LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is a GLP-1 receptor agonist FDA-approved for type 2 diabetes and chronic weight management. While gastrointestinal side effects are most common, some patients report skin sensitivity during treatment. Understanding the relationship between semaglutide and skin-related symptoms—including injection site reactions, potential systemic effects, and when to seek medical attention—is essential for safe medication use. This article examines the evidence for semaglutide side effects related to skin sensitivity, distinguishes documented reactions from patient-reported symptoms, and provides guidance on management and monitoring.
Quick Answer: Generalized skin sensitivity is not a recognized adverse effect in FDA labeling for semaglutide, though injection site reactions occur in 1.4-2.4% of patients using subcutaneous formulations.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the action of endogenous GLP-1, enhancing glucose-dependent insulin secretion, suppressing glucagon release, slowing gastric emptying, and promoting satiety through central nervous system pathways.
Importantly, semaglutide carries a boxed warning for risk of thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, affecting a substantial proportion of patients. These include nausea, vomiting, diarrhea, abdominal pain, and constipation, which typically occur during dose escalation and often diminish over time. According to the FDA prescribing information, these gastrointestinal symptoms are dose-dependent and represent the primary reason for treatment discontinuation in clinical trials.
Beyond gastrointestinal effects, semaglutide carries warnings for more serious but less common adverse events. These include acute pancreatitis, diabetic retinopathy complications in patients with pre-existing retinopathy, acute kidney injury (particularly in the setting of dehydration from gastrointestinal losses), and hypoglycemia when used in combination with insulin or insulin secretagogues. Hypersensitivity reactions, including anaphylaxis and angioedema, have been reported and require immediate medical attention and drug discontinuation. Gallbladder disease, including cholelithiasis and cholecystitis, has also been reported with increased frequency.
While dermatologic reactions are not among the most prominent adverse effects listed in the prescribing information, patients and clinicians have reported various skin-related symptoms during semaglutide therapy. Understanding the spectrum of these reactions and their clinical significance is essential for appropriate patient counseling and management.
Patient reports of skin sensitivity associated with semaglutide use encompass a range of subjective experiences, though there is no officially established causal relationship between semaglutide and generalized skin sensitivity in the FDA-approved labeling. Anecdotal reports from patients describe sensations of increased skin tenderness, heightened sensitivity to touch, or a feeling that the skin is more reactive than usual. Some individuals report that previously tolerated skincare products, fabrics, or environmental factors seem to cause more irritation during semaglutide treatment.
It is important to distinguish between documented adverse effects and patient-reported symptoms that may or may not be directly attributable to the medication. The FDA prescribing information does not list generalized skin sensitivity as a recognized adverse reaction, though injection site reactions are well-documented for the subcutaneous formulations (Ozempic and Wegovy). However, the labeling does recognize specific hypersensitivity reactions including rash and urticaria as potential manifestations of drug hypersensitivity, which are distinct from nonspecific skin sensitivity complaints.
Several mechanisms could theoretically contribute to altered skin sensation or sensitivity during semaglutide therapy, though these remain speculative without robust clinical evidence. Rapid weight loss associated with semaglutide use may lead to changes in skin texture, hydration status, and barrier function. Nutritional deficiencies resulting from reduced caloric intake and altered eating patterns could potentially affect skin health. Additionally, the metabolic changes induced by improved glycemic control might influence peripheral nerve function or microvascular perfusion, though this has not been systematically studied in humans and data remain limited.
Clinicians should approach patient reports of skin sensitivity with appropriate clinical skepticism while remaining attentive to the patient's experience. A thorough history should explore the temporal relationship between medication initiation or dose escalation and symptom onset, the specific nature and distribution of symptoms, and potential alternative explanations including concurrent medications, environmental exposures, or underlying dermatologic conditions.
