LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Sulfur burps—belching with a distinctive rotten egg odor—are an uncomfortable gastrointestinal side effect some patients experience while taking GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound). These medications slow gastric emptying to help control blood glucose and appetite, but this delayed digestion can increase gas formation, including hydrogen sulfide. While sulfur burps can be distressing, several evidence-based strategies can provide relief and prevention. Understanding why these symptoms occur and how to manage them effectively helps patients maintain their treatment regimen while minimizing discomfort.
Quick Answer: Sulfur burps on GLP-1 medications can be managed through over-the-counter remedies like bismuth subsalicylate, dietary modifications limiting sulfur-rich foods, smaller meal portions, and gradual dose titration under medical supervision.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Sulfur burps—characterized by a distinctive rotten egg odor—occur when hydrogen sulfide gas accumulates in the digestive tract and is expelled through belching. GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), as well as the dual GIP/GLP-1 receptor agonist tirzepatide (Mounjaro, Zepbound), may contribute to this uncomfortable symptom through their effects on digestion.
These medications work by mimicking naturally occurring incretin hormones, which slow gastric emptying—the rate at which food moves from the stomach into the small intestine. This delayed emptying helps control blood glucose and regulate appetite but can create conditions where food remains in the digestive tract longer than usual. This prolonged transit time may increase the opportunity for gas formation, including hydrogen sulfide, particularly when consuming foods containing sulfur compounds.
The FDA-approved prescribing information for these medications lists gastrointestinal adverse effects—including nausea, vomiting, diarrhea, and in some cases eructation (belching)—as common side effects. For example, in clinical trials of Wegovy (semaglutide), eructation was reported in 5.8% of patients versus 0% in the placebo group. While sulfur burps specifically are not explicitly listed in clinical trial data, belching is a recognized side effect that may be more noticeable during initial dose titration when the digestive system is adapting to the medication's effects. For many patients, these effects tend to diminish over time with continued treatment.
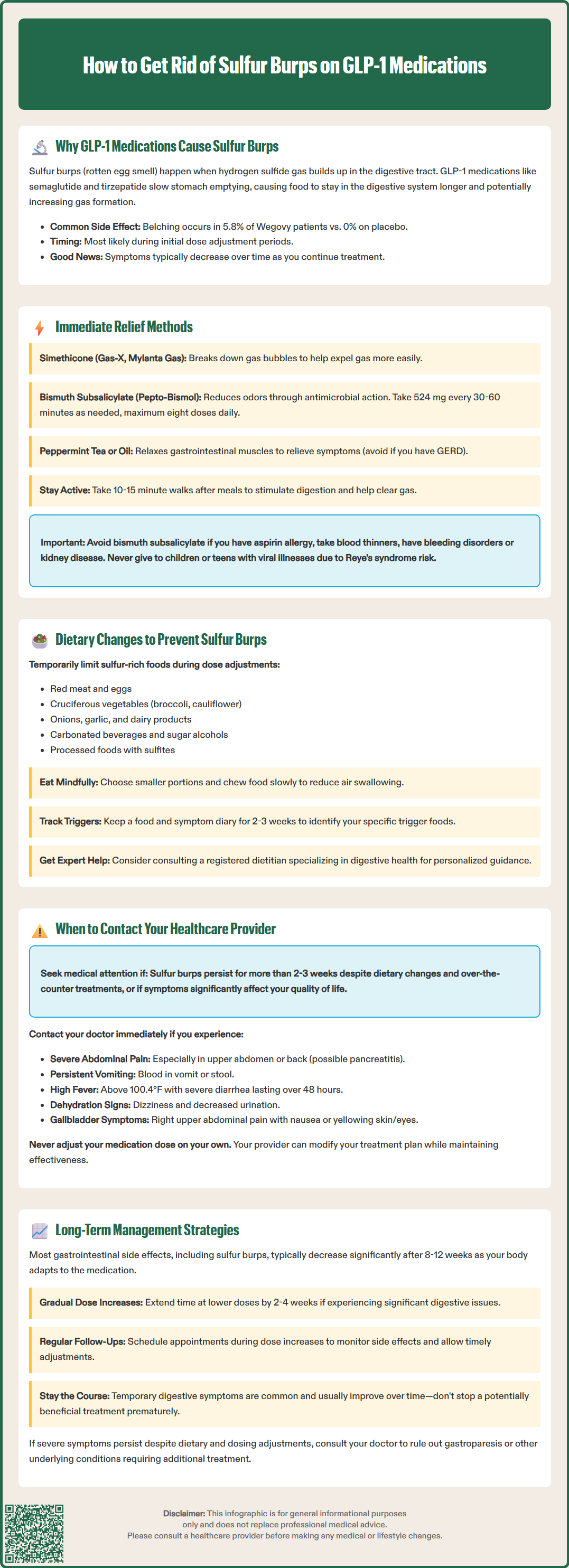
When sulfur burps occur, several strategies may provide relatively rapid symptomatic relief. Over-the-counter anti-gas products containing simethicone (such as Gas-X or Mylanta Gas) work by breaking down gas bubbles in the digestive tract, potentially facilitating easier expulsion. While simethicone does not specifically target hydrogen sulfide and has mixed evidence for efficacy, some patients find it provides modest relief.
