LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 injection pens are specialized medical devices that deliver glucagon-like peptide-1 receptor agonist medications through subcutaneous injection for managing type 2 diabetes and, in some cases, chronic weight management. These pre-filled pens offer a convenient alternative to traditional vial-and-syringe methods, featuring user-friendly designs with dose selectors and audible feedback mechanisms. FDA-approved GLP-1 medications work by mimicking a natural hormone that enhances insulin secretion, suppresses glucagon, and slows gastric emptying. Understanding how these injection pens function, their proper use, and their clinical benefits helps patients and healthcare providers make informed treatment decisions aligned with American Diabetes Association guidelines.
Quick Answer: GLP-1 injection pens are pre-filled devices that deliver glucagon-like peptide-1 receptor agonist medications subcutaneously to treat type 2 diabetes and certain weight management conditions.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
GLP-1 injection pens are pre-filled, disposable or reusable devices designed to deliver glucagon-like peptide-1 (GLP-1) receptor agonist medications subcutaneously. These medications are FDA-approved primarily for the treatment of type 2 diabetes mellitus, with some formulations also approved for chronic weight management in adults with obesity or overweight with at least one weight-related comorbidity.
GLP-1 is an incretin hormone naturally produced in the intestinal L-cells in response to food intake. GLP-1 receptor agonists mimic this endogenous hormone by binding to GLP-1 receptors on pancreatic beta cells, thereby enhancing glucose-dependent insulin secretion. This mechanism reduces the risk of hypoglycemia compared to insulin or sulfonylureas, as insulin release occurs only when blood glucose levels are elevated.
Beyond glycemic control, GLP-1 receptor agonists exert several additional effects that contribute to their therapeutic profile. They suppress glucagon secretion from pancreatic alpha cells, slow gastric emptying to reduce postprandial glucose excursions, and promote satiety through central nervous system pathways. These combined actions result in improved glycemic control, weight reduction, and potential cardiovascular benefits, though specific cardiovascular indications vary by agent according to FDA labeling.
The injection pen delivery system may improve adherence compared to traditional vial-and-syringe methods. Most pens feature dose selectors, hidden needles, and audible or tactile feedback to confirm dose delivery, making them accessible for patients with varying levels of dexterity or visual impairment. The subcutaneous route of administration allows for self-injection, typically in the abdomen, thigh, or upper arm.
Several GLP-1 receptor agonist formulations are available in the US market, each with distinct pharmacokinetic profiles and dosing schedules. Short-acting agents include exenatide immediate-release (Byetta) and lixisenatide (Adlyxin), though availability may be limited. These formulations primarily target postprandial glucose control due to their shorter half-lives.
Long-acting GLP-1 receptor agonists have gained prominence due to their convenient dosing schedules and comprehensive glycemic effects. These include:
Dulaglutide (Trulicity): Once-weekly injection with a single-dose pen featuring an automatic injection mechanism
Semaglutide (Ozempic): Once-weekly administration with dose escalation from 0.25 mg to maintenance doses of 0.5 mg, 1 mg, or 2 mg
Exenatide extended-release (Bydureon BCise): Once-weekly microsphere suspension requiring resuspension before injection
Liraglutide (Victoza): Once-daily injection available in a multi-dose pen
For weight management, semaglutide 2.4 mg (Wegovy) and liraglutide 3.0 mg (Saxenda) are specifically FDA-approved. Additionally, tirzepatide (Mounjaro, Zepbound) represents a dual GIP/GLP-1 receptor agonist—not a GLP-1 receptor agonist—available for both diabetes management and weight loss, depending on the brand and indication.
Fixed-ratio combination products containing both insulin and a GLP-1 receptor agonist are also available, including insulin glargine/lixisenatide (Soliqua) and insulin degludec/liraglutide (Xultophy).
Pen designs vary considerably across products. Some feature pre-attached needles with automatic injection mechanisms, while others require manual needle attachment and depression of an injection button. The American Diabetes Association (ADA) Standards of Care emphasize individualized selection based on patient preference, dosing frequency tolerance, insurance coverage, and clinical goals. Healthcare providers should consider renal function, gastrointestinal tolerability, and cardiovascular risk profile when selecting the most appropriate agent.
Patients should check current availability with their healthcare provider and pharmacy, as supply constraints may affect access to certain products.
