LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
What to expect after first semaglutide injection is a common concern for patients beginning this GLP-1 medication for type 2 diabetes or weight management. After your initial subcutaneous injection, semaglutide begins binding to receptors throughout your body, triggering changes in appetite, digestion, and metabolism. Most patients experience mild, manageable effects in the first 24-48 hours, including reduced hunger and possible gastrointestinal symptoms like nausea. Understanding the typical timeline and side effects helps you prepare for this adjustment period and recognize when medical attention may be needed. This guide provides evidence-based information on what happens after your first dose.
Quick Answer: After your first semaglutide injection, you can expect reduced appetite and possible mild nausea within 24-48 hours, though significant weight loss and full therapeutic effects develop gradually over 4-5 weeks as the medication reaches steady-state levels.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist that begins working shortly after subcutaneous injection, though its full effects develop gradually over several weeks. After your first injection, the medication enters your bloodstream and starts binding to GLP-1 receptors in multiple tissues, including the pancreas, gastrointestinal tract, and brain.
In the first 24 to 48 hours, many patients notice subtle changes in appetite and satiety. Semaglutide slows gastric emptying—the rate at which food leaves your stomach—which can create a feeling of fullness that persists longer than usual after meals. This effect on gastric emptying is typically strongest initially and tends to diminish with continued use. Some individuals report feeling less interested in food or experiencing earlier satiety when eating. These effects are typically mild initially, as starting doses (0.25 mg weekly for both Ozempic and Wegovy) are intentionally low to allow your body to adjust.
It is important to understand that semaglutide has a long half-life of approximately one week, meaning it takes four to five weeks to reach steady-state concentrations in your body. Consequently, the effects you experience after the first injection represent only the beginning of the medication's action. Most patients do not see significant weight loss or substantial glucose control improvements in the first 48 hours.
During this initial period, monitor how you feel and maintain adequate hydration. Some patients experience mild nausea or gastrointestinal discomfort as their body adapts to the medication's effects on the digestive system. These early responses are generally transient and tend to improve as treatment continues.
Gastrointestinal side effects are the most frequently reported adverse reactions following the first semaglutide injection. According to FDA prescribing information, the frequency of side effects varies between Ozempic (for type 2 diabetes) and Wegovy (for weight management), with higher rates typically seen with Wegovy as it is titrated to higher doses.
Nausea is the most prevalent side effect, affecting approximately 16-20% of Ozempic patients and up to 44% of Wegovy patients in clinical trials. This typically manifests as mild to moderate queasiness that may be more noticeable after eating. The nausea is generally most pronounced during the first few days after injection and often diminishes with subsequent doses.
Gastrointestinal symptoms beyond nausea are also common and may include:
Decreased appetite or early satiety
Mild abdominal discomfort or bloating
Diarrhea (reported in 8-9% of Ozempic patients; up to 30% with Wegovy)
Constipation (reported in 5-7% of Ozempic patients; up to 24% with Wegovy)
Occasional vomiting in more sensitive individuals
Fatigue and headache occur in some patients during the initial adjustment period, though these symptoms are typically mild and self-limiting. Some individuals report feeling slightly more tired than usual or experiencing mild headaches in the first few days.
Injection site reactions such as redness, itching, or mild discomfort at the injection site affect a small percentage of patients but are generally minor and resolve quickly.
It is worth noting that the starting dose of semaglutide (0.25 mg weekly) is specifically designed to minimize side effects while allowing your body to adapt to the medication. Most adverse effects are dose-dependent, meaning they tend to be less severe at lower doses. The majority of patients who experience side effects after their first injection find that these symptoms are mild, manageable, and improve significantly within the first week as physiological adaptation occurs.
