LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is a GLP-1 receptor agonist widely prescribed for type 2 diabetes and weight management. As more patients use this medication, questions arise about its safety during dental procedures. While semaglutide does not contraindicate dental work, its effect on gastric emptying requires specific considerations, particularly for procedures involving sedation or anesthesia. Understanding how to safely coordinate dental care with semaglutide therapy ensures optimal outcomes and minimizes risks. This guide provides evidence-based recommendations for patients and healthcare providers navigating dental procedures while on semaglutide treatment.
Quick Answer: Patients taking semaglutide can safely undergo dental procedures, though procedures requiring sedation may need individualized risk assessment due to delayed gastric emptying.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. It is marketed under brand names including Ozempic and Rybelsus for diabetes, and Wegovy for weight management. This medication mimics the action of the naturally occurring hormone GLP-1, which plays a crucial role in glucose regulation and appetite control.
The mechanism of action involves several physiological pathways. Semaglutide stimulates insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning it promotes insulin release primarily when blood glucose levels are elevated. Simultaneously, it suppresses glucagon secretion, reducing hepatic glucose production. Semaglutide slows gastric emptying, which prolongs the sensation of fullness after eating and contributes to reduced caloric intake. This effect on gastric emptying may attenuate with chronic therapy, though patients with active gastrointestinal symptoms may still have higher residual gastric content risk.
The medication also acts on appetite centers in the brain, reducing hunger signals and food cravings. Semaglutide is administered either as a once-weekly subcutaneous injection (Ozempic, Wegovy) or as a daily oral tablet (Rybelsus). The injectable formulations have a half-life of approximately one week, meaning the drug remains active in the body for an extended period.
Common adverse effects include nausea, vomiting, diarrhea, constipation, and abdominal pain, particularly during dose escalation. These gastrointestinal effects are dose-dependent, most prominent during the initial weeks of therapy, and may lessen over time. These effects are directly related to the medication's impact on gastric motility and are relevant considerations when planning dental procedures that may require fasting or sedation.
Yes, patients taking semaglutide can safely undergo dental procedures, but specific considerations may be necessary, particularly for procedures requiring sedation or anesthesia. There is no official contraindication to dental work while taking semaglutide, and the medication does not need to be discontinued for routine dental cleanings, examinations, or minor procedures performed under local anesthesia alone.
For procedures requiring moderate to deep sedation or general anesthesia, current multi-society guidance (2024) from the American Society of Anesthesiologists (ASA) and partner organizations indicates that most patients can continue GLP-1 receptor agonists perioperatively. The primary concern relates to the potential risk of pulmonary aspiration due to delayed gastric emptying, as gastric contents could be regurgitated and aspirated into the lungs during sedation.
Risk factors that warrant additional consideration include:
Being in the dose-escalation phase of semaglutide therapy
Experiencing significant gastrointestinal symptoms (nausea, vomiting, fullness)
Taking higher doses of the medication
Having known gastroparesis or diabetic autonomic neuropathy
For routine dental procedures such as cleanings, fillings, or simple extractions performed with local anesthesia only, semaglutide does not pose additional risks, and patients can continue their regular medication schedule. However, patients should inform their dentist about all medications, including semaglutide, during their medical history review.
For procedures requiring sedation, coordination between the patient, dentist, anesthesia provider, and prescribing physician ensures appropriate risk assessment. For higher-risk patients, strategies may include a 24-hour liquid-only diet before the procedure, point-of-care gastric ultrasound where available, airway-protective techniques, or deferring the procedure until symptoms resolve. If any temporary adjustment to semaglutide therapy is considered, this should be coordinated with the prescribing physician, especially for patients with diabetes who may need alternative glucose management strategies.