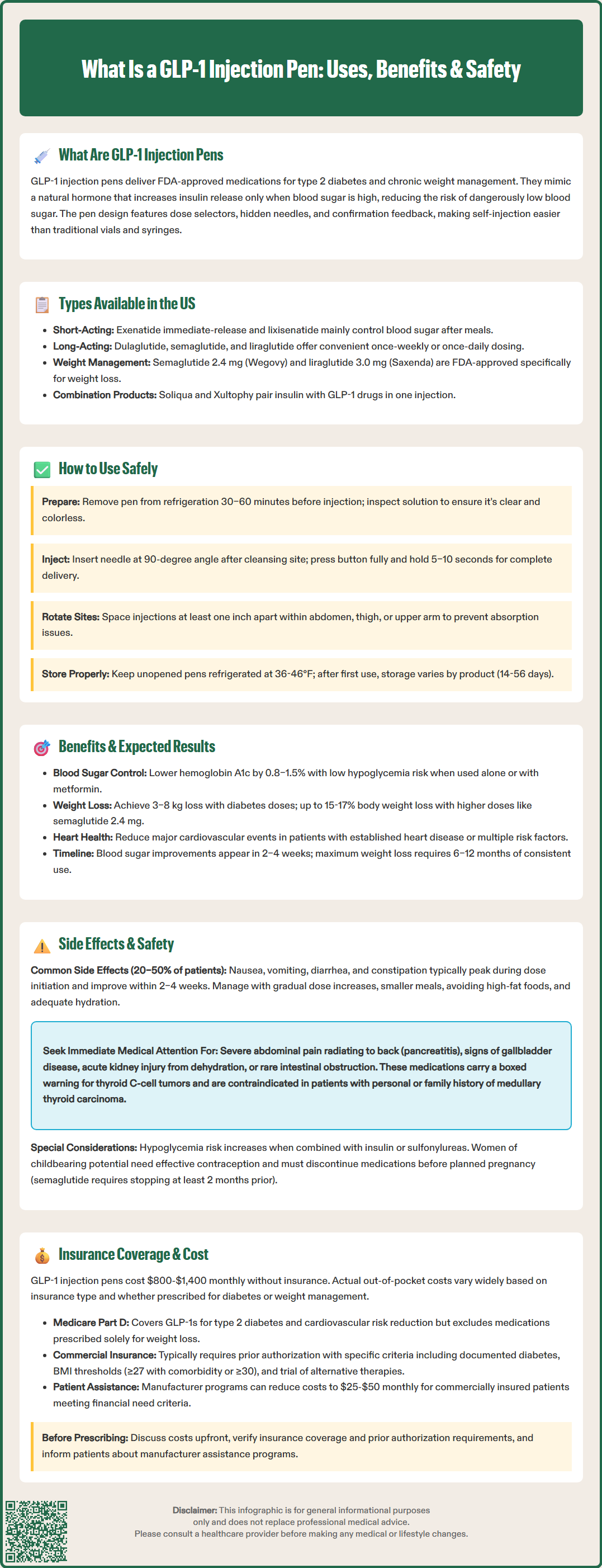
Proper injection technique is essential to ensure therapeutic efficacy and minimize adverse effects. Before initial use, patients should receive comprehensive training from a healthcare provider or diabetes educator, including hands-on demonstration with a training pen when available.
Pre-injection preparation involves several critical steps. Remove the pen from refrigerated storage 30–60 minutes before injection to allow it to reach room temperature, which reduces injection site discomfort. Never freeze these medications. Inspect the medication visually; most GLP-1 solutions should be clear and colorless (exenatide extended-release is an exception, appearing as a white suspension). Do not use if the solution appears discolored, cloudy (when it should be clear), or contains particulate matter. Wash hands thoroughly with soap and water.
Injection technique follows these general steps, though specific instructions vary by product:
For pens requiring needle attachment: Attach a new pen needle securely, removing both outer and inner needle caps
For pens requiring priming: Perform an airshot (flow check) as directed in the product instructions to ensure proper pen function
Select the prescribed dose using the dose selector (if applicable)
Choose an injection site in the abdomen (at least 2 inches from the navel), front of thigh, or upper arm
Cleanse the site with an alcohol swab and allow to air dry
Pinch the skin gently and insert the needle at a 90-degree angle
Depress the injection button fully and hold for the time specified in your product's instructions (typically 5–10 seconds) to ensure complete dose delivery
Remove the needle, dispose of it immediately in an FDA-cleared sharps container, and do not recap
Rotation of injection sites is important to prevent lipohypertrophy, which can impair medication absorption. Maintain a rotation pattern within the same anatomical region, spacing injections at least one inch apart from previous sites. Patients should never share pens or needles, even among family members, due to infection risk.
