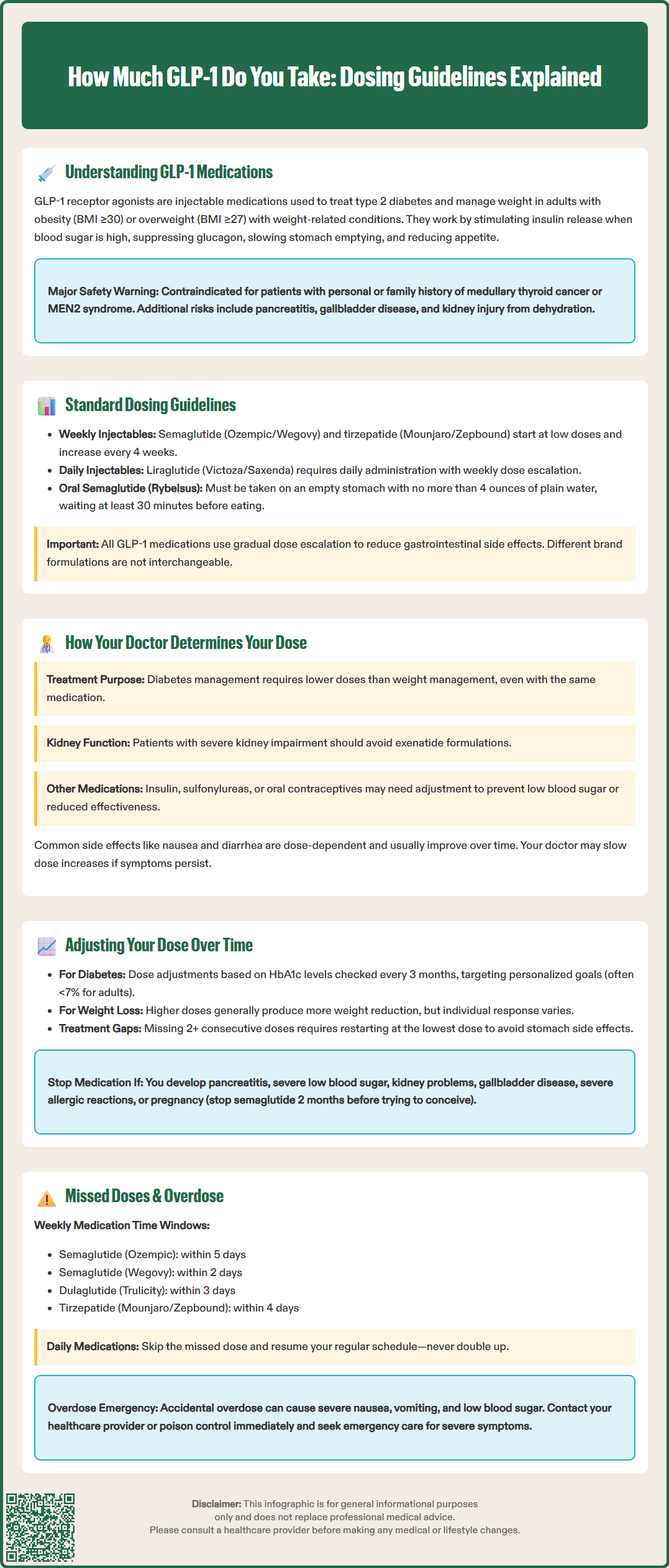
Determining the appropriate GLP-1 receptor agonist dose involves a comprehensive assessment of multiple clinical factors. Your healthcare provider considers your treatment goals, current health status, medication tolerance, and response to therapy when establishing and adjusting your dosing regimen.
Primary considerations include:
Treatment indication: Diabetes management typically requires lower doses than those used for weight management with the same medication. For example, semaglutide dosing differs substantially between Ozempic (diabetes) and Wegovy (weight management).
Baseline glycemic control: Patients with higher HbA1c levels may require more aggressive dose escalation, though this must be balanced against tolerability. The American College of Physicians (ACP) recommends targeting an HbA1c between 7% and 8% for most patients with type 2 diabetes, while the American Diabetes Association (ADA) often recommends <7% for many adults, with individualization based on patient factors.
