LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Learning how to give yourself a shot of semaglutide is a straightforward process that becomes routine with practice. Semaglutide, marketed as Ozempic for type 2 diabetes and Wegovy for chronic weight management, is a once-weekly subcutaneous injection that you can safely administer at home. This comprehensive guide walks you through proper injection technique, site selection, common mistakes to avoid, and side effect management. Whether you're preparing for your first injection or looking to refine your technique, understanding the correct procedure ensures optimal medication delivery and treatment success.
Quick Answer: Semaglutide is self-administered as a once-weekly subcutaneous injection into the abdomen, thigh, or upper arm using either a multi-dose pen (Ozempic) or single-dose pen (Wegovy).
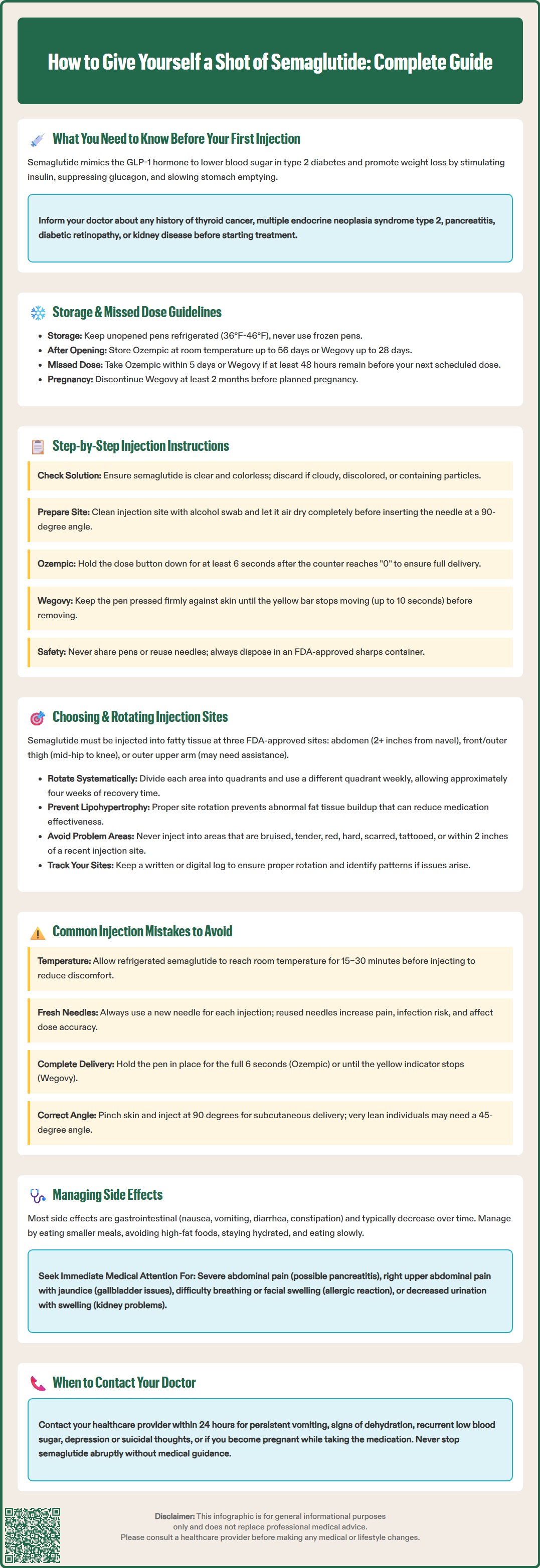
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Ozempic) and chronic weight management (Wegovy). Both formulations are administered as subcutaneous injections once weekly, but they use different delivery devices. Before your first injection, understanding the medication's mechanism and proper handling is essential for safe, effective treatment.
Semaglutide works by mimicking the incretin hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, and slows gastric emptying. This mechanism reduces blood glucose levels in people with type 2 diabetes and promotes satiety, contributing to weight loss. Ozempic comes in a multi-dose, dial-a-dose pen requiring needle attachment, while Wegovy is a single-dose disposable pen with a concealed needle.
