LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Semaglutide is available in two FDA-approved formulations: oral tablets (Rybelsus) and subcutaneous injections (Ozempic, Wegovy). While both contain the same active medication—a GLP-1 receptor agonist—they differ significantly in delivery method, dosing frequency, absorption, and approved uses. Injectable semaglutide offers once-weekly convenience and generally produces greater reductions in blood sugar and body weight, while oral semaglutide provides a needle-free alternative for patients with type 2 diabetes. Understanding these differences helps patients and clinicians select the most appropriate formulation based on treatment goals, lifestyle preferences, and individual medical needs.
Quick Answer: Injectable semaglutide generally provides greater blood sugar reduction and weight loss than oral tablets, but oral semaglutide offers a needle-free alternative for type 2 diabetes management.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes and, at higher doses, for chronic weight management in adults with obesity or overweight with weight-related comorbidities. This medication is available in two distinct formulations: an oral tablet (Rybelsus) and subcutaneous injections (Ozempic for diabetes, Wegovy for weight management).
The injectable forms were approved first, with Ozempic receiving FDA approval in 2017 for type 2 diabetes and for reducing major adverse cardiovascular events in adults with type 2 diabetes and established cardiovascular disease. Wegovy was approved in 2021 for weight management in adults and was later approved for adolescents aged 12 years and older with obesity. In 2024, Wegovy also received FDA approval for reducing cardiovascular risk in adults with established cardiovascular disease and obesity or overweight. Rybelsus, the oral tablet formulation, was approved in 2019 for type 2 diabetes, representing the first oral GLP-1 receptor agonist available in the United States.
Both formulations contain the same active ingredient—semaglutide—but differ substantially in their delivery mechanism, absorption characteristics, and approved indications. The oral tablet uses a novel absorption enhancer called sodium N-(8-[2-hydroxybenzoyl] amino) caprylate (SNAC) to facilitate absorption across the gastric mucosa, overcoming the challenge that peptide medications typically face when taken by mouth.
Importantly, semaglutide is not indicated for patients with type 1 diabetes or diabetic ketoacidosis. Patients should not use multiple semaglutide products or other GLP-1 receptor agonists concurrently due to potential overlapping effects and increased risk of adverse reactions.
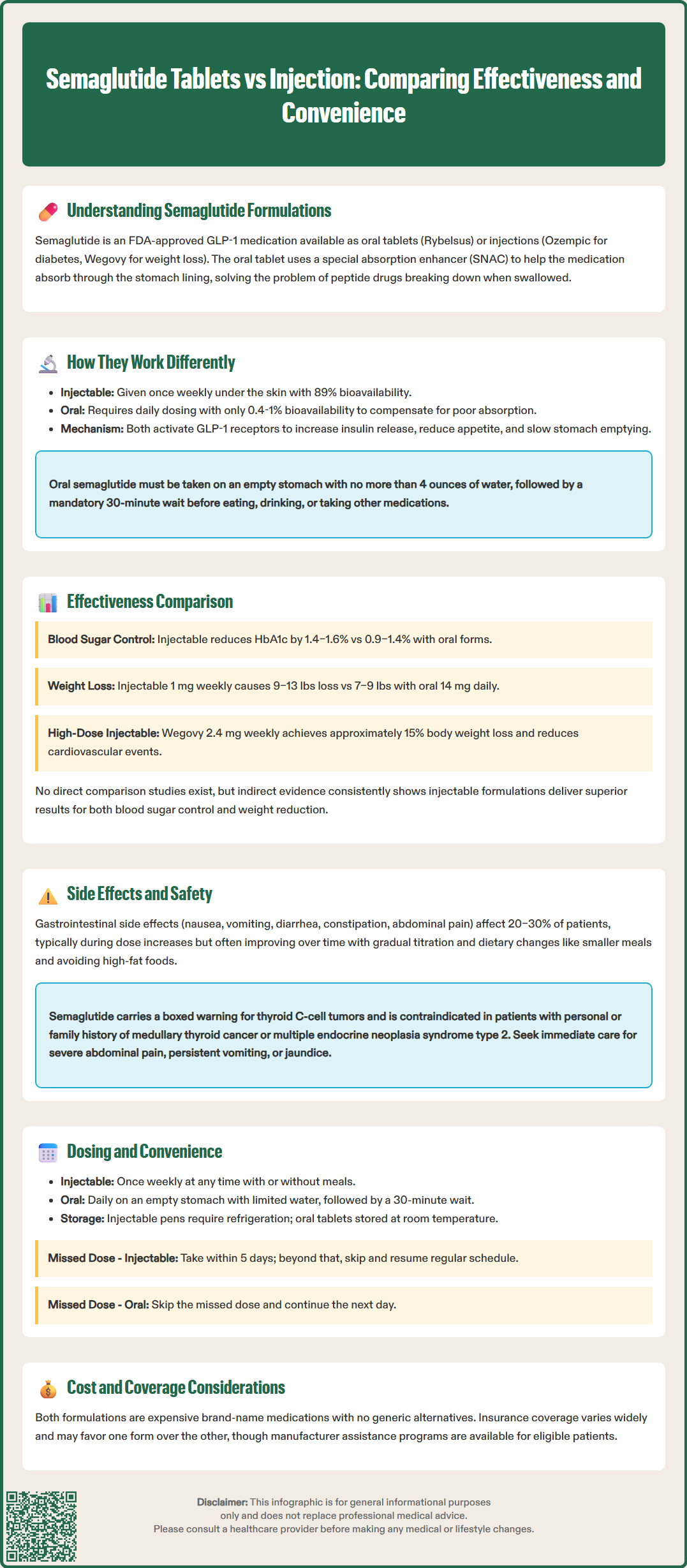
While both formulations contain identical active medication, their pharmacokinetic profiles differ significantly due to their routes of administration. Injectable semaglutide is administered subcutaneously once weekly, allowing for consistent absorption through subcutaneous tissue with predictable bioavailability approaching 89%. The medication has a half-life of approximately one week and reaches steady-state concentrations after approximately 4–5 weeks of weekly dosing, providing sustained GLP-1 receptor activation throughout the week.
