LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide, a GLP-1 receptor agonist approved for type 2 diabetes and weight management, is frequently prescribed alongside thyroid medications like levothyroxine. Many patients with diabetes or obesity also have hypothyroidism, making this combination common in clinical practice. While these medications work through different mechanisms—semaglutide via incretin pathways and levothyroxine through thyroid hormone replacement—understanding their potential interactions is essential for safe, effective treatment. This article examines the compatibility of semaglutide and thyroid medication, addressing FDA warnings, monitoring requirements, and practical considerations for patients taking both therapies concurrently.
Quick Answer: Semaglutide can generally be taken safely with thyroid medications like levothyroxine, though proper timing, monitoring, and awareness of FDA warnings are essential.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand names Ozempic for injection and Rybelsus for oral tablets) and chronic weight management (as Wegovy). It works by mimicking the incretin hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. These mechanisms contribute to improved glycemic control and significant weight loss in appropriate patient populations.
Thyroid medications, primarily levothyroxine, are prescribed to manage hypothyroidism—a condition where the thyroid gland produces insufficient thyroid hormone. Levothyroxine is a synthetic form of thyroxine (T4) that restores normal thyroid hormone levels, regulating metabolism, energy production, and numerous physiological processes. According to the National Institute of Diabetes and Digestive and Kidney Diseases (NIDDK), hypothyroidism affects approximately 5% of the US population (including both overt and subclinical cases), with higher prevalence among women and older adults.
Many patients with type 2 diabetes or obesity also have concurrent thyroid disorders, making the combination of semaglutide and thyroid medication a common clinical scenario. Understanding how these medications work independently is essential before examining their potential interactions. Both medications play critical roles in metabolic regulation, though through entirely different mechanisms—semaglutide through incretin pathways and thyroid hormone through nuclear receptor-mediated gene transcription. The question of whether these agents can be safely used together requires careful consideration of pharmacological properties, clinical evidence, and FDA guidance regarding thyroid-related safety concerns specific to GLP-1 receptor agonists.
Yes, semaglutide can generally be taken concurrently with thyroid medications such as levothyroxine, though specific considerations apply based on the formulation of semaglutide used. Injectable semaglutide (Ozempic, Wegovy) and oral levothyroxine have no direct pharmacokinetic interactions that would prevent co-administration, but proper timing and monitoring are important.
Levothyroxine is absorbed primarily in the small intestine, with peak absorption occurring 2-4 hours after oral administration. It has a long half-life of approximately 7 days, allowing for once-daily dosing. As a narrow therapeutic index medication, consistent administration and absorption are critical for maintaining stable thyroid levels. Injectable semaglutide, administered subcutaneously once weekly, has a half-life of approximately one week and reaches steady-state concentrations after 4-5 weeks of treatment.
However, important considerations exist. The FDA labeling for all semaglutide formulations notes that GLP-1 receptor agonists delay gastric emptying, which could affect the absorption of oral medications. For oral semaglutide (Rybelsus), the FDA prescribing information specifically notes increased thyroxine exposure when co-administered with levothyroxine, requiring thyroid parameter monitoring.
The American Thyroid Association recommends taking levothyroxine on an empty stomach, typically 30-60 minutes before breakfast, to optimize absorption. For patients taking oral semaglutide, which also requires administration on an empty stomach with a small amount of water at least 30 minutes before food or other medications, timing conflicts may arise. Alternative options include taking levothyroxine at bedtime (at least 3-4 hours after the last meal) with clinician guidance.
Patients taking both medications should maintain consistent timing of administration and report any symptoms suggesting thyroid dysfunction to their healthcare provider. While co-administration is generally safe with appropriate monitoring, individualized management ensures optimal therapeutic outcomes for both conditions.