Before beginning treatment, your healthcare provider should review your medical history, particularly any personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2, as semaglutide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. Additionally, discuss any history of pancreatitis, diabetic retinopathy, or kidney disease, as these conditions may require closer monitoring during treatment.
Semaglutide should not be used during pregnancy. If you're using Wegovy for weight management, you should discontinue it at least 2 months before a planned pregnancy and use effective contraception. If pregnancy occurs while on semaglutide, contact your healthcare provider immediately.
Key preparation steps include:
Storing unopened pens in the refrigerator (36°F to 46°F) and protecting them from light
After first use, Ozempic can be stored at room temperature (up to 86°F) for up to 56 days; Wegovy for up to 28 days
Allowing the pen to reach room temperature before injection (15–30 minutes)
Checking the medication's appearance—it should be clear and colorless
Never using a pen that has been frozen, even if subsequently thawed
Never sharing your pen or needles with anyone else, even if the needle is changed
If you miss a dose, follow specific guidelines: For Ozempic, administer within 5 days of the missed dose; for Wegovy, administer as soon as possible if at least 48 hours before the next scheduled dose.
Your healthcare provider or diabetes educator should demonstrate the injection technique during your initial visit. Many patients find it helpful to practice with a training pen before administering their first dose. Understanding proper technique from the outset reduces anxiety and minimizes the risk of injection-related complications.
Administering semaglutide correctly ensures optimal medication delivery and reduces discomfort. The injection process typically takes just a few minutes once you become familiar with the steps. Always perform injections in a clean, well-lit area where you can comfortably access your supplies.
Gather your supplies:
Semaglutide pen (at room temperature)
Alcohol swab
FDA-approved sharps disposal container
Gauze or cotton ball (optional)
For Ozempic (multi-dose pen):
Step 1: Wash your hands thoroughly with soap and water for at least 20 seconds.
Step 2: Remove the pen cap and inspect the medication through the viewing window. The solution should be clear and colorless. Do not use if the liquid appears cloudy, discolored, or contains particles.
Step 3: Attach a new needle to the pen. Remove both the outer and inner needle caps. Never reuse needles.
Step 4: For first-time use only, prime the pen. Turn the dose selector to the flow check symbol, point the needle upward, and press the dose button until a drop appears at the needle tip.
Step 5: Select your prescribed dose by turning the dose selector until the correct number appears in the dose window. Double-check the dose before proceeding.
Step 6: Clean your chosen injection site with an alcohol swab using a circular motion. Allow the area to air dry completely.
Step 7: Pinch a fold of skin gently between your thumb and forefinger. Insert the needle at a 90-degree angle. Release the skin fold after insertion.
Step 8: Press and hold the dose button until the dose counter shows "0." Continue holding for at least 6 seconds to ensure complete medication delivery.
Step 9: Release the dose button and withdraw the needle straight out.
Step 10: Carefully place the outer needle cap back on the needle, then unscrew and discard the needle in a sharps container. Replace the pen cap.
For Wegovy (single-dose disposable pen):
Step 1: Wash your hands thoroughly with soap and water.
Step 2: Inspect the pen through the viewing window. The solution should be clear and colorless. Check the expiration date.
Step 3: Clean your chosen injection site with an alcohol swab. Allow to air dry completely.
Step 4: Remove the pen cap. You will hear a click. Do not reattach the cap or touch the needle guard.
Step 5: Press and hold the pen firmly against your skin at a 90-degree angle. You will hear a click when the injection begins.
Step 6: Continue holding the pen against your skin until the yellow bar in the window stops moving completely. This may take up to 10 seconds.
Step 7: Lift the pen straight away from your skin. The needle guard will cover the needle automatically.
Step 8: Discard the used pen in an FDA-approved sharps container.
Never share your semaglutide pen or needles with another person, even if the needle has been changed, as this poses serious infection risks. For safe disposal of used needles and pens, follow local regulations or visit the FDA's website for guidance on proper sharps disposal.
Proper injection site selection and rotation are critical for maintaining medication effectiveness and preventing lipohypertrophy—abnormal fat tissue buildup that can occur with repeated injections in the same location. Semaglutide is administered subcutaneously, meaning the medication is delivered into the fatty tissue layer between skin and muscle.