Oral semaglutide faces substantial absorption challenges inherent to peptide medications taken by mouth. The SNAC absorption enhancer temporarily increases gastric pH and facilitates transcellular absorption across the stomach lining, but bioavailability remains relatively low at approximately 0.4–1% compared to subcutaneous administration. To compensate for this reduced absorption, oral semaglutide requires daily dosing and must be taken under strict conditions: on an empty stomach with no more than 4 ounces of plain water, with a mandatory 30-minute wait before consuming any food, beverages, or other oral medications. Tablets must be swallowed whole and should never be split, crushed, or chewed.
Despite these pharmacokinetic differences, both formulations work through the same mechanism of action once absorbed. Semaglutide binds to and activates GLP-1 receptors in pancreatic beta cells, enhancing glucose-dependent insulin secretion while suppressing inappropriate glucagon release. Additionally, GLP-1 receptor activation in the central nervous system reduces appetite and food intake, slows gastric emptying, and promotes satiety—mechanisms that contribute to both glycemic control and weight reduction. The delayed gastric emptying may affect the absorption of other oral medications, which should be considered when planning medication administration timing.
Clinical trial data demonstrate that injectable semaglutide generally produces greater reductions in both HbA1c and body weight compared to the oral formulation, though both forms show clinically meaningful benefits. In the SUSTAIN clinical trial program evaluating injectable semaglutide for type 2 diabetes, the 1 mg weekly dose reduced HbA1c by approximately 1.4–1.6% from baseline, while the SUSTAIN FORTE trial showed that the 2 mg dose provided additional glycemic benefits for patients needing intensification. The PIONEER trials examining oral semaglutide showed HbA1c reductions of approximately 0.9–1.4% with the 14 mg daily dose—the highest approved oral dose for diabetes.
Weight loss outcomes similarly favor injectable formulations. In diabetes trials, injectable semaglutide 1 mg produced mean weight loss of 4–6 kg (approximately 9–13 lbs), while oral semaglutide 14 mg resulted in weight loss of approximately 3–4 kg (7–9 lbs). The difference becomes more pronounced with higher-dose injectable semaglutide: Wegovy (2.4 mg weekly) demonstrated mean weight loss of approximately 15% of body weight in the STEP clinical trial program for obesity management, substantially exceeding outcomes typically seen with oral semaglutide at diabetes-approved doses.
It is important to note that oral semaglutide is not currently FDA-approved for weight management as a primary indication, whereas injectable semaglutide has specific approval for chronic weight management at the 2.4 mg dose. The SELECT trial demonstrated that Wegovy 2.4 mg also reduces the risk of major adverse cardiovascular events in adults with established cardiovascular disease and obesity or overweight. While no direct head-to-head trials have compared oral semaglutide with injectable semaglutide at diabetes doses, indirect comparisons across clinical trials suggest that injectable formulations generally provide greater efficacy for both glycemic control and weight reduction.