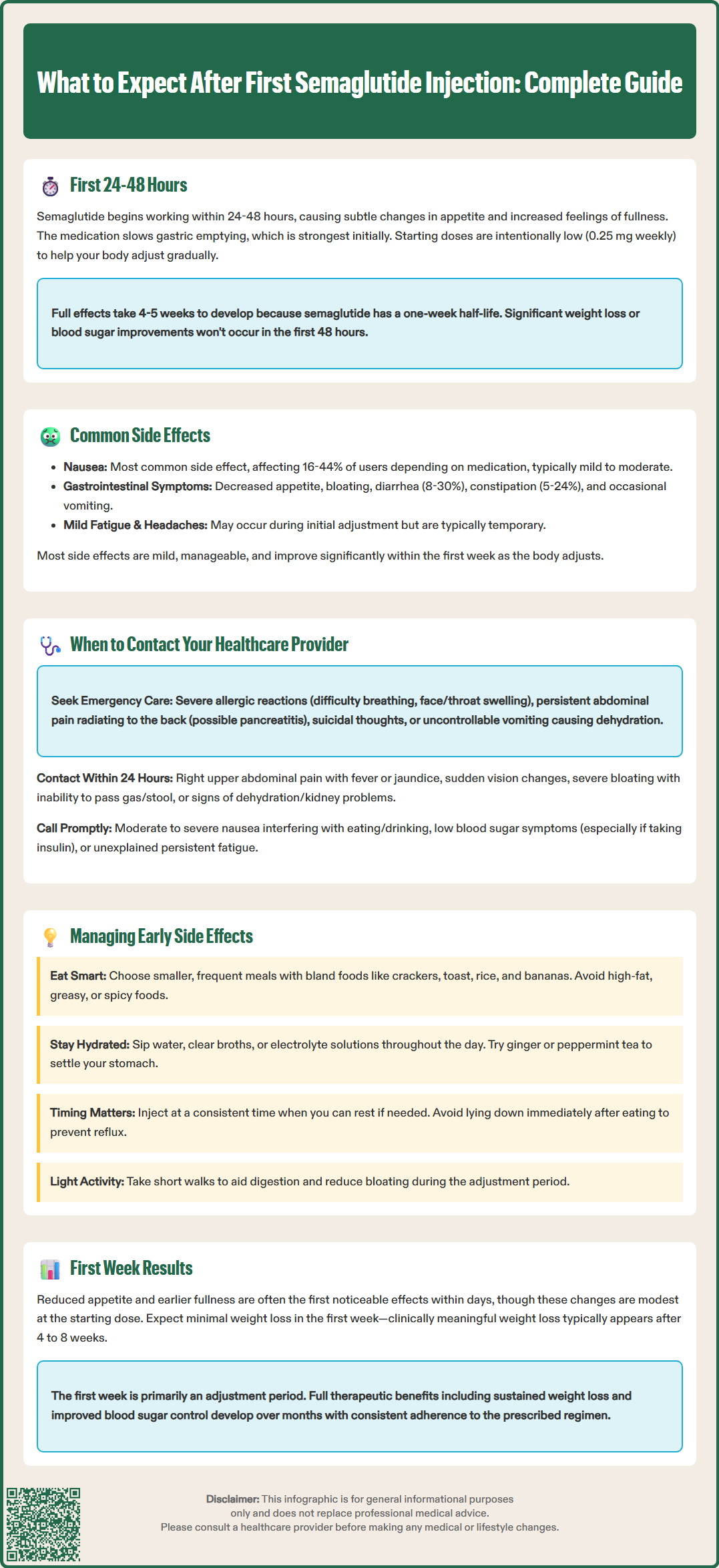
While most side effects after the first semaglutide injection are mild and expected, certain symptoms warrant prompt medical attention. Understanding when to seek help ensures your safety and allows for appropriate management of potentially serious complications.
Call 911 or seek emergency medical care immediately if you experience:
Signs of severe allergic reaction (anaphylaxis), including difficulty breathing, severe rash, swelling of the face or throat, or rapid heartbeat
Severe, persistent abdominal pain, particularly if radiating to the back, which may indicate pancreatitis (stop taking semaglutide)
Suicidal thoughts or behaviors (alternatively, call or text 988 Suicide & Crisis Lifeline)
Persistent vomiting that prevents you from keeping down fluids, risking dehydration
Contact your healthcare provider within 24 hours if you notice:
Right upper abdominal pain, fever, or yellowing of skin/eyes, which may indicate gallbladder disease
Sudden changes in vision, floaters, or vision loss, especially if you have diabetic retinopathy
Severe abdominal bloating, inability to pass gas or stool, which may suggest intestinal obstruction (ileus)
Signs of dehydration or possible kidney problems, including dark urine, dizziness, or decreased urination
Moderate to severe nausea that interferes with eating or drinking
Symptoms of hypoglycemia (particularly if taking insulin or sulfonylureas), such as shakiness, confusion, sweating, or rapid heartbeat
Unexplained persistent fatigue or weakness
Routine follow-up is appropriate for mild, tolerable side effects that do not interfere with daily activities. However, if you are uncertain about the severity of any symptom, err on the side of caution and contact your healthcare provider. Your medical team can assess whether symptoms are within the expected range or require intervention, such as dose adjustment, additional medications to manage side effects, or discontinuation of semaglutide if necessary.