Bismuth subsalicylate (Pepto-Bismol) may help reduce gastrointestinal odors through its antimicrobial properties and ability to bind some sulfur compounds. The typical adult dose is 524 mg (two tablets or 30 mL) every 30-60 minutes as needed, not exceeding eight doses in 24 hours. Important safety considerations include: avoid use if you have aspirin allergy, are taking anticoagulants or other salicylate medications, have bleeding disorders, or kidney disease. It should not be given to children or teenagers with or recovering from viral illnesses due to Reye's syndrome risk. Bismuth can cause temporary darkening of the tongue and stool.
Peppermint tea or peppermint oil capsules may provide relief through their carminative properties, which help relax gastrointestinal smooth muscle. However, peppermint oil should be used cautiously if you have gastroesophageal reflux disease (GERD) as it may worsen symptoms by relaxing the lower esophageal sphincter. Staying hydrated with non-carbonated beverages, sipped slowly throughout the day, may help dilute stomach contents. Light physical activity, such as a 10-15 minute walk after meals, can also stimulate digestive motility and promote gas clearance.
Dietary modification represents an important strategy for managing sulfur burps while taking GLP-1 medications. Consider temporarily limiting foods that may contribute to gas and odor, particularly during dose titration periods:
High-protein foods like red meat and eggs, which contain sulfur-containing amino acids
Cruciferous vegetables (broccoli, cauliflower, Brussels sprouts, cabbage)
Allium vegetables (onions, garlic, leeks)
Dairy products, especially if you have lactose intolerance
Some legumes that may cause gas in certain individuals
Processed foods containing preservatives like sulfites
Carbonated beverages that introduce additional gas
Sugar alcohols (sorbitol, mannitol, xylitol) found in sugar-free products, which can ferment in the digestive tract
These nutritious foods need not be eliminated entirely, and individual tolerance varies considerably. Portion control is particularly important while on GLP-1 therapy—smaller portions are often better tolerated than large meals. Chewing food thoroughly and eating slowly can reduce the amount of air swallowed during meals.
Keeping a food and symptom diary for 2-3 weeks can help identify your personal trigger foods. If dietary challenges persist, consider consulting with a registered dietitian who specializes in digestive health for personalized guidance. Some patients find that principles from low-FODMAP diets (which limit certain fermentable carbohydrates) may be helpful for short-term symptom management, though this should be done with professional guidance.
While sulfur burps are generally a benign if unpleasant side effect, certain circumstances warrant prompt medical evaluation. Persistent or worsening symptoms despite dietary modifications and over-the-counter interventions lasting more than 2-3 weeks should be discussed with your prescribing clinician, as this may indicate inadequate tolerance to the current dose or the need for alternative management strategies.
