LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Choosing the right breakfast while taking semaglutide can significantly impact your treatment experience and nutritional health. Semaglutide, a GLP-1 receptor agonist approved for type 2 diabetes and weight management, alters appetite and digestion in ways that make traditional breakfast choices challenging. Many patients experience reduced hunger, early fullness, and gastrointestinal side effects that require thoughtful meal planning. Understanding what to eat for breakfast on semaglutide helps maximize nutrition, minimize discomfort, and support your therapeutic goals. This guide provides evidence-based recommendations for breakfast foods that work with your medication, not against it, while addressing common side effects and offering practical meal ideas.
Quick Answer: Optimal breakfast choices on semaglutide should prioritize lean proteins, complex carbohydrates, and easily digestible foods in smaller portions while avoiding high-fat, greasy, and heavily processed items that can worsen gastrointestinal side effects.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). Its mechanism of action directly influences appetite regulation and gastrointestinal function, which has significant implications for breakfast choices and meal planning.
Gastrointestinal effects are among the most common adverse reactions to semaglutide. The medication slows gastric emptying—the rate at which food leaves the stomach and enters the small intestine. This delayed emptying contributes to prolonged feelings of fullness but can also cause nausea, bloating, and early satiety, particularly during the first few weeks of treatment or after dose escalation. According to FDA prescribing information, nausea rates vary by indication and dosage—approximately 15-20% of patients taking semaglutide for diabetes management experience nausea, while rates increase to up to 44% for those on higher doses for weight management.
These physiological changes mean that breakfast requires thoughtful planning. Patients may find that their usual morning meal feels too heavy or triggers discomfort. Understanding how semaglutide alters normal digestive processes helps inform better food choices that work with, rather than against, the medication's effects.
Optimal breakfast choices while taking semaglutide should prioritize nutrient density, adequate protein, and foods that are gentle on the digestive system. Given the medication's appetite-suppressing effects, maximizing nutritional value in smaller portions becomes essential to prevent deficiencies while supporting metabolic health.
Lean protein sources should form the foundation of a semaglutide-friendly breakfast. Protein helps maintain muscle mass during weight loss, promotes satiety, and stabilizes blood glucose levels. Excellent options include eggs (prepared with minimal fat), Greek yogurt, cottage cheese, turkey or chicken breast, and plant-based alternatives like tofu scrambles. Including adequate protein at breakfast (typically 15-30 grams, individualized based on your needs) supports metabolic health. Those with kidney disease should consult their healthcare provider about appropriate protein intake. Protein also tends to be well-tolerated even when appetite is suppressed.
Complex carbohydrates provide sustained energy without causing rapid blood sugar spikes. Steel-cut or rolled oats, quinoa, whole grain toast, and sweet potatoes offer fiber, B vitamins, and minerals. These foods digest more slowly than refined carbohydrates, which helps maintain stable blood glucose levels. Portion sizes may need adjustment based on individual tolerance—a half-cup of cooked oatmeal may suffice where a full cup was previously consumed.
Healthy fats in moderation support nutrient absorption and provide essential fatty acids. Small amounts of avocado, nuts, seeds, or nut butters can enhance breakfast satisfaction. However, because fats slow digestion further and are calorie-dense, portions should be carefully controlled based on individual tolerance—typically one to two tablespoons of nut butter or a quarter of an avocado.
Fruits and vegetables add vitamins, minerals, antioxidants, and fiber. Berries, bananas, apples, spinach, tomatoes, and bell peppers work well in breakfast preparations. These foods are generally well-tolerated and help ensure adequate micronutrient intake when overall food volume decreases. Aim for at least one serving of produce at breakfast to support digestive health and provide natural fiber that aids regular bowel movements—important since constipation can be a side effect of semaglutide therapy.
