LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While patients may wonder about potential urinary tract infection (UTI) risks, current clinical evidence does not establish a causal link between semaglutide and UTIs. Unlike SGLT-2 inhibitors that increase urinary glucose and infection risk, semaglutide works through different mechanisms. Understanding the relationship between semaglutide and UTI symptoms helps patients distinguish medication side effects from unrelated infections and maintain appropriate vigilance for urinary symptoms requiring medical attention.
Quick Answer: Semaglutide does not cause urinary tract infections based on current FDA prescribing information and clinical trial data.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity. Marketed under brand names including Ozempic, Wegovy, and Rybelsus, semaglutide works by mimicking the action of the naturally occurring hormone GLP-1. This mechanism enhances glucose-dependent insulin secretion, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying, which collectively improves glycemic control and promotes weight loss.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, reflecting its mechanism of action on the digestive system. According to FDA prescribing information, these include nausea, vomiting, diarrhea, abdominal pain, and constipation. These symptoms are typically most pronounced during dose escalation and often diminish over time as the body adjusts to the medication. The FDA-approved prescribing information recommends gradual dose titration to minimize gastrointestinal side effects.
Other notable adverse effects include injection site reactions (for subcutaneous formulations), fatigue, and dizziness. More serious but less common risks include pancreatitis, gallbladder disease, acute kidney injury (particularly in the setting of dehydration from gastrointestinal symptoms), and hypoglycemia when used in combination with insulin or sulfonylureas. Semaglutide is not recommended for patients with severe gastroparesis.
The FDA label carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies. Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Additionally, patients with a history of diabetic retinopathy should be monitored for worsening retinopathy, particularly with rapid improvement in glucose control. Patients should be counseled about these potential risks and the importance of reporting new or worsening symptoms to their healthcare provider.
There is no established causal relationship between semaglutide use and urinary tract infections (UTIs) based on current clinical evidence and FDA-approved prescribing information. Unlike sodium-glucose cotransporter-2 (SGLT-2) inhibitors—another class of diabetes medications—semaglutide does not alter urinary glucose levels or create a glucose-rich environment in the urinary tract that would promote bacterial growth.
SGLT-2 inhibitors have a well-established association with genital mycotic infections, while the evidence for increased UTI risk is mixed. The FDA has issued safety communications regarding rare but serious urinary tract infections with SGLT-2 inhibitors. In contrast, semaglutide works through a different mechanism that does not affect urinary glucose excretion.
Clinical trials evaluating semaglutide safety, including the SUSTAIN and STEP trial programs which enrolled thousands of participants, did not identify UTIs as a significant adverse event associated with the medication. The FDA-approved prescribing information for Ozempic, Wegovy, and Rybelsus does not list UTIs among common or significant adverse reactions.
However, several indirect factors related to semaglutide use may theoretically influence UTI risk in certain circumstances. Dehydration secondary to gastrointestinal side effects (particularly vomiting and diarrhea) can concentrate urine and potentially increase susceptibility to urinary tract infections. Additionally, patients with diabetes—regardless of medication—have baseline increased UTI risk due to factors including impaired immune function, incomplete bladder emptying related to diabetic neuropathy, and historically elevated glucose levels that may have created favorable conditions for bacterial colonization.
It is important to distinguish correlation from causation. If a patient develops a UTI while taking semaglutide, this likely represents coincidental timing rather than a medication-induced effect. UTIs are common, particularly among women, with approximately 50–60% of women experiencing at least one UTI during their lifetime. The temporal association with starting a new medication does not necessarily indicate causality.