FDA-approved injection sites include:
Abdomen: Offers a large surface area for injections. Inject at least 2 inches away from the navel and avoid the area within 2 inches of any scars or the waistline.
Thigh: Use the front and outer areas of the thigh, midway between the hip and knee. Avoid the inner thigh, where major blood vessels and nerves are located.
Upper arm: The outer back area of the upper arm, where there is sufficient subcutaneous tissue. This site may require assistance from another person, as it can be challenging to pinch the skin and inject simultaneously while maintaining proper technique.
Rotation strategy is essential for preventing injection site complications. Divide each approved area into quadrants and use a different quadrant each week, creating a systematic rotation pattern. For example, if injecting in the abdomen, you might use the upper right quadrant one week, lower right the next, then lower left, and upper left, before returning to the starting position. This approach allows each site approximately four weeks to recover between injections.
Avoid injecting into areas that are:
Bruised, tender, red, or hard
Scarred or damaged
Within 2 inches of a previous injection site from the same week
Areas with stretch marks, moles, or tattoos
While some patients may notice subjective differences between sites, the FDA-approved labeling does not designate any site as preferred over others. Consistency in your approach—using a systematic rotation pattern—helps prevent injection site complications and may contribute to more predictable results.
Keep a simple log of injection sites, either in a notebook or smartphone app. This practice helps ensure proper rotation and can be valuable information if you experience injection site reactions or need to troubleshoot issues with your healthcare team.
Even experienced patients occasionally make injection errors that can affect medication delivery or cause discomfort. Understanding common mistakes helps you maintain proper technique and achieve optimal treatment outcomes.
Injecting cold medication: Using semaglutide directly from the refrigerator is one of the most frequent errors. Cold medication typically causes more injection site discomfort. Always remove the pen from refrigeration 15–30 minutes before injection, allowing it to reach room temperature naturally. Never attempt to warm the pen artificially using hot water, microwaves, or direct sunlight, as heat can degrade the medication.
Reusing needles: Some patients reuse needles to save money or reduce waste, but this practice carries significant risks. Reused needles become dull, causing more tissue trauma and pain. They may also harbor bacteria, increasing infection risk, and can introduce air bubbles into the pen, affecting dose accuracy. Always use a fresh needle for each injection.
Inadequate hold time: For Ozempic, removing the needle before the full 6-second hold time is complete can result in incomplete dose delivery. For Wegovy, removing the pen before the yellow indicator stops moving can lead to underdosing. Follow the specific instructions for your device to ensure complete dose delivery.
Injecting into muscle: Inserting the needle too deeply or failing to pinch the skin can result in intramuscular rather than subcutaneous injection. This may cause increased pain. Always pinch a fold of skin when needed and insert at the appropriate angle for your body type and needle length. Very lean individuals may need to inject at a 45-degree angle to ensure subcutaneous delivery.
Skipping the air shot (priming): For Ozempic, failing to prime the pen before first use can result in air in the needle, leading to inaccurate dosing. Note that Wegovy pens should not be primed.
Injecting through clothing: Never inject through clothing, even thin fabric. This introduces contaminants and prevents proper skin preparation with alcohol.
Rubbing the injection site: Massaging or rubbing the site after injection may affect medication absorption. Simply apply gentle pressure if bleeding occurs.
Inconsistent timing: While semaglutide offers flexibility in administration time, maintaining consistency helps establish a routine and reduces the likelihood of missed doses. Choose a day and approximate time that fits your schedule, and set a reminder on your phone.
Not checking the dose window (Ozempic): Always verify the dose before injection. Administering the wrong dose could affect your treatment. Significant overdose, particularly when used with insulin or sulfonylureas, could potentially lead to hypoglycemia.
Missing doses: If you miss a dose of Ozempic, take it within 5 days of the missed dose. For Wegovy, take the missed dose as soon as possible if it's at least 48 hours before your next scheduled dose. Otherwise, skip the missed dose and resume your regular schedule.