Renal function: While most GLP-1 receptor agonists do not require dose adjustment for mild to moderate renal impairment, your kidney function influences medication selection and monitoring frequency. Exenatide (both immediate and extended-release) should be avoided in severe renal impairment (CrCl <30 mL/min). All patients should be monitored for acute kidney injury, especially if dehydration occurs.
Gastrointestinal tolerance: The most common adverse effects—nausea, vomiting, diarrhea, and constipation—are dose-dependent and typically diminish over time. Your provider may slow dose escalation or maintain a lower dose if you experience persistent gastrointestinal symptoms.
Cardiovascular history: Patients with established cardiovascular disease may benefit from GLP-1 receptor agonists with proven cardiovascular benefits, such as semaglutide, dulaglutide, or liraglutide, which may influence medication selection and target dosing.
Concurrent medications: Your provider reviews other glucose-lowering medications, particularly insulin or sulfonylureas, which may require dose reduction when initiating GLP-1 therapy to prevent hypoglycemia. Combining GLP-1 receptor agonists with DPP-4 inhibitors is generally not recommended due to limited additive benefit. For women taking tirzepatide with oral contraceptives, backup contraception may be advised during dose escalation due to potential reduced contraceptive exposure.
Contraindications: GLP-1 receptor agonists are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Caution is also warranted in patients with a history of pancreatitis.
Your doctor will also consider practical factors such as your ability to adhere to daily versus weekly injections, insurance coverage, and personal preferences when selecting the most appropriate GLP-1 medication and dosing strategy for your individual circumstances.
GLP-1 receptor agonist therapy requires ongoing assessment and potential dose adjustments based on treatment response, tolerability, and evolving clinical needs. The gradual dose-escalation approach used with these medications serves to minimize gastrointestinal side effects while achieving therapeutic goals.
Routine dose escalation follows manufacturer-recommended schedules, typically increasing every four weeks for weekly formulations or weekly for daily formulations. However, your healthcare provider may modify this timeline based on your individual response. If you experience significant nausea, vomiting, or other gastrointestinal symptoms, your doctor may recommend remaining at your current dose for an additional period before advancing, or may slow the escalation schedule.
For diabetes management, dose adjustments are guided by glycemic control markers, primarily HbA1c and self-monitored blood glucose readings. Your provider typically assesses HbA1c every three months during dose titration. If you achieve your glycemic target (often HbA1c <7% for many adults per ADA guidelines, though individualized based on age, comorbidities, and hypoglycemia risk), you may remain at your current dose. Inadequate glycemic response after at least four weeks at a given dose may prompt further escalation to the next tier.
For weight management indications, dose adjustments consider weight loss trajectory, tolerability, and plateau effects. Clinical trials demonstrate that higher doses generally produce greater weight reduction, but individual responses vary considerably. Some patients achieve satisfactory results at intermediate doses, while others require maximum approved doses.
Dose reduction or discontinuation may be necessary if you develop:
Persistent, intolerable gastrointestinal symptoms despite supportive measures
Acute pancreatitis (discontinue permanently)
Severe hypoglycemia, particularly if taking concurrent insulin or sulfonylureas
Acute kidney injury or worsening renal function
Gallbladder disease symptoms (abdominal pain, jaundice)
Diabetic retinopathy complications (particularly with semaglutide)
Severe hypersensitivity reactions including anaphylaxis or angioedema
Pregnancy or plans for pregnancy (for semaglutide, discontinue at least two months before planned conception; for other GLP-1 medications, follow specific label guidance; all should be discontinued when pregnancy is recognized)
After prolonged treatment interruptions (typically ≥2 consecutive missed doses or longer gaps), re-titration from the initial dose may be necessary according to product-specific guidelines to minimize gastrointestinal side effects.
Long-term maintenance dosing remains stable for many patients once therapeutic goals are achieved, though periodic reassessment ensures continued appropriateness of therapy. Your healthcare provider should review your treatment at least annually, considering whether continued GLP-1 therapy remains beneficial and whether dose adjustment might optimize outcomes.