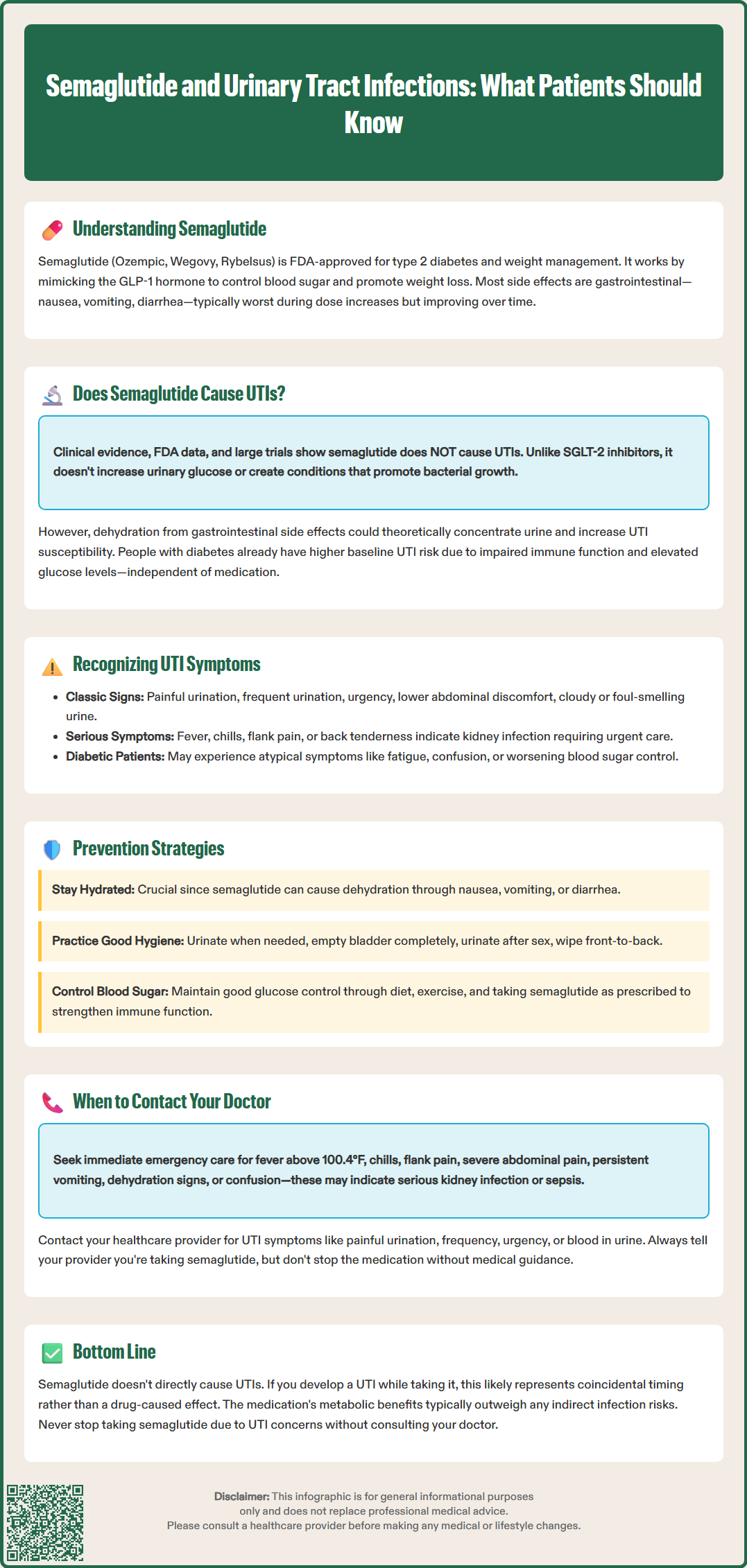
Recognizing urinary tract infection symptoms is essential for all patients, including those taking semaglutide, to ensure prompt diagnosis and treatment. Classic UTI symptoms include dysuria (painful or burning sensation during urination), urinary frequency (needing to urinate more often than usual), urinary urgency (sudden, compelling need to urinate), and suprapubic or lower abdominal discomfort. While patients may also notice cloudy, dark, or foul-smelling urine, or hematuria (blood in the urine), these findings alone are not diagnostic and should be evaluated alongside other symptoms.
For patients taking semaglutide, it is important to distinguish UTI symptoms from medication-related side effects or complications. Abdominal discomfort is common with semaglutide due to its gastrointestinal effects, but UTI-related pain is typically localized to the lower abdomen or suprapubic region and is often accompanied by urinary symptoms. Nausea and vomiting can occur with both upper UTIs (pyelonephritis) and as semaglutide side effects, making differentiation challenging. The presence of fever, chills, flank pain, or costovertebral angle tenderness suggests upper urinary tract involvement (pyelonephritis) and requires urgent medical evaluation.
Patients with diabetes taking semaglutide should be particularly vigilant, as they may experience atypical or less pronounced symptoms due to diabetic neuropathy affecting sensory perception. Some individuals may present with nonspecific symptoms such as increased fatigue, confusion (particularly in older adults), or worsening glycemic control without classic urinary symptoms.
Women are at substantially higher risk for UTIs than men due to anatomical differences, with shorter urethral length facilitating bacterial ascent into the bladder. Postmenopausal women face additional risk due to estrogen deficiency affecting urogenital tissue. Men presenting with UTI symptoms warrant careful evaluation, as UTIs in men are generally considered complicated infections and may indicate underlying urological abnormalities such as prostatic hypertrophy or urinary retention requiring further investigation.
It's important to note that asymptomatic bacteriuria (bacteria in the urine without symptoms) generally should not be treated in most non-pregnant adults, as per Infectious Diseases Society of America (IDSA) guidelines.