Important: Semaglutide is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2), and is not recommended during pregnancy, especially when used for weight management.
Implementing practical strategies can significantly reduce the impact of side effects during your initial experience with semaglutide. These evidence-based approaches help your body adjust to the medication while maintaining adequate nutrition and hydration.
Dietary modifications are among the most effective interventions:
Eat smaller, more frequent meals rather than large portions, which can overwhelm your slowed digestive system
Choose bland, easily digestible foods during the first few days, such as crackers, toast, rice, bananas, and applesauce
Avoid high-fat, greasy, or spicy foods that may exacerbate nausea
Limit foods with strong odors if you are experiencing nausea
Eat slowly and chew thoroughly to aid digestion
Stop eating when you feel comfortably satisfied, as overeating can worsen gastrointestinal discomfort
Hydration strategies are critical, especially if experiencing nausea, vomiting, or diarrhea:
Sip water, clear broths, or electrolyte solutions throughout the day
Avoid large volumes of liquid at once, which can increase nausea
Consider ginger tea or peppermint tea, which may help settle the stomach
Limit caffeine and alcohol, as these can worsen dehydration and gastrointestinal symptoms
Timing and lifestyle adjustments can also help:
Administer your injection at a consistent time each week, preferably when you can rest if needed
Some patients anecdotally report that injecting in the evening may reduce daytime nausea, though this varies by individual
Avoid lying down immediately after eating, which can worsen reflux or nausea
Engage in light physical activity, such as short walks, which may help with digestion and reduce bloating
Pharmacological support may be appropriate in some cases. Discuss with your healthcare provider whether anti-nausea medications (such as ondansetron) or other supportive treatments might be beneficial if dietary and lifestyle modifications are insufficient. Never adjust your semaglutide dose without medical guidance.
Be aware that semaglutide's effect on slowing gastric emptying may potentially affect the absorption of some oral medications. If you take medications with a narrow therapeutic index, consult your healthcare provider about optimal timing of these medications.
Setting realistic expectations for your first week on semaglutide is essential for maintaining motivation and understanding the medication's timeline of action. While individual responses vary, certain patterns are commonly observed during the initial treatment period.
Appetite and eating behavior changes are often the first noticeable effects. Many patients report reduced hunger, earlier feelings of fullness during meals, and decreased food cravings within the first few days. These changes reflect semaglutide's action on appetite-regulating centers in the brain and its effect on gastric emptying. However, the magnitude of these effects is typically modest at the starting dose and becomes more pronounced as the dose is gradually increased over subsequent weeks.
Weight loss in the first week is generally minimal and should not be used as a primary indicator of treatment success. Most patients experience variable weight changes during the first week, which may reflect water weight or reduced food intake rather than significant fat loss. Clinically meaningful weight loss typically becomes apparent after 4 to 8 weeks of treatment, once therapeutic doses are reached and steady-state drug levels are achieved. In clinical trials, significant weight loss was observed over months, not days.
Blood glucose effects for patients with type 2 diabetes may begin to appear within the first week, though substantial improvements generally require several weeks. Semaglutide enhances glucose-dependent insulin secretion and suppresses inappropriate glucagon release, but these effects build gradually. Patients should continue monitoring blood glucose as directed and be aware of hypoglycemia risk if taking other glucose-lowering medications, particularly insulin or sulfonylureas.
Overall well-being varies considerably among individuals. Some patients feel energized and positive about starting treatment, while others experience mild fatigue or gastrointestinal discomfort that temporarily affects their quality of life. These initial experiences do not predict long-term outcomes. The first week is primarily an adjustment period, and the full therapeutic benefits of semaglutide—including sustained weight loss and improved glycemic control—develop over months, not days. Patience and consistent adherence to the prescribed regimen are key to achieving optimal results.
Semaglutide begins binding to receptors within hours of injection, with appetite reduction often noticeable within 24-48 hours. However, full therapeutic effects develop over 4-5 weeks as the medication reaches steady-state concentrations in your body.
Yes, nausea is the most common side effect, affecting 16-44% of patients depending on the formulation. It is typically mild at the starting dose and improves within the first week as your body adjusts to the medication.
Seek emergency care for severe abdominal pain, difficulty breathing, persistent vomiting, or suicidal thoughts. Contact your provider within 24 hours for vision changes, signs of gallbladder disease, severe nausea interfering with eating, or symptoms of hypoglycemia if taking other diabetes medications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.