Accompanying gastrointestinal symptoms that suggest more serious conditions require medical assessment. Contact your healthcare provider if sulfur burps occur alongside:
Severe or persistent abdominal pain, particularly if localized to the upper abdomen or radiating to the back (possible pancreatitis)
Pain in the right upper quadrant of the abdomen, possibly with nausea, vomiting, or yellowing of the skin/eyes (possible gallbladder disease)
Persistent vomiting that prevents adequate oral intake or medication administration
Signs of dehydration (decreased urination, dizziness, extreme thirst)
Blood in vomit or stool
Unintentional weight loss exceeding expected therapeutic effects
Fever (temperature >100.4°F/38°C)
Severe diarrhea lasting more than 48 hours
These symptoms may indicate serious conditions such as pancreatitis (inflammation of the pancreas, a rare but serious adverse effect associated with GLP-1 medications), gallbladder disease (which can occur with weight loss), severe gastroparesis (delayed gastric emptying), or other gastrointestinal conditions requiring investigation.
Medication adjustment may be necessary if symptoms significantly impair quality of life. Your provider might recommend temporarily pausing dose escalation, extending the interval between dose increases, or switching to an alternative formulation. Never adjust medication doses independently, as this can compromise therapeutic efficacy.
Successful long-term management of sulfur burps and other gastrointestinal effects requires a comprehensive approach that balances therapeutic benefits with tolerability. Gradual dose titration represents the cornerstone of minimizing adverse effects. FDA-approved prescribing information for all GLP-1 medications specifies incremental dose increases over weeks to months. Patients experiencing significant symptoms may benefit from extending titration intervals beyond the standard schedule—for example, remaining at a lower dose for an additional 2-4 weeks before advancing.
For many patients, gastrointestinal side effects, including sulfur burps, diminish significantly after 8-12 weeks as physiologic adaptation occurs. According to FDA labeling for semaglutide products, the incidence of gastrointestinal adverse events typically decreases over time with continued treatment at the same dose level.
If severe symptoms persist despite conservative measures, your healthcare provider may consider further evaluation for conditions such as gastroparesis. In select cases with confirmed gastroparesis, prokinetic medications might be discussed, though this represents off-label use for GLP-1-related symptoms. Metoclopramide carries an FDA black box warning for tardive dyskinesia with use exceeding 12 weeks and should only be used under careful medical supervision with appropriate monitoring.
Regular follow-up during dose titration enables timely intervention when problems arise. The American Diabetes Association Standards of Care emphasizes the importance of monitoring both efficacy and tolerability of GLP-1 therapies, with follow-up frequency individualized based on the specific medication, titration schedule, and patient response.
Patient education about realistic expectations—that some transient gastrointestinal symptoms are common and typically improve—enhances adherence and reduces premature discontinuation of potentially beneficial therapy. Maintaining open communication with your healthcare team allows for adjustments to optimize both symptom management and therapeutic outcomes.
GLP-1 medications slow gastric emptying, causing food to remain in the digestive tract longer than usual. This prolonged transit time increases the opportunity for hydrogen sulfide gas formation, particularly when consuming foods containing sulfur compounds, resulting in sulfur burps with a rotten egg odor.
Temporarily limit high-protein foods like red meat and eggs, cruciferous vegetables (broccoli, cauliflower), allium vegetables (onions, garlic), dairy products, carbonated beverages, and sugar alcohols found in sugar-free products. Individual tolerance varies, so keeping a food diary can help identify your personal trigger foods.
Contact your healthcare provider if sulfur burps persist beyond 2-3 weeks despite dietary changes, or if accompanied by severe abdominal pain, persistent vomiting, blood in vomit or stool, fever, signs of dehydration, or pain radiating to the back, as these may indicate serious conditions like pancreatitis requiring immediate evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.