LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

When to stop metformin before colonoscopy is a common question for patients with type 2 diabetes preparing for this screening procedure. Metformin, a first-line oral diabetes medication, may need temporary discontinuation due to dehydration risks during bowel preparation that could theoretically affect kidney function and drug clearance. The timing varies based on your kidney function, overall health, and specific institutional protocols. While practices differ across U.S. healthcare systems, most centers recommend holding metformin when bowel preparation begins—typically the day before your procedure. This article explains the medical rationale, timing considerations, and blood sugar management strategies during this brief medication interruption.
Quick Answer: Metformin is typically stopped when colonoscopy bowel preparation begins (usually the day before the procedure) and on the morning of colonoscopy, then restarted once normal eating and hydration resume.
Metformin is a first-line oral medication for type 2 diabetes that works primarily by reducing hepatic glucose production and improving insulin sensitivity in peripheral tissues. While generally well-tolerated, metformin carries a rare but serious risk of lactic acidosis, particularly when kidney function is compromised or during periods of physiological stress.
Colonoscopy preparation involves bowel cleansing with osmotic laxatives and dietary restrictions that can lead to dehydration and temporary alterations in kidney function. This dehydration risk is the primary concern prompting temporary metformin discontinuation. Standard colonoscopy does not use intravenous contrast agents; however, if separate imaging with iodinated contrast is planned alongside your colonoscopy, additional precautions apply per FDA labeling.
The decision to temporarily discontinue metformin before colonoscopy is not universally standardized and depends on individual patient factors. Institutional protocols vary widely in the United States. Risk stratification is based on baseline kidney function, hydration status, and the specific colonoscopy protocol being used. Patients with normal renal function undergoing routine screening colonoscopy may have different instructions than those with impaired kidney function.
Healthcare providers assess several factors when making this determination: baseline estimated glomerular filtration rate (eGFR), patient age, comorbid conditions affecting kidney function, and the type of bowel preparation prescribed. The FDA label for metformin recommends temporary discontinuation in situations where acute kidney injury is anticipated. This individualized approach balances diabetes management continuity with patient safety during the periprocedural period.