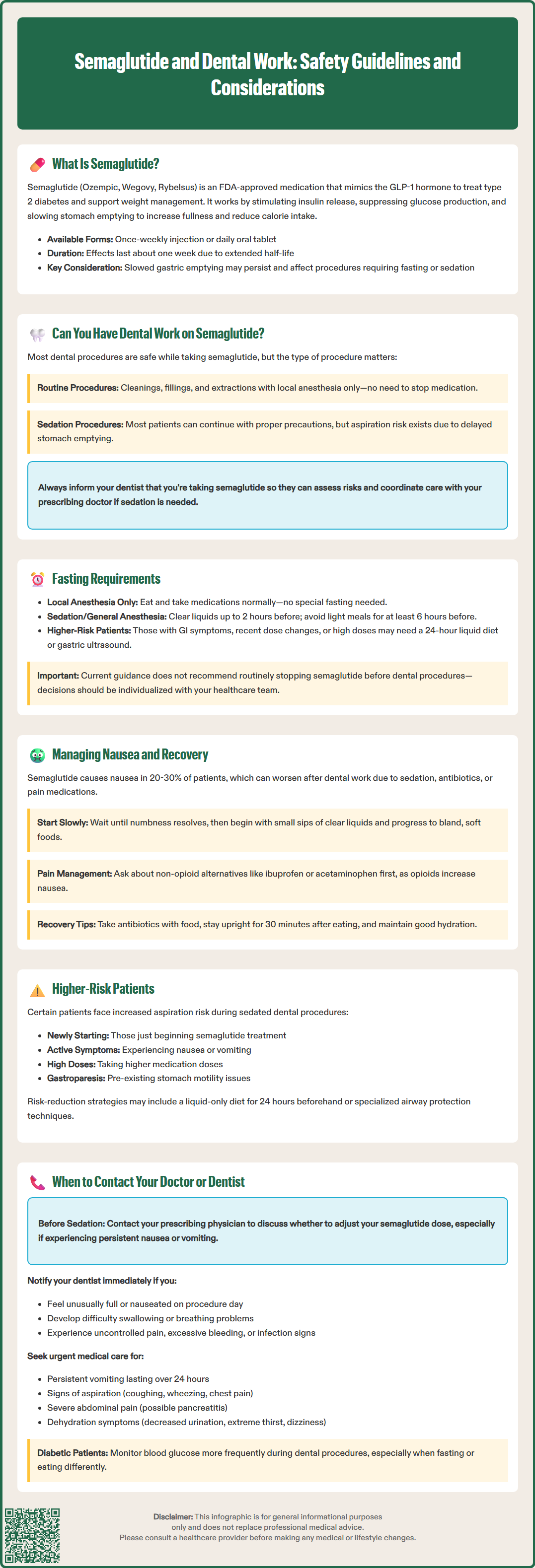
Fasting requirements for dental procedures in patients taking semaglutide should follow standard guidelines with potential individualization based on risk assessment. For procedures requiring only local anesthesia, no special fasting is typically necessary, and patients can eat and take medications as usual before their appointment.
For procedures involving sedation or general anesthesia, standard ASA fasting guidelines generally apply for most patients:
Clear liquids are allowed up to 2 hours before sedation
Light meals should be avoided for at least 6 hours before the procedure
For patients identified as higher risk (those with active GI symptoms, in dose escalation, on high doses, or with known motility disorders), the anesthesia provider may recommend additional precautions such as:
A 24-hour liquid-only diet before the procedure
Point-of-care gastric ultrasound assessment where available
Airway-protective strategies during sedation
Patients should follow their dental provider's specific instructions, which may include:
Taking essential medications (such as blood pressure or heart medications) with small sips of water as directed
Maintaining adequate hydration with clear liquids up to the allowed time before the procedure
Discussing any active GI symptoms with the dental team before sedation
Current multi-society guidance does not recommend routinely holding semaglutide before procedures. Decisions about medication timing should be individualized based on the patient's specific situation and made in consultation with the healthcare team.
It is essential that patients communicate openly with their dental team about their last meal, any symptoms of nausea or fullness, and their medication schedule. If a patient feels unusually full or nauseated on the day of a planned sedation procedure, the dental team should be notified immediately, as this may indicate retained gastric contents and could warrant rescheduling the procedure for safety reasons.
Post-dental procedure recovery can be more challenging for patients taking semaglutide due to the medication's gastrointestinal effects. Nausea is one of the most common adverse effects of semaglutide, affecting up to 20-30% of patients, and this can be exacerbated by dental procedures, particularly those involving sedation, antibiotics, or pain medications.