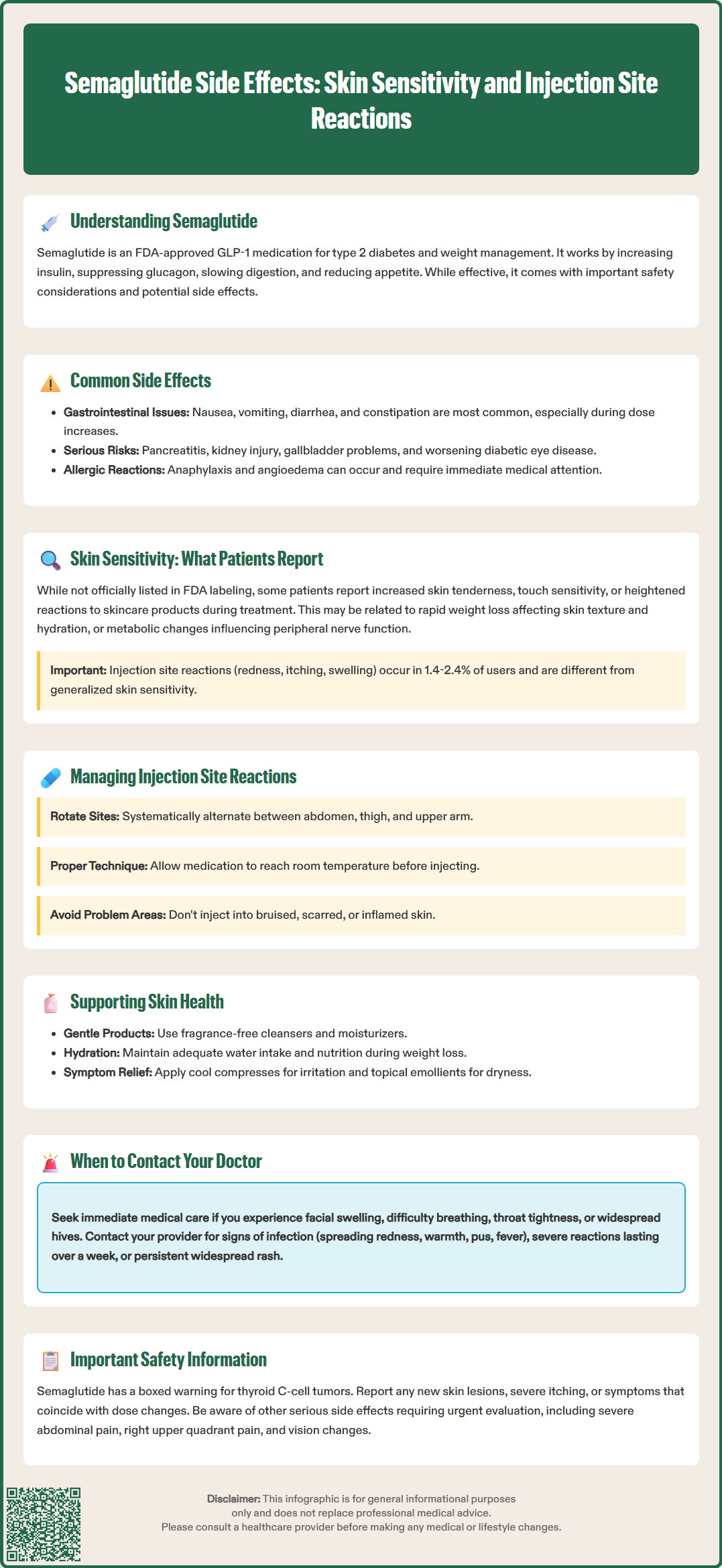
For patients using subcutaneous semaglutide formulations (Ozempic and Wegovy), injection site reactions represent a well-characterized adverse effect that must be distinguished from generalized skin sensitivity. According to the FDA prescribing information, injection site reactions occurred in 1.4% of Ozempic patients and 2.4% of Wegovy patients in clinical trials. These localized reactions typically manifest as erythema, pruritus, swelling, or discomfort at the injection site and are generally mild to moderate in severity.
Injection site reactions are mechanistically distinct from systemic skin sensitivity. Local reactions result from direct tissue trauma, immune response to the injected protein, or irritation from the vehicle components of the formulation. These reactions are spatially confined to the injection area and temporally related to the injection event, usually appearing within hours to days after administration and resolving spontaneously within several days. Proper injection technique, site rotation, and allowing the medication to reach room temperature before injection can minimize these local reactions.
In contrast, systemic skin sensitivity would be expected to present with more diffuse symptoms not limited to injection sites. Patients might describe generalized pruritus, widespread areas of tenderness or hyperesthesia, or skin reactivity in areas distant from injection sites. The temporal pattern may differ as well, with systemic effects potentially developing more gradually or persisting beyond the immediate post-injection period. Distinguishing between these presentations is clinically important because management strategies differ substantially.
Clinicians should conduct a focused dermatologic examination when patients report skin-related symptoms. Documentation should include the distribution and morphology of any visible skin changes, the presence or absence of primary lesions (such as papules, plaques, or vesicles), and assessment of whether findings are limited to injection sites or more widespread. Photographic documentation can be valuable for monitoring progression. If injection site reactions are severe, persistent, or associated with signs of infection (warmth, purulent drainage, systemic symptoms), further evaluation and possible treatment modification may be warranted.
Management of skin sensitivity during semaglutide therapy requires a systematic approach that addresses both local injection site reactions and any reported systemic symptoms. For injection site reactions, patient education on proper injection technique is foundational. Patients should be instructed to rotate injection sites systematically among the abdomen, thigh, and upper arm, avoiding repeated injections in the same location. The medication should be allowed to reach room temperature before injection, and patients should follow the specific Instructions for Use for their device, including proper needle placement and holding the button for the manufacturer-specified time. Patients should avoid injecting into areas with bruising, scars, lipodystrophy, or inflamed skin.
