LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Tirzepatide and chest pain is an important consideration for patients using this dual GIP/GLP-1 receptor agonist for type 2 diabetes or weight management. While chest pain is not a common side effect listed in FDA prescribing information, patients may experience chest discomfort through various mechanisms including gastrointestinal effects, reflux, or unrelated cardiac conditions. Understanding when chest symptoms warrant urgent evaluation is critical, as individuals with diabetes have elevated cardiovascular risk. This article examines the relationship between tirzepatide therapy and chest pain, helping patients and clinicians distinguish concerning symptoms from benign side effects.
Quick Answer: Chest pain is not a common side effect of tirzepatide, though patients may experience chest discomfort from gastrointestinal effects like reflux or nausea rather than direct cardiac effects.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus under the brand name Mounjaro and for chronic weight management as Zepbound. For weight management, Zepbound is indicated for adults with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² (overweight) with at least one weight-related comorbidity.
The mechanism of action involves simultaneous activation of both GIP and GLP-1 receptors, which are incretin hormones naturally produced in the gastrointestinal tract. By stimulating these receptors, tirzepatide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriately elevated glucagon secretion, and slows gastric emptying. These combined effects result in improved postprandial glucose control and reduced fasting glucose levels. Additionally, tirzepatide acts on central appetite regulation pathways, promoting satiety and reducing caloric intake, which contributes to its weight loss effects.
Tirzepatide is administered as a once-weekly subcutaneous injection, with dosing typically initiated at 2.5 mg (primarily for tolerability) and gradually titrated upward every 4 weeks based on glycemic response and tolerability. The maximum approved dose is 15 mg weekly for diabetes management. Clinical trials have demonstrated A1C reductions of 1.8% to 2.4% in type 2 diabetes (SURPASS program). Weight loss effects vary by population, with approximately 5-11% in diabetes trials and 15-21% in obesity trials (SURMOUNT program) at the highest doses. The medication's half-life of approximately five days allows for weekly administration.
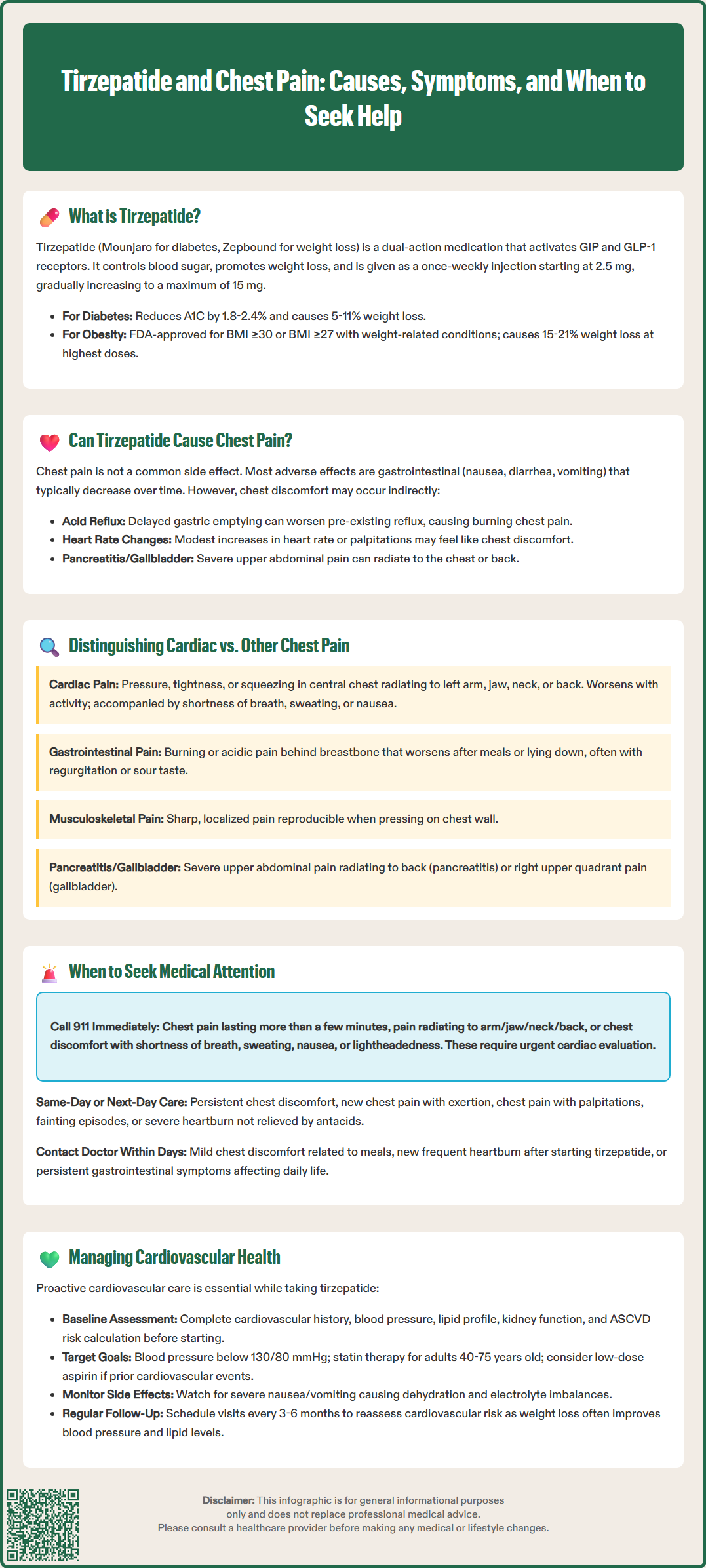
Chest pain is not listed as a common adverse effect in the FDA-approved prescribing information for tirzepatide. The most frequently reported adverse effects in clinical trials were gastrointestinal in nature, including nausea (12-22%), diarrhea (12-16%), vomiting (6-10%), and constipation (6-7%), with rates varying by dose. These symptoms typically occur during dose escalation and tend to diminish over time as tolerance develops.