If a dose is missed, follow the specific instructions for your medication. For example, semaglutide (Ozempic) can be administered up to 5 days after the missed dose, while dulaglutide (Trulicity) allows up to 3 days. Always consult your product's Instructions for Use or your healthcare provider for specific guidance.
Storage requirements vary by product. Unopened pens generally require refrigeration (36-46°F/2-8°C). After first use, some pens can be stored at room temperature for specific periods (typically 14-56 days depending on the product), while others must return to refrigeration. Never use medication beyond its expiration date.
Only use FDA-approved GLP-1 medications obtained from licensed pharmacies. The FDA has issued warnings about compounded or counterfeit products that may cause serious harm.
GLP-1 receptor agonists demonstrate robust efficacy across multiple clinical endpoints. In pivotal clinical trials, these agents typically reduce hemoglobin A1c by 0.8–1.5% from baseline, with greater reductions observed at higher doses and in patients with higher baseline A1c values. The glucose-dependent mechanism of action results in a low intrinsic risk of hypoglycemia when used as monotherapy or with metformin, though risk increases when combined with insulin or sulfonylureas.
Weight loss represents a significant benefit, distinguishing GLP-1 receptor agonists from many other glucose-lowering medications. Patients typically experience 3–8 kg (6.6–17.6 lbs) weight reduction over 6–12 months with diabetes-indicated doses. Higher-dose formulations approved for weight management produce more substantial losses: semaglutide 2.4 mg (Wegovy) typically achieves 15-17% of baseline body weight loss, while liraglutide 3.0 mg (Saxenda) averages 5-7%. This effect results from delayed gastric emptying, enhanced satiety, and reduced caloric intake rather than increased energy expenditure.
Cardiovascular outcomes trials have demonstrated additional benefits beyond glycemic control. Liraglutide (LEADER trial), semaglutide (SUSTAIN-6), and dulaglutide (REWIND trial) have shown significant reductions in major adverse cardiovascular events (MACE) in patients with established cardiovascular disease or multiple cardiovascular risk factors. In 2024, semaglutide 2.4 mg (Wegovy) received FDA approval for reducing cardiovascular risk in adults with established cardiovascular disease and either obesity or overweight with at least one weight-related comorbidity, based on the SELECT trial. The FDA labels for these specific agents include cardiovascular risk reduction indications, making them preferred agents in patients with type 2 diabetes and atherosclerotic cardiovascular disease, as recommended by ADA/American College of Cardiology consensus guidelines.
Patients should understand that results develop gradually. Glycemic improvements typically manifest within 2–4 weeks, while maximum weight loss effects may require 6–12 months of consistent therapy. The ADA emphasizes realistic goal-setting and the importance of combining pharmacotherapy with lifestyle modifications, including medical nutrition therapy and increased physical activity, to optimize outcomes.
Gastrointestinal adverse effects represent the most common tolerability concerns with GLP-1 receptor agonists, occurring in 20–50% of patients. Nausea is typically most pronounced during dose initiation and escalation, generally improving over 2–4 weeks as physiologic adaptation occurs. Vomiting, diarrhea, constipation, and abdominal discomfort are also frequently reported. These effects result from delayed gastric emptying and are usually mild to moderate in severity.
To minimize gastrointestinal symptoms, clinicians should implement gradual dose titration protocols as specified in FDA labeling. Patients should be advised to eat smaller, more frequent meals, avoid high-fat foods, and stay well-hydrated. If nausea persists beyond 4–6 weeks or significantly impairs quality of life, dose reduction or alternative therapy should be considered.
Serious adverse effects require clinical vigilance:
Pancreatitis: Patients should be counseled to seek immediate medical attention for severe, persistent abdominal pain radiating to the back, with or without vomiting. While observational data have not definitively established causality, GLP-1 receptor agonists should be discontinued if pancreatitis is suspected and not restarted if confirmed
Gallbladder disease: Rapid weight loss increases cholelithiasis risk; patients with symptoms of cholecystitis or choledocholithiasis require appropriate evaluation
Acute kidney injury: Reported primarily in association with severe gastrointestinal adverse effects leading to dehydration; monitoring renal function is advisable in at-risk patients. Exenatide is not recommended in severe renal impairment (eGFR <30 mL/min/1.73m²)
Hypoglycemia: Risk increases when combined with insulin or sulfonylureas; dose reduction of these concomitant agents is often necessary
Thyroid C-cell tumors: Based on rodent studies, GLP-1 receptor agonists carry a boxed warning regarding medullary thyroid carcinoma risk and are contraindicated in patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2
Intestinal obstruction/ileus: Rare cases have been reported with some agents; patients with severe gastrointestinal disease or gastroparesis may not be suitable candidates
Hypersensitivity reactions: Including anaphylaxis, have been reported rarely
Injection site reactions, including erythema, pruritus, or induration, occur in approximately 2–5% of patients and are generally self-limited. Diabetic retinopathy complications have been observed with rapid glycemic improvement, particularly with semaglutide; patients with pre-existing retinopathy should undergo ophthalmologic monitoring.