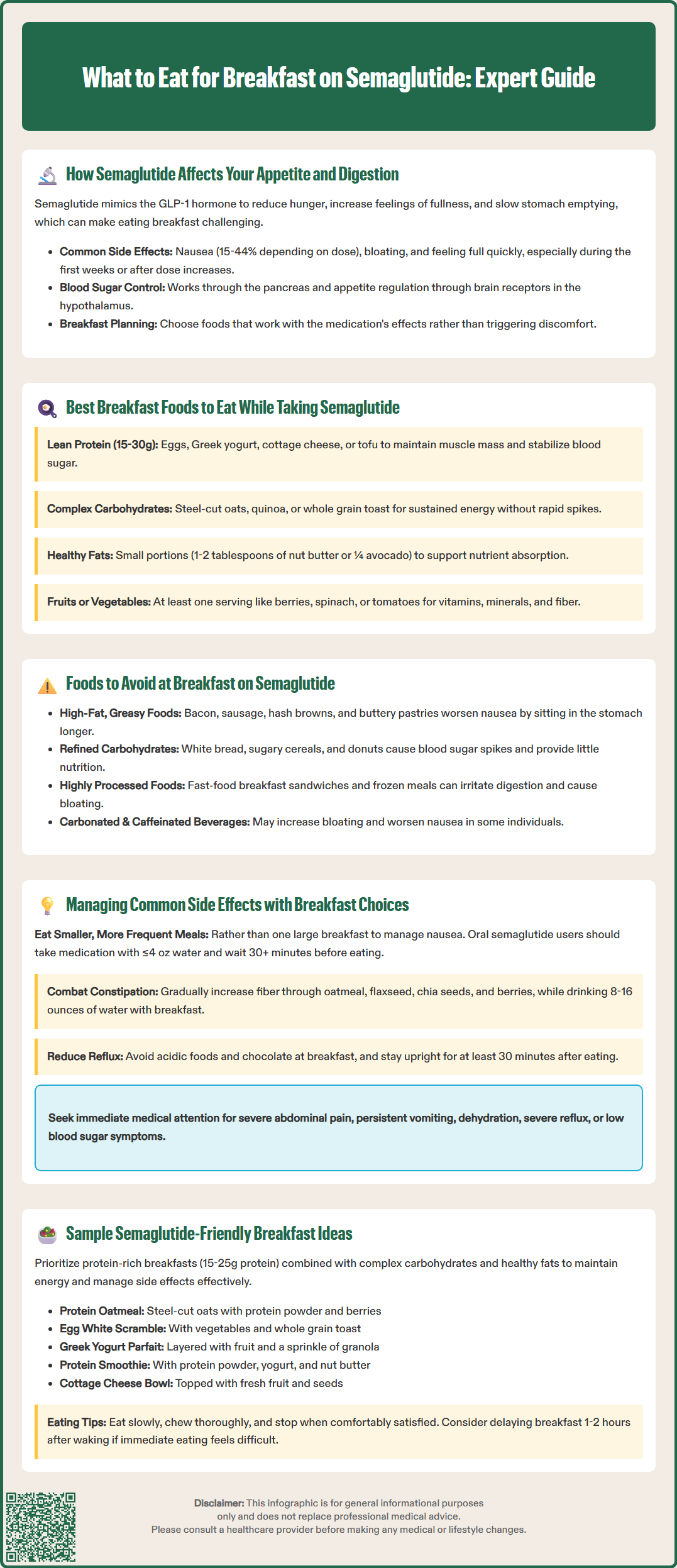
Certain breakfast foods can exacerbate semaglutide's gastrointestinal side effects or work against the medication's therapeutic goals. Identifying and limiting these items can significantly improve treatment tolerance and outcomes.
High-fat, greasy foods are particularly problematic. Bacon, sausage, hash browns fried in oil, buttery pastries, and cream-based dishes can trigger or worsen nausea due to delayed gastric emptying. Fatty foods require more time and digestive effort to process, and when combined with semaglutide's gastric-slowing effects, they may sit uncomfortably in the stomach for extended periods. Many patients report that foods they previously enjoyed—such as eggs benedict or breakfast burritos with cheese and sour cream—now cause significant discomfort.
Refined carbohydrates and added sugars should be minimized. White bread, sugary cereals, pastries, donuts, and sweetened beverages can cause rapid blood glucose fluctuations, which is counterproductive for patients using semaglutide for diabetes management. These foods also provide minimal nutritional value relative to their calorie content, making them poor choices when appetite is reduced and every bite should contribute to nutritional needs.
Highly processed foods often contain additives, excessive sodium, and artificial ingredients that may irritate the digestive system. Breakfast sandwiches from fast-food restaurants, frozen breakfast meals, and packaged pastries typically combine multiple problematic elements: high fat, refined carbohydrates, and sodium levels that can contribute to bloating and discomfort.
Carbonated and caffeinated beverages may need to be limited based on individual tolerance. While there is no official contraindication between semaglutide and caffeine, some people find that carbonated drinks increase bloating and gastric discomfort, particularly when gastric emptying is already delayed. Similarly, caffeine may worsen nausea in sensitive individuals. If you enjoy coffee or tea, consider starting with small amounts and monitoring how your body responds.
Large portion sizes of any food should be avoided. Even nutritious foods can cause discomfort when consumed in quantities that exceed the stomach's capacity. Patients often need to relearn appropriate portion sizes, typically reducing breakfast volume based on comfort and satiety signals rather than eating out of habit.
Strategic breakfast planning can help mitigate the most common adverse effects associated with semaglutide therapy, improving medication adherence and quality of life during treatment.
For nausea management, the timing and composition of breakfast are critical. Eating smaller, more frequent meals rather than one large breakfast often helps. For injectable semaglutide (Ozempic, Wegovy), some patients find that adjusting meal timing based on their injection schedule improves tolerance. For oral semaglutide (Rybelsus), it's essential to follow FDA-approved administration instructions: take upon waking with no more than 4 ounces of plain water, then wait at least 30 minutes before consuming any food, beverages, or other oral medications. Some patients report that ginger tea or peppermint tea may provide comfort, though evidence for their anti-nausea effects is limited. Cold or room-temperature foods are sometimes better tolerated than hot meals when nausea is present. Avoiding strong food odors during preparation can also help, as heightened sensitivity to smells is common.