However, chest discomfort can occasionally be reported by patients taking tirzepatide through several potential mechanisms. Severe nausea and vomiting may lead to esophageal irritation, gastroesophageal reflux, or musculoskeletal strain from retching—all of which can manifest as chest discomfort. The medication's effect on gastric emptying can exacerbate pre-existing gastroesophageal reflux disease (GERD), potentially causing retrosternal burning or pressure that mimics cardiac symptoms.
Tirzepatide can cause modest increases in heart rate and some patients may experience palpitations, which can be perceived as chest discomfort. Additionally, when used with insulin or sulfonylureas, hypoglycemia may occur, potentially causing adrenergic symptoms including palpitations or chest discomfort.
Importantly, tirzepatide carries warnings for pancreatitis and gallbladder disease, which can present with severe upper abdominal pain that may radiate to the chest or back. Patients with type 2 diabetes have an inherently elevated cardiovascular risk profile, independent of tirzepatide therapy. The SURPASS clinical trial program did not identify increased cardiovascular events with tirzepatide compared to placebo or active comparators, though dedicated cardiovascular outcome trials are still ongoing.
Differentiating between cardiac chest pain and other causes in patients taking tirzepatide requires careful clinical assessment. Cardiac chest pain typically presents as pressure, tightness, or squeezing in the central chest, often radiating to the left arm, jaw, neck, or back. It may be accompanied by dyspnea, diaphoresis, nausea, lightheadedness, or a sense of impending doom. Cardiac symptoms are frequently exertional, worsening with physical activity and improving with rest, though unstable angina or acute coronary syndrome can occur at rest.
Gastrointestinal chest discomfort associated with tirzepatide's side effects tends to present differently. Reflux-related chest pain is typically described as burning or acidic, located retrosternally, and often worsens after meals or when lying flat. It may be accompanied by regurgitation, dysphagia, or a sour taste. Esophageal spasm can cause severe chest pain that mimics cardiac ischemia but is usually associated with swallowing and may respond to antacids or smooth muscle relaxants.
Musculoskeletal pain is typically sharp, localized, and reproducible with chest wall palpation or movement. Pancreatitis presents with severe, persistent epigastric pain often radiating to the back, while gallbladder disease typically causes right upper quadrant pain that may radiate to the right shoulder or chest. Pulmonary conditions like pulmonary embolism may present with pleuritic chest pain worsened by breathing, often accompanied by dyspnea, tachypnea, or hemoptysis.
Clinical red flags that suggest cardiac origin include: sudden onset of severe symptoms, radiation to typical cardiac distribution areas, associated autonomic symptoms (sweating, pallor), exertional provocation, and risk factors such as prior cardiovascular disease, long-standing diabetes, hypertension, dyslipidemia, or family history of premature coronary disease. When uncertainty exists, cardiac evaluation should take precedence given the potentially life-threatening nature of acute coronary syndromes in this high-risk population.