Immediate post-procedure management should focus on gradual reintroduction of food and fluids. After dental work, especially procedures involving local anesthesia, patients should wait until numbness has completely resolved before eating to avoid accidentally biting the cheek or tongue. When ready to eat, start with small sips of clear liquids such as water or ice chips, progressing slowly to avoid triggering nausea.
For the first 24-48 hours after dental procedures, consider these strategies:
Eat small, frequent meals rather than large portions
Choose bland, soft foods such as yogurt, applesauce, mashed potatoes, or smoothies
Avoid fatty, fried, or spicy foods that may worsen nausea
Stay upright for at least 30 minutes after eating
Take pain medications with food when possible to minimize gastric irritation
If prescription pain medications (such as opioids) are necessary after dental surgery, be aware that these can further slow gastric emptying and worsen nausea when combined with semaglutide. Discuss with your dentist whether non-opioid alternatives such as ibuprofen or acetaminophen might be sufficient for pain control, in line with current CDC guidelines for a nonopioid-first approach. If opioids are required, take the lowest effective dose and consult your healthcare provider about appropriate anti-nausea medications if needed.
Antibiotic therapy following dental procedures may also contribute to gastrointestinal upset. Taking antibiotics with food (unless specifically contraindicated) may help minimize additional nausea. Some patients may benefit from specific probiotic strains to help prevent antibiotic-associated diarrhea, though evidence varies by strain and indication—discuss this option with your healthcare provider. Maintain adequate hydration throughout recovery, as dehydration can worsen both nausea and healing. If persistent vomiting occurs, contact your healthcare provider, as this may require temporary adjustment of your semaglutide dose or additional anti-emetic therapy.
Certain symptoms or situations warrant prompt communication with your healthcare providers when undergoing dental work while taking semaglutide. Understanding these warning signs helps ensure safe treatment and recovery.
Before the dental procedure, contact your prescribing physician if:
You have a procedure requiring sedation scheduled and are unsure whether to adjust your semaglutide dose
You are experiencing persistent nausea or vomiting that might indicate retained gastric contents
You have concerns about fasting requirements given your diabetes management needs
You need guidance on managing blood glucose during fasting periods
Contact your dentist immediately if:
You feel unusually full or nauseated on the day of a scheduled sedation procedure
You experience difficulty swallowing or breathing after dental work
You develop severe or worsening pain not controlled by prescribed medications
You notice excessive bleeding that does not stop with pressure
You develop signs of infection including fever, increasing swelling, or pus drainage
Seek urgent medical attention for:
Persistent vomiting lasting more than 24 hours after dental work, especially if unable to keep down fluids or medications
Signs of aspiration including coughing, wheezing, chest pain, or difficulty breathing following sedation (call 911 for severe breathing problems)
Severe abdominal pain that is new or different from typical semaglutide-related discomfort, especially if persistent and radiating to the back (which may indicate pancreatitis)
Signs of gallbladder disease including severe pain in the upper right abdomen, fever, or yellowing of the skin or eyes
Signs of dehydration including decreased urination, extreme thirst, dizziness, or confusion
Uncontrolled blood glucose levels in diabetic patients, particularly if unable to eat normally
For patients with diabetes, monitoring blood glucose more frequently during the peri-procedural period is advisable, especially if fasting or dietary changes are required. Your physician may provide specific guidance on adjusting diabetes medications during this time. Maintaining open communication between your dentist, physician, and yourself ensures coordinated care and optimal safety throughout your dental treatment while taking semaglutide.
No, current multi-society guidance does not recommend routinely stopping semaglutide before dental procedures. For routine dental work with local anesthesia, continue your regular medication schedule. For procedures requiring sedation, your healthcare team will assess individual risk factors and determine if any modifications are needed.
Semaglutide slows gastric emptying, which may increase the risk of pulmonary aspiration during sedation or general anesthesia. However, most patients can safely undergo sedation with appropriate fasting protocols and risk assessment, particularly if they are not experiencing active gastrointestinal symptoms.
Start with small sips of clear liquids after numbness resolves, then progress to bland, soft foods like yogurt, applesauce, or mashed potatoes. Eat small, frequent meals and avoid fatty, fried, or spicy foods for 24-48 hours to minimize nausea and support healing.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.