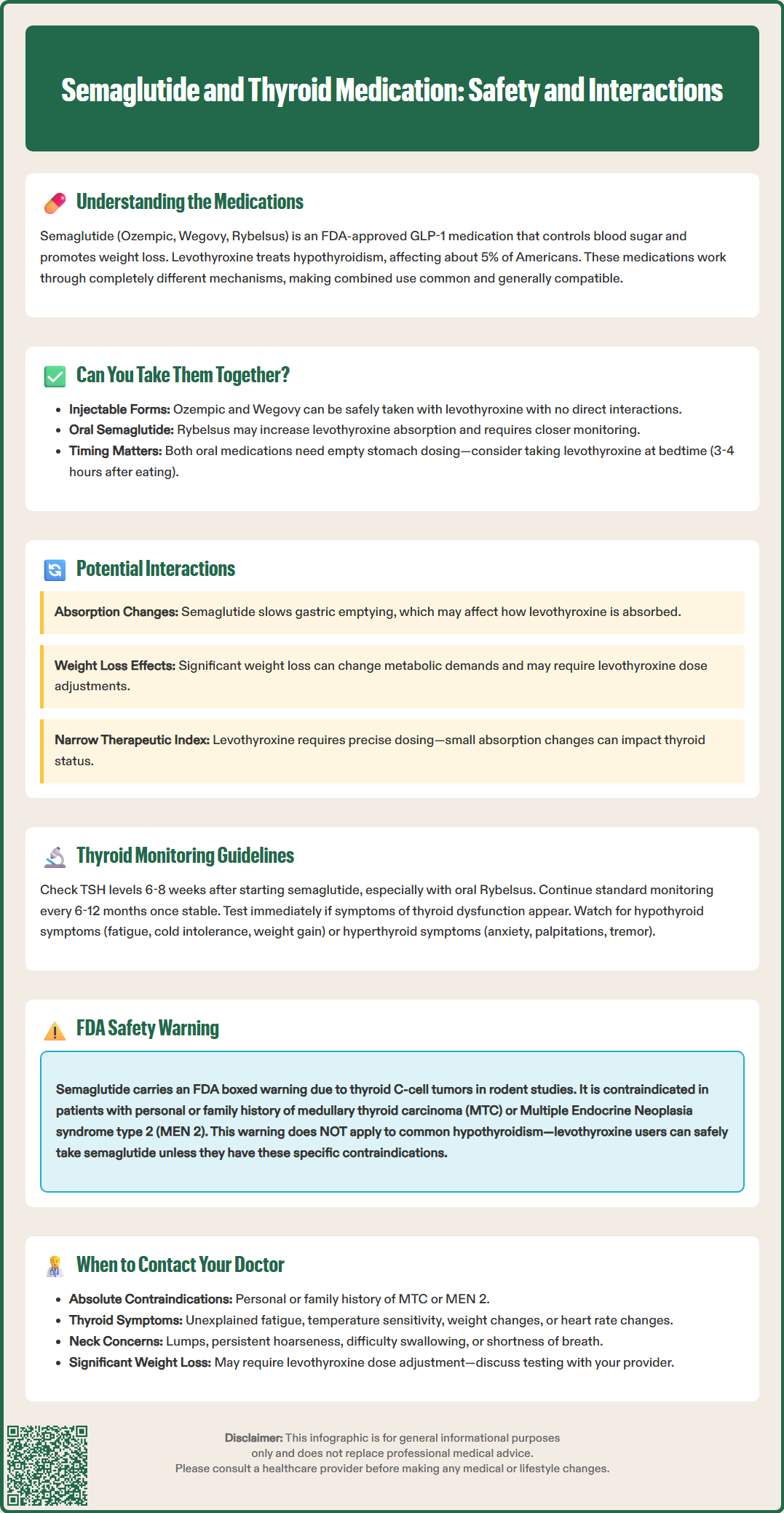
The potential interactions between semaglutide and thyroid medications vary by formulation. For injectable semaglutide (Ozempic, Wegovy), interactions are primarily indirect, while oral semaglutide (Rybelsus) has documented pharmacokinetic interactions with levothyroxine.
Injectable semaglutide's mechanism of slowing gastric emptying could theoretically alter the absorption kinetics of oral levothyroxine. The FDA labeling for all semaglutide products cautions that delayed gastric emptying may impact the absorption of concomitantly administered oral medications. Since levothyroxine is a narrow therapeutic index medication, even modest changes in absorption could affect thyroid status in some patients.
For oral semaglutide (Rybelsus), the FDA prescribing information specifically notes increased thyroxine exposure when co-administered with levothyroxine. This interaction requires monitoring of thyroid parameters when initiating or adjusting either medication.
Weight loss induced by semaglutide may indirectly affect thyroid hormone requirements. As patients lose substantial weight, their metabolic demands change, potentially altering the dose of levothyroxine needed to maintain euthyroid status. Some patients may require levothyroxine dose reductions as they lose weight, while the relationship is not always linear or predictable. This represents a physiological adjustment rather than a true drug interaction.
Timing of medication administration is particularly important. Because levothyroxine absorption can be affected by food and other medications, maintaining a consistent routine is essential. Patients using injectable semaglutide should take levothyroxine at the same time each day, preferably on an empty stomach. For those using oral semaglutide, clinicians should provide specific guidance on scheduling both medications to minimize absorption conflicts while maintaining fasting requirements for both drugs.
There is no evidence that semaglutide affects thyroid hormone synthesis, secretion, or peripheral conversion of T4 to the active form T3. Clinical monitoring remains important to ensure both conditions are adequately controlled and to detect any individual variations in response to therapy.
Patients taking both semaglutide and thyroid medication should undergo regular thyroid function monitoring, following established guidelines for thyroid disease management. The American Thyroid Association recommends checking thyroid-stimulating hormone (TSH) levels 4-6 weeks after initiating levothyroxine or changing doses, then every 6-12 months once stable. This monitoring schedule should be maintained for patients starting semaglutide.
When initiating semaglutide in patients already taking levothyroxine, clinicians may consider checking TSH levels 6-8 weeks after starting treatment, particularly for patients using oral semaglutide (Rybelsus) due to its documented effect on thyroxine exposure. Additional testing may be appropriate after clinically significant weight loss has occurred. This approach helps identify whether levothyroxine dose adjustments are needed due to metabolic changes associated with weight reduction or altered absorption.
Patients should be educated about symptoms of both hypothyroidism (fatigue, cold intolerance, weight gain, constipation) and hyperthyroidism (anxiety, palpitations, heat intolerance, tremor) to facilitate early detection of thyroid dysfunction.
For patients with well-controlled hypothyroidism starting semaglutide, baseline TSH measurement provides a reference point for future comparisons. If symptoms suggestive of thyroid dysfunction develop during semaglutide treatment, thyroid function tests should be obtained promptly rather than waiting for routine monitoring intervals.
Documentation of thyroid medication adherence is important, as non-adherence can confound interpretation of thyroid function tests. Patients should be counseled to maintain consistent timing of levothyroxine administration and to report any gastrointestinal side effects from semaglutide that might affect medication-taking behavior. For patients using oral semaglutide, alternative levothyroxine timing (such as bedtime dosing) may be considered to avoid scheduling conflicts while maintaining consistent absorption. Regular monitoring allows for timely dose adjustments and ensures both diabetes or weight management goals and thyroid function optimization are achieved safely.
The FDA has issued important safety warnings regarding semaglutide and thyroid concerns, specifically related to thyroid C-cell tumors observed in animal studies. In rodent studies, semaglutide caused dose-dependent and treatment-duration-dependent thyroid C-cell tumors at clinically relevant exposures. These findings resulted in a boxed warning in the prescribing information for Ozempic, Wegovy, and Rybelsus, the strongest warning the FDA can require.
The boxed warning states that semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) and in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Healthcare providers should assess for these conditions through medical history before prescribing semaglutide. The FDA does not recommend routine calcitonin measurement or thyroid ultrasound screening, as these have uncertain value and are not recommended for patients taking GLP-1 receptor agonists. Patients should be counseled about the potential risk and instructed to report symptoms of thyroid tumors, including:
A lump or swelling in the neck
Hoarseness or voice changes
Difficulty swallowing
Shortness of breath
It is important to note that the relevance of rodent C-cell tumor findings to humans remains uncertain. Human thyroid C-cells express GLP-1 receptors at much lower levels than rodent C-cells, and there is no established causal relationship between GLP-1 receptor agonists and MTC in humans. Post-marketing surveillance and clinical trial data have not demonstrated an increased incidence of MTC in patients treated with semaglutide compared to control populations, though the FDA notes that human relevance remains unknown.
The FDA warning pertains specifically to medullary thyroid carcinoma, not to common thyroid conditions like hypothyroidism or the use of levothyroxine. Patients taking thyroid hormone replacement for hypothyroidism are not at increased risk from semaglutide unless they have the specific contraindications mentioned above. This distinction is critical for appropriate patient counseling and risk assessment.
Patients taking or considering semaglutide alongside thyroid medication should consult their healthcare provider in several specific circumstances. Before starting semaglutide, a comprehensive medical history should be obtained, including any personal or family history of thyroid cancer, particularly medullary thyroid carcinoma, or Multiple Endocrine Neoplasia syndrome type 2. These conditions represent absolute contraindications to semaglutide use.
Patients should contact their healthcare provider if they develop symptoms suggesting thyroid dysfunction while taking semaglutide. Hypothyroid symptoms include unexplained fatigue, cold intolerance, constipation, dry skin, or unintended weight gain despite continued semaglutide use. Conversely, symptoms of hyperthyroidism—such as anxiety, tremor, palpitations, heat intolerance, or diarrhea—warrant evaluation, as they might indicate excessive thyroid hormone replacement.
Any neck symptoms require prompt medical attention, including a palpable lump, persistent hoarseness, difficulty swallowing, or unexplained shortness of breath. While these symptoms have many potential causes, they require evaluation to rule out thyroid pathology, given the FDA's boxed warning regarding thyroid C-cell tumors.
Significant weight loss achieved with semaglutide may necessitate levothyroxine dose adjustment. Patients who experience substantial or sustained weight loss should discuss thyroid function testing with their provider, even in the absence of symptoms. Additionally, if gastrointestinal side effects from semaglutide (nausea, vomiting) interfere with the ability to take levothyroxine consistently, medical guidance is needed to maintain thyroid control.
Patients taking oral semaglutide (Rybelsus) should discuss medication scheduling with their provider to ensure optimal absorption of both medications, as both require administration on an empty stomach. Alternative timing strategies, such as bedtime levothyroxine dosing, may be considered.
Regular follow-up appointments allow for monitoring of both diabetes or weight management goals and thyroid function. Patients should not adjust doses of either medication independently. Collaborative care between endocrinologists, primary care providers, and other specialists ensures comprehensive management of these complex, interrelated conditions and optimizes both safety and therapeutic outcomes.
Yes, semaglutide can be taken with levothyroxine for hypothyroidism, provided you don't have a personal or family history of medullary thyroid carcinoma or MEN 2 syndrome. Proper timing of medications and regular thyroid monitoring are important to ensure both conditions remain well-controlled.
Semaglutide doesn't directly affect thyroid hormone production, but it may alter levothyroxine absorption through delayed gastric emptying. Additionally, weight loss from semaglutide can change metabolic demands, potentially requiring levothyroxine dose adjustments over time.
The FDA has issued a boxed warning for semaglutide due to thyroid C-cell tumors observed in animal studies. Semaglutide is contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2, though the relevance to humans remains uncertain.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.