If you realize you've made an error, contact your healthcare provider for guidance rather than attempting to correct it yourself. For example, if you're unsure whether you received the full dose, do not administer additional medication without medical advice.
Semaglutide is generally well-tolerated, but like all medications, it can cause side effects. Most adverse effects are gastrointestinal and typically diminish over time as your body adjusts to the medication. Understanding what to expect and when to seek medical attention ensures safe treatment.
Common gastrointestinal side effects include nausea, vomiting, diarrhea, constipation, and abdominal pain. These effects are usually mild to moderate and most pronounced when initiating therapy or increasing doses. The gradual dose escalation schedule is specifically designed to minimize these symptoms.
Management strategies for GI side effects:
Eat smaller, more frequent meals rather than large portions
Avoid high-fat, greasy, or spicy foods
Stay well-hydrated, especially if experiencing vomiting or diarrhea
Eat slowly and stop when you feel comfortably satisfied
Avoid lying down immediately after eating
Consider ginger tea or other natural remedies for nausea (discuss with your provider first)
Injection site reactions such as redness, itching, or mild swelling may occur. These reactions are usually self-limited and resolve within a few days. Proper injection technique and site rotation minimize these occurrences. If reactions persist beyond 3–4 days or worsen, contact your healthcare provider.
Hypoglycemia risk is low with semaglutide monotherapy because its glucose-lowering effect is glucose-dependent. However, when combined with insulin or sulfonylureas, the risk increases significantly. Symptoms include shakiness, sweating, confusion, rapid heartbeat, and hunger. If you experience hypoglycemia, follow the ADA's 15-15 rule: consume 15 grams of fast-acting carbohydrates, wait 15 minutes, and recheck blood glucose. Repeat if necessary.
Serious side effects requiring immediate medical attention:
Pancreatitis: Severe, persistent abdominal pain that may radiate to the back, often accompanied by nausea and vomiting. This is a medical emergency requiring immediate evaluation.
Gallbladder problems: Right upper abdominal pain, fever, yellowing of skin or eyes (jaundice), or clay-colored stools may indicate cholecystitis or cholelithiasis.
Kidney problems: Decreased urination, swelling in legs or feet, unusual fatigue, or confusion may indicate acute kidney injury, particularly in patients experiencing severe vomiting or diarrhea leading to dehydration.
Severe allergic reactions: Difficulty breathing, severe rash, swelling of face or throat, or rapid heartbeat require emergency care (call 911).
Vision changes: New or worsening vision problems, particularly in patients with pre-existing diabetic retinopathy, should be evaluated promptly by an ophthalmologist.
Thyroid nodules: Any neck lump, hoarseness, difficulty swallowing, or shortness of breath should be evaluated, given the theoretical thyroid cancer risk.
Contact your healthcare provider within 24 hours if you experience:
Persistent vomiting preventing adequate fluid intake
Signs of dehydration (dark urine, dizziness, dry mouth)
Severe or worsening abdominal pain
Recurrent hypoglycemia
Depression or suicidal thoughts (rare but reported with Wegovy)
Persistent resting heart rate increases with symptoms like dizziness or chest pain
Pregnancy while taking semaglutide (stop Wegovy immediately)
Maintain open communication with your healthcare team throughout treatment. Many side effects can be managed with dose adjustments, timing modifications, or supportive care measures. Never discontinue semaglutide abruptly without medical guidance, as this may affect your diabetes control or weight management progress. Your provider can help determine whether side effects warrant dose reduction, temporary discontinuation, or alternative treatment strategies.
Semaglutide can be injected into three FDA-approved sites: the abdomen (at least 2 inches from the navel), the front and outer thigh, or the outer back area of the upper arm. Rotate between these sites weekly to prevent tissue complications.
For Ozempic, press and hold the dose button for at least 6 seconds after the dose counter reaches zero. For Wegovy, keep the pen pressed against your skin until the yellow bar stops moving completely, which may take up to 10 seconds.
For Ozempic, administer the missed dose within 5 days; otherwise, skip it and resume your regular schedule. For Wegovy, take the missed dose as soon as possible if at least 48 hours remain before your next scheduled dose; otherwise, skip it and continue with your regular weekly schedule.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.