Patients taking tirzepatide should be counseled to seek immediate emergency medical attention for any symptoms suggestive of acute cardiac events. Call 911 or proceed to the nearest emergency department immediately if experiencing: chest pain or pressure lasting more than a few minutes or that resolves and returns; pain radiating to the arm, jaw, neck, or back; chest discomfort accompanied by shortness of breath, sweating, nausea, or lightheadedness; or any sudden, severe chest pain that feels different from previous experiences. These symptoms require urgent evaluation with electrocardiography, cardiac biomarkers, and potential cardiac imaging to rule out myocardial infarction or unstable angina.
Seek same-day or next-day medical evaluation for: persistent or worsening chest discomfort that is not severe but concerning; new or changed patterns of chest pain with exertion; chest pain accompanied by palpitations or irregular heartbeat; persistent palpitations; syncope or near-syncope; or severe, persistent heartburn or reflux symptoms not responding to over-the-counter antacids. These situations warrant clinical assessment, though they may not require emergency services.
Contact your prescribing physician within a few days for: mild, intermittent chest discomfort clearly related to meals or reflux; new onset of frequent heartburn after starting tirzepatide; or persistent gastrointestinal symptoms affecting quality of life. Additionally, patients should report any concerning symptoms during routine follow-up appointments.
Patients should check their blood glucose during symptomatic episodes, especially if taking insulin or sulfonylureas alongside tirzepatide, as hypoglycemia can cause similar symptoms. While patients should generally not discontinue tirzepatide without medical guidance due to potential glycemic deterioration, they should immediately stop the medication and seek urgent medical care if they develop symptoms of pancreatitis (severe, persistent abdominal pain, sometimes radiating to the back) or serious allergic reactions.
Comprehensive cardiovascular risk management remains paramount for patients with type 2 diabetes receiving tirzepatide therapy, as diabetes increases cardiovascular risk. The American Diabetes Association (ADA) and American College of Cardiology (ACC) recommend a multifaceted approach that extends beyond glycemic control. Baseline cardiovascular assessment should include detailed history of prior cardiovascular events, current symptoms, blood pressure measurement, lipid profile, renal function assessment, and calculation of 10-year atherosclerotic cardiovascular disease (ASCVD) risk using validated tools such as the Pooled Cohort Equations.
Optimization of cardiovascular risk factors should occur concurrently with tirzepatide therapy. Blood pressure targets should be individualized, with a general goal of <130/80 mmHg for most patients with diabetes, though <140/90 mmHg may be appropriate for lower-risk individuals or when lower targets aren't feasible. Home blood pressure monitoring can help guide management. Statin therapy is recommended for most adults with diabetes aged 40-75 years, with at least moderate-intensity statins for most patients and high-intensity statins indicated for those with established ASCVD or multiple risk factors. Low-dose aspirin (typically 81 mg daily in the US) should be considered for secondary prevention in patients with prior cardiovascular events, while primary prevention use requires individualized assessment of bleeding risk versus benefit. Smoking cessation is imperative and should be actively supported.
Monitoring during tirzepatide therapy should include regular assessment of gastrointestinal tolerability, as severe nausea and vomiting can lead to dehydration and electrolyte disturbances that may indirectly affect cardiovascular stability. Patients should be educated about gradual dose titration to minimize gastrointestinal side effects. For those experiencing reflux symptoms, proton pump inhibitors or H2-receptor antagonists may be appropriate. Weight loss achieved with tirzepatide often improves cardiovascular risk markers, including blood pressure and lipid profiles, potentially allowing for medication adjustments. Regular follow-up every 3-6 months enables ongoing cardiovascular risk assessment, medication optimization, and prompt evaluation of any new symptoms.
Chest pain is not listed as a common adverse effect in tirzepatide's FDA prescribing information. When chest discomfort occurs, it is typically related to gastrointestinal side effects like reflux or nausea rather than direct cardiac effects of the medication.
Seek immediate emergency care for chest pain lasting more than a few minutes, pain radiating to the arm, jaw, neck, or back, or chest discomfort accompanied by shortness of breath, sweating, nausea, or lightheadedness. These symptoms require urgent cardiac evaluation.
Yes, tirzepatide's effects on gastric emptying can worsen gastroesophageal reflux disease, causing retrosternal burning or pressure. Severe nausea and vomiting may also lead to esophageal irritation or musculoskeletal strain that manifests as chest discomfort.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.