Understanding how to manage missed doses or accidental overdoses is essential for safe GLP-1 receptor agonist use. The appropriate response depends on the specific medication, dosing frequency, and timing of the missed dose.
For weekly injectable GLP-1 medications (follow product-specific guidelines):
Semaglutide (Ozempic): If you miss your scheduled dose and remember within five days, administer the missed dose as soon as possible, then resume your regular weekly schedule. If more than five days have passed, skip the missed dose and take your next dose on the regularly scheduled day.
Semaglutide (Wegovy): If you miss a dose and remember within two days, administer the missed dose as soon as possible. If more than two days have passed, skip the missed dose and resume your regular schedule.
Dulaglutide (Trulicity): If you miss a dose and remember within three days, administer the missed dose. If more than three days have passed, skip the missed dose and take the next dose on the regularly scheduled day.
Tirzepatide (Mounjaro/Zepbound): If you miss a dose and remember within four days, administer the missed dose. If more than four days have passed, skip the missed dose and take the next dose on the regularly scheduled day.
Exenatide extended-release (Bydureon): If you miss a dose and it's three or more days until your next scheduled dose, take the missed dose. Otherwise, wait for your next scheduled dose.
For daily injectable GLP-1 medications:
Liraglutide (Victoza/Saxenda): If you miss a daily dose, resume your regular dosing schedule with the next scheduled dose. Do not take an extra dose or increase your next dose to compensate for the missed one.
Exenatide (Byetta): If you miss a dose, skip it and resume with the next scheduled dose. Do not take Byetta after a meal; it should be administered before meals.
For oral semaglutide (Rybelsus):
If you miss a dose, skip it and take your next dose the following day. Do not take two tablets on the same day.
After multiple missed doses (typically two or more consecutive doses), consult your healthcare provider, as re-titration from a lower dose may be necessary according to product-specific guidelines.
If you accidentally take too much:
GLP-1 receptor agonist overdose can cause severe nausea, vomiting, and potentially hypoglycemia, particularly in patients taking concurrent insulin or sulfonylureas (GLP-1 medications alone rarely cause hypoglycemia). If you accidentally inject more than your prescribed dose:
Contact your healthcare provider or poison control center (1-800-222-1222) immediately
Monitor for symptoms of hypoglycemia (shakiness, sweating, confusion, rapid heartbeat) if you take insulin or sulfonylureas
Stay well-hydrated and avoid eating large meals, which may worsen nausea
Seek emergency medical attention if you experience severe vomiting, signs of dehydration, severe abdominal pain, or altered consciousness
Important safety considerations:
Maintaining consistency in your dosing schedule optimizes therapeutic effects and minimizes side effects. Setting phone reminders, using the same injection day each week, or linking doses to daily routines can improve adherence. Always consult your medication's FDA-approved Prescribing Information and Instructions for Use for exact guidance. If you frequently miss doses or have difficulty managing your injection schedule, discuss this with your healthcare provider, who may recommend strategies to improve adherence or consider alternative treatment options. Never share your GLP-1 medication with others, even if they have the same diagnosis, as dosing must be individualized and gradually escalated under medical supervision.
Starting doses vary by medication: semaglutide (Ozempic/Wegovy) begins at 0.25 mg weekly, dulaglutide (Trulicity) at 0.75 mg weekly, and liraglutide (Victoza/Saxenda) at 0.6 mg daily. All GLP-1 medications start low and gradually increase every 4 weeks (weekly formulations) or weekly (daily formulations) to minimize gastrointestinal side effects.
No, never adjust your GLP-1 dose without consulting your healthcare provider. Dose escalation must follow FDA-approved schedules and be guided by your glycemic control, tolerability, and individual clinical factors to ensure safety and effectiveness.
For weekly GLP-1 medications, the window to take a missed dose varies by product: semaglutide (Ozempic) allows 5 days, semaglutide (Wegovy) allows 2 days, dulaglutide (Trulicity) allows 3 days, and tirzepatide (Mounjaro/Zepbound) allows 4 days. If beyond these windows, skip the missed dose and resume your regular schedule.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.