While semaglutide does not directly increase UTI risk, patients can implement evidence-based strategies to minimize infection likelihood during treatment. Maintaining adequate hydration is paramount, particularly given semaglutide's gastrointestinal side effects. Patients should aim for sufficient fluid intake to produce pale yellow urine, with needs varying based on individual factors, activity level, and climate. Those experiencing nausea, vomiting, or diarrhea should be especially attentive to hydration status and may benefit from oral rehydration solutions containing electrolytes.
If patients experience persistent vomiting or inability to maintain adequate hydration while taking semaglutide, they should contact their healthcare provider promptly. In cases of severe dehydration, temporary adjustment or interruption of semaglutide may be necessary, along with monitoring of renal function.
Standard UTI prevention measures remain important for all patients. These include urinating when the urge arises rather than delaying, ensuring complete bladder emptying, and urinating shortly after sexual intercourse to flush bacteria from the urethra. Women should practice front-to-back wiping after bowel movements to prevent bacterial contamination from the rectal area. Avoiding potentially irritating feminine hygiene products, douches, and harsh soaps in the genital area helps maintain normal protective flora.
For patients with diabetes, optimizing glycemic control reduces UTI risk by improving immune function and eliminating glucosuria that can promote bacterial growth. Regular monitoring of blood glucose levels and adherence to the complete diabetes management plan—including semaglutide as prescribed, dietary modifications, and physical activity—supports overall metabolic health and infection resistance.
Patients with recurrent UTIs (defined as two or more infections in six months or three or more in one year) should discuss preventive strategies with their healthcare provider. Options may include low-dose prophylactic antibiotics, postcoital antibiotic prophylaxis for women with intercourse-related infections, or vaginal estrogen therapy for postmenopausal women. Methenamine hippurate is an antibiotic-sparing option for some patients with recurrent UTIs. Cranberry products may offer modest benefit for recurrent UTI prevention according to the American Urological Association (conditional recommendation), but should not replace proven strategies. Patients should not discontinue semaglutide due to UTI concerns without consulting their prescribing physician, as the metabolic benefits typically outweigh any theoretical indirect risks.
Patients taking semaglutide should contact their healthcare provider promptly if they develop symptoms suggestive of a urinary tract infection. Dysuria, urinary frequency, urgency, suprapubic pain, or visible blood in the urine warrant medical evaluation, typically beginning with urinalysis and, when indicated, urine culture to confirm infection and guide antibiotic selection. Early treatment prevents progression to more serious upper urinary tract infection and reduces symptom duration.
Certain presentations require urgent or emergency medical attention. Patients should seek immediate care if they develop fever (temperature ≥100.4°F or 38°C), chills, flank pain, severe abdominal pain, persistent vomiting preventing oral intake, signs of dehydration (decreased urination, dark urine, dizziness, dry mouth), or altered mental status. These symptoms may indicate pyelonephritis, sepsis, or severe dehydration requiring intravenous antibiotics and fluids.
Patients with diabetes are at increased risk for complicated infections and should have a lower threshold for seeking medical evaluation. UTIs in men, pregnant women, and patients with significant comorbidities or immunosuppression are generally considered complicated infections requiring prompt medical attention and potentially different management approaches.
Patients should also contact their healthcare provider if UTI symptoms do not improve within 48–72 hours of starting antibiotic therapy, or if symptoms recur shortly after completing treatment. Persistent or recurrent infections may indicate antibiotic resistance, inadequate treatment duration, or underlying urological abnormalities requiring further investigation with imaging studies or urology referral.
It is important to inform healthcare providers about all medications, including semaglutide, when presenting with infection symptoms. While semaglutide does not cause UTIs, the medication context helps providers assess overall clinical status, consider potential drug interactions with antibiotics, and evaluate whether gastrointestinal side effects have contributed to dehydration. Patients should never discontinue semaglutide without medical guidance, as abrupt cessation can lead to worsening glycemic control. Healthcare providers can help patients navigate concurrent illness management while maintaining diabetes treatment continuity and adjusting therapy as needed based on individual circumstances.
No, semaglutide does not increase UTI risk based on FDA prescribing information and clinical trials. Unlike SGLT-2 inhibitors, semaglutide does not affect urinary glucose levels or create conditions that promote bacterial growth in the urinary tract.
Contact your healthcare provider promptly if you experience dysuria, urinary frequency, urgency, or suprapubic pain. Seek immediate care for fever, chills, flank pain, or persistent vomiting, as these may indicate serious infection requiring urgent treatment.
Dehydration from gastrointestinal side effects like vomiting or diarrhea may theoretically increase UTI susceptibility by concentrating urine. Maintaining adequate hydration is important, especially during dose escalation when gastrointestinal symptoms are most common.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.