Constipation can occur with semaglutide use, with rates varying by product and dosage according to FDA prescribing information. This can be addressed through fiber-rich breakfast choices. Incorporating oatmeal with ground flaxseed, chia seeds, berries, and adequate fluid intake supports regular bowel movements. However, fiber should be increased gradually to avoid gas and bloating. Prunes or prune juice at breakfast can provide gentle natural laxative effects. Adequate hydration throughout the morning—aiming for at least 8-16 ounces of water with breakfast—is essential, as dehydration can worsen constipation.
Early satiety and reduced appetite require a focus on nutrient-dense foods. When patients can only consume small amounts, every bite should contribute meaningful nutrition. Protein smoothies or shakes can be particularly useful, allowing patients to consume adequate protein, vitamins, and minerals in a more easily tolerated liquid form. Adding protein powder, yogurt, nut butter, and fruits to smoothies creates a nutritionally balanced breakfast that doesn't require chewing or dealing with solid food textures that may feel unappealing.
Gastroesophageal reflux may occur or worsen in some patients. Avoiding acidic foods (citrus fruits, tomatoes) and chocolate at breakfast can help. Eating in an upright position and remaining upright for at least 30 minutes after breakfast reduces reflux risk.
Important safety note: Contact your healthcare provider immediately if you experience severe or persistent abdominal pain (with or without vomiting), signs of pancreatitis or gallbladder disease, persistent vomiting leading to dehydration, severe reflux symptoms, or hypoglycemia (especially if you also take insulin or sulfonylureas). These may require medical attention or medication adjustments.
Practical, balanced breakfast options can help patients maintain adequate nutrition while managing semaglutide's effects. These examples emphasize protein, incorporate complex carbohydrates and healthy fats in appropriate portions, and are generally well-tolerated.
Option 1: Protein-Packed Oatmeal Prepare one-half cup of steel-cut oats with water or unsweetened almond milk. Stir in one scoop of unflavored or vanilla protein powder (adding 15-25g protein), top with a quarter-cup of fresh berries, one tablespoon of ground flaxseed, and a sprinkle of cinnamon. This combination provides sustained energy, fiber for digestive health, and adequate protein in a gentle, easily digestible format.
Option 2: Vegetable Egg White Scramble Scramble three egg whites (or one whole egg plus two whites) with sautéed spinach, tomatoes, and mushrooms cooked in a small amount of olive oil spray. Serve with one slice of whole grain toast and a quarter of an avocado. This breakfast delivers protein, healthy fats, and multiple servings of vegetables while remaining relatively light and unlikely to trigger nausea.
Option 3: Greek Yogurt Parfait Layer three-quarters cup of plain Greek yogurt (regular or low-fat based on preference) with one-quarter cup of low-sugar granola, mixed berries, and one tablespoon of sliced almonds. Add a drizzle of honey if desired (one teaspoon maximum). This option provides probiotics that may support digestive health, protein, and antioxidants from berries. Lactose-free or plant-based yogurt alternatives work well for those with dairy sensitivities.
Option 4: Protein Smoothie Blend one scoop of protein powder, one-half cup of frozen berries, one-half banana, one cup of unsweetened almond milk, one tablespoon of natural peanut butter, and a handful of spinach. This liquid breakfast is often well-tolerated even when solid foods feel unappealing and provides balanced nutrition in an easily consumed format.
Option 5: Cottage Cheese Bowl Combine three-quarters cup of cottage cheese with diced peaches or pineapple, one tablespoon of chia seeds, and a sprinkle of cinnamon. This high-protein, low-preparation option works well for patients with limited morning appetite or time.
Important considerations: Patients should eat slowly, chewing thoroughly, and stop eating when feeling comfortably satisfied rather than full. Meal timing may require adjustment—some patients tolerate breakfast better 1-2 hours after waking rather than immediately. If taking Rybelsus, remember to wait at least 30 minutes after taking the medication before eating breakfast. Keeping a food diary to track which breakfast options are best tolerated can help identify personal patterns and preferences. Any persistent difficulty eating, unintended rapid weight loss, or severe gastrointestinal symptoms should prompt consultation with a healthcare provider, as dose adjustment or additional interventions may be necessary.
Yes, eggs are an excellent breakfast choice on semaglutide when prepared with minimal fat. They provide high-quality protein that helps maintain muscle mass and promotes satiety without typically triggering nausea or discomfort.
Semaglutide slows gastric emptying and acts on brain appetite centers, which can cause nausea, especially with high-fat or large-portion breakfasts. Eating smaller amounts of easily digestible foods and avoiding greasy items typically reduces this side effect.
According to FDA prescribing information, you must wait at least 30 minutes after taking Rybelsus before consuming any food, beverages (other than plain water), or other oral medications to ensure proper absorption of the medication.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.