Both oral and injectable semaglutide share a similar adverse effect profile, with gastrointestinal symptoms representing the most common tolerability concerns. Nausea, vomiting, diarrhea, abdominal pain, and constipation occur frequently with both formulations, typically emerging during dose escalation and often diminishing over time as patients develop tolerance. In clinical trials, approximately 20–30% of patients taking oral semaglutide experienced nausea, with similar or slightly higher rates observed with injectable forms, particularly at higher doses.
The gradual dose titration protocols for both formulations aim to minimize gastrointestinal side effects. Oral semaglutide typically starts at 3 mg daily for 30 days, then increases to 7 mg daily, with optional escalation to 14 mg if additional glycemic control is needed. Injectable semaglutide for diabetes begins at 0.25 mg weekly for four weeks, increasing to 0.5 mg, with possible escalation to 1 mg or 2 mg. Wegovy follows a more extended titration schedule over 16–20 weeks to reach the 2.4 mg maintenance dose. Patients should be counseled that gastrointestinal symptoms are generally transient and can be managed through dietary modifications, including smaller meal portions and avoiding high-fat foods.
Serious adverse effects, though rare, include pancreatitis, gallbladder disease, acute kidney injury (typically secondary to dehydration from gastrointestinal symptoms), and hypoglycemia when combined with insulin or sulfonylureas. Patients should seek immediate medical attention for severe abdominal pain (especially if radiating to the back), persistent vomiting, yellowing of skin/eyes, or signs of allergic reaction. Semaglutide may worsen diabetic retinopathy, particularly in patients with pre-existing retinopathy experiencing rapid improvement in blood glucose; appropriate ophthalmologic monitoring is recommended.
Both formulations carry a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though the clinical relevance to humans remains uncertain. Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Wegovy is contraindicated during pregnancy, and weight loss therapy should be discontinued if pregnancy occurs. Due to semaglutide's long half-life, discontinuation at least 2 months before planned pregnancy should be considered. Caution is advised in patients with severe gastrointestinal disease, including severe gastroparesis.
The choice between oral and injectable semaglutide often hinges on patient preferences, lifestyle factors, and practical considerations beyond clinical efficacy. Injectable semaglutide offers the convenience of once-weekly administration, which many patients find easier to remember and incorporate into their routine compared to daily medications. The pre-filled, single-dose pens are designed for ease of use, requiring minimal training, and can be administered at any time of day with or without meals. Patients can self-inject subcutaneously in the abdomen, thigh, or upper arm, rotating injection sites to minimize local reactions. Used needles should be disposed of in an FDA-cleared sharps container.
If a dose of injectable semaglutide is missed, patients should administer it as soon as possible within 5 days after the missed dose. If more than 5 days have passed, they should skip the missed dose and administer the next dose on the regularly scheduled day. Unopened pens should be refrigerated (36°F to 46°F); after first use, Ozempic pens can be stored at room temperature or refrigerated for up to 56 days, while Wegovy pens are single-use only.
Oral semaglutide requires more stringent adherence to administration instructions. The tablet must be taken daily, first thing in the morning on an empty stomach, with no more than 4 ounces of plain water. Patients must wait at least 30 minutes before eating, drinking anything other than water, or taking other oral medications. If a dose is missed, patients should skip that day's dose and resume the next day. Tablets should be stored at room temperature and swallowed whole. Semaglutide may increase the exposure of medications taken orally, particularly levothyroxine, and appropriate monitoring is recommended.
Cost and insurance coverage represent additional practical considerations. Both formulations are brand-name medications without generic alternatives currently available in the United States, resulting in substantial out-of-pocket costs for patients without adequate insurance coverage. Insurance authorization requirements, prior authorization processes, and formulary placement vary considerably between plans and may favor one formulation over another. Some patients may have coverage for diabetes indications but not weight management, affecting access to higher-dose injectable semaglutide. Patient assistance programs are available through the manufacturer for eligible individuals. Ultimately, shared decision-making between clinicians and patients should weigh clinical effectiveness, side effect profiles, lifestyle compatibility, and financial considerations to determine the most appropriate semaglutide formulation for each individual's circumstances.
Injectable semaglutide, particularly Wegovy at 2.4 mg weekly, produces significantly greater weight loss than oral semaglutide. Oral semaglutide is not FDA-approved for weight management as a primary indication.
Switching between formulations is possible under physician guidance, but patients should not use both forms simultaneously. Your healthcare provider will determine appropriate dosing and timing for the transition based on your treatment goals.
Oral semaglutide contains an absorption enhancer (SNAC) that works best on an empty stomach. Food, beverages, or other medications taken too soon can significantly reduce absorption and effectiveness of the medication.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.