Pregnancy considerations: Women of childbearing potential should use effective contraception while on these medications. Discontinuation timing before planned pregnancy varies by product: semaglutide should be stopped at least 2 months before, while other agents have different recommendations. These medications should be discontinued immediately if pregnancy occurs.
Perioperative management: According to 2024 multi-society guidance, most patients can continue GLP-1 receptor agonists perioperatively, though individualized risk assessment is recommended, particularly for major gastrointestinal surgery or procedures with high aspiration risk.
Drug interactions: Tirzepatide and some short-acting GLP-1 receptor agonists may delay absorption of oral medications due to gastric emptying effects. Oral contraceptives should be taken at least 1 hour before these medications or 4 hours after.
GLP-1 injection pens represent a significant financial consideration, with estimated list prices typically ranging from $800 to $1,400 per month without insurance coverage. Actual out-of-pocket costs vary substantially based on insurance type, formulary tier placement, and whether the medication is prescribed for FDA-approved diabetes or weight management indications.
Medicare Part D coverage for GLP-1 receptor agonists varies by plan. Medications prescribed for type 2 diabetes are generally covered, though tier placement (typically Tier 3 or 4) affects copayment amounts. As of 2024, Medicare Part D plans may cover semaglutide 2.4 mg (Wegovy) when prescribed for its cardiovascular risk reduction indication in eligible patients. However, Medicare Part D still does not cover medications prescribed solely for weight loss, even for FDA-approved weight management agents, due to statutory exclusions under the Medicare Prescription Drug, Improvement, and Modernization Act of 2003.
Medicaid coverage varies significantly by state, with some states providing access to these medications with prior authorization and others imposing more restrictive criteria or excluding coverage for weight management.
Commercial insurance coverage is more variable. Most plans include at least one GLP-1 receptor agonist on formulary, but prior authorization requirements are nearly universal. Typical criteria include:
Documented diagnosis of type 2 diabetes with inadequate glycemic control on metformin or other first-line agents
BMI ≥27 kg/m² with weight-related comorbidity or BMI ≥30 kg/m² (for weight management indications)
Trial and failure of alternative therapies
Absence of contraindications
Coverage for weight management indications under commercial plans has expanded but remains inconsistent, with many employers specifically excluding obesity medications from pharmacy benefits.
Patient assistance programs offered by manufacturers can significantly reduce costs for eligible patients. These programs typically require documentation of financial need and lack of adequate insurance coverage. Copay assistance cards may reduce out-of-pocket costs to $25–$50 per month for commercially insured patients, though restrictions apply for government insurance beneficiaries due to federal anti-kickback statutes.
Clinicians should engage patients in transparent cost discussions before prescribing, verify insurance coverage and prior authorization requirements, and provide information about manufacturer assistance programs. Pharmacy benefit managers increasingly employ step therapy protocols, requiring trial of less expensive agents before approving GLP-1 receptor agonists. The American Association of Clinical Endocrinology advocates for improved access to these evidence-based therapies, particularly for patients with cardiovascular disease or obesity-related complications where clinical benefits are well-established.
Injection frequency depends on the specific medication: long-acting agents like semaglutide (Ozempic) and dulaglutide (Trulicity) require once-weekly administration, while liraglutide (Victoza) is injected once daily. Your healthcare provider will determine the appropriate dosing schedule based on your treatment goals and the specific FDA-approved product prescribed.
GLP-1 receptor agonists have a low intrinsic risk of hypoglycemia when used alone or with metformin because they enhance insulin secretion only when blood glucose is elevated. However, hypoglycemia risk increases significantly when combined with insulin or sulfonylureas, often requiring dose adjustments of these concomitant medications.
Medicare Part D generally covers GLP-1 medications prescribed for type 2 diabetes, though tier placement affects copayment amounts. As of 2024, some plans may cover semaglutide 2.4 mg (Wegovy) for cardiovascular risk reduction in eligible patients, but Medicare does not cover medications prescribed solely for weight loss due to statutory exclusions.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.