General skin care measures may help patients who report increased skin sensitivity, regardless of whether a direct causal relationship with semaglutide is established. Recommendations include using gentle, fragrance-free cleansers and moisturizers to support skin barrier function, particularly in the context of weight loss which can affect skin hydration. Patients should be advised to avoid harsh skincare products, excessive bathing with hot water, and known irritants. Adequate hydration and nutrition are essential, as rapid weight loss and reduced caloric intake may compromise skin health.
For patients experiencing significant discomfort, symptomatic management may be appropriate. Topical emollients can improve skin barrier function and reduce dryness. If pruritus is prominent, non-sedating antihistamines may provide relief, though evidence for their efficacy in this specific context is limited. Sedating antihistamines should be avoided, particularly in older adults or those who must avoid impairment. Cool compresses can soothe localized irritation at injection sites. Patients should be counseled to avoid scratching, which can lead to secondary skin damage and potential infection.
For signs of systemic hypersensitivity reactions (generalized hives, facial/lip/tongue swelling, breathing difficulty), patients should stop the medication immediately and seek emergency care. These patients should not be rechallenged with semaglutide unless directed by an allergy specialist.
It is important to evaluate whether dose adjustment might be beneficial. If skin symptoms appeared or worsened following dose escalation, discussing with the prescribing provider whether to maintain the current dose longer before further titration, or whether a temporary dose reduction might be appropriate, could be considered. However, any medication adjustment should be clinician-directed and balance symptom management with therapeutic goals for glycemic control or weight management.
Referral to dermatology is warranted for persistent or worsening widespread rash, mucosal involvement, or systemic symptoms. Clinicians should also consider whether alternative explanations for skin symptoms require investigation, including other medications, supplements, environmental factors, stress, or concurrent medical conditions.
Patients taking semaglutide should be educated about specific skin-related symptoms that warrant prompt medical evaluation. While mild injection site reactions are generally self-limited and manageable with conservative measures, certain presentations require clinical assessment to rule out more serious conditions or complications. Clear guidance on when to seek medical attention empowers patients to participate actively in their care while ensuring appropriate safety monitoring.
Patients should contact their healthcare provider if they experience:
Signs of infection at injection sites, including increasing warmth, redness spreading beyond the immediate injection area, purulent drainage, or fever. These findings may indicate cellulitis or abscess formation requiring antibiotic therapy.
Severe or progressive injection site reactions that worsen over time rather than improving, or reactions that persist beyond one week. This pattern may suggest an allergic response or other complication requiring evaluation.
Widespread rash or urticaria (hives), particularly if mild to moderate and not accompanied by other symptoms. Document the timing relative to dose changes.
Patients should SEEK EMERGENCY CARE IMMEDIATELY and STOP taking semaglutide if they experience:
Other reasons to contact a healthcare provider:
New skin lesions or changes in existing moles, especially in the context of any medication use. While not specifically associated with semaglutide, any concerning skin changes warrant dermatologic evaluation.
Severe pruritus that significantly impacts quality of life or sleep, or that does not respond to conservative measures. Persistent, severe itching may indicate an underlying condition requiring investigation.
Patients should also report skin symptoms if they are accompanied by systemic signs such as fever, malaise, joint pain, or other concerning symptoms that might suggest a more serious adverse reaction. The temporal relationship between medication initiation or dose changes and symptom onset should be communicated to the healthcare provider, as this information aids in causality assessment.
For patients with diabetes, any skin changes should be evaluated with particular attention to potential diabetic complications. Diabetic dermopathy, necrobiosis lipoidica, or infections may occur independently of semaglutide use but require appropriate management. Additionally, patients should be reminded that semaglutide carries specific warnings for other serious adverse effects, including pancreatitis (severe abdominal pain), acute gallbladder disease (right upper quadrant pain), and changes in vision, all of which require urgent medical evaluation.
Healthcare providers should establish clear communication channels for patients to report concerns and should conduct regular follow-up assessments, particularly during dose titration periods when adverse effects are most likely to emerge. Serious adverse events should be reported to the FDA MedWatch program (www.fda.gov/medwatch or 1-800-FDA-1088). Documentation of skin-related symptoms in the medical record contributes to post-marketing surveillance and helps build the evidence base regarding the full safety profile of semaglutide in real-world clinical practice.
Generalized skin sensitivity is not listed as a recognized adverse effect in FDA prescribing information for semaglutide. Injection site reactions (erythema, pruritus, swelling) occur in 1.4-2.4% of patients using subcutaneous formulations and are well-documented, localized effects.
Contact your healthcare provider for widespread rash or hives. Seek emergency care immediately and stop semaglutide if you experience facial swelling, difficulty breathing, throat tightness, or hives with systemic symptoms, as these may indicate anaphylaxis.
Rotate injection sites systematically among abdomen, thigh, and upper arm, allow medication to reach room temperature before injection, avoid injecting into bruised or inflamed areas, and follow proper injection technique per the Instructions for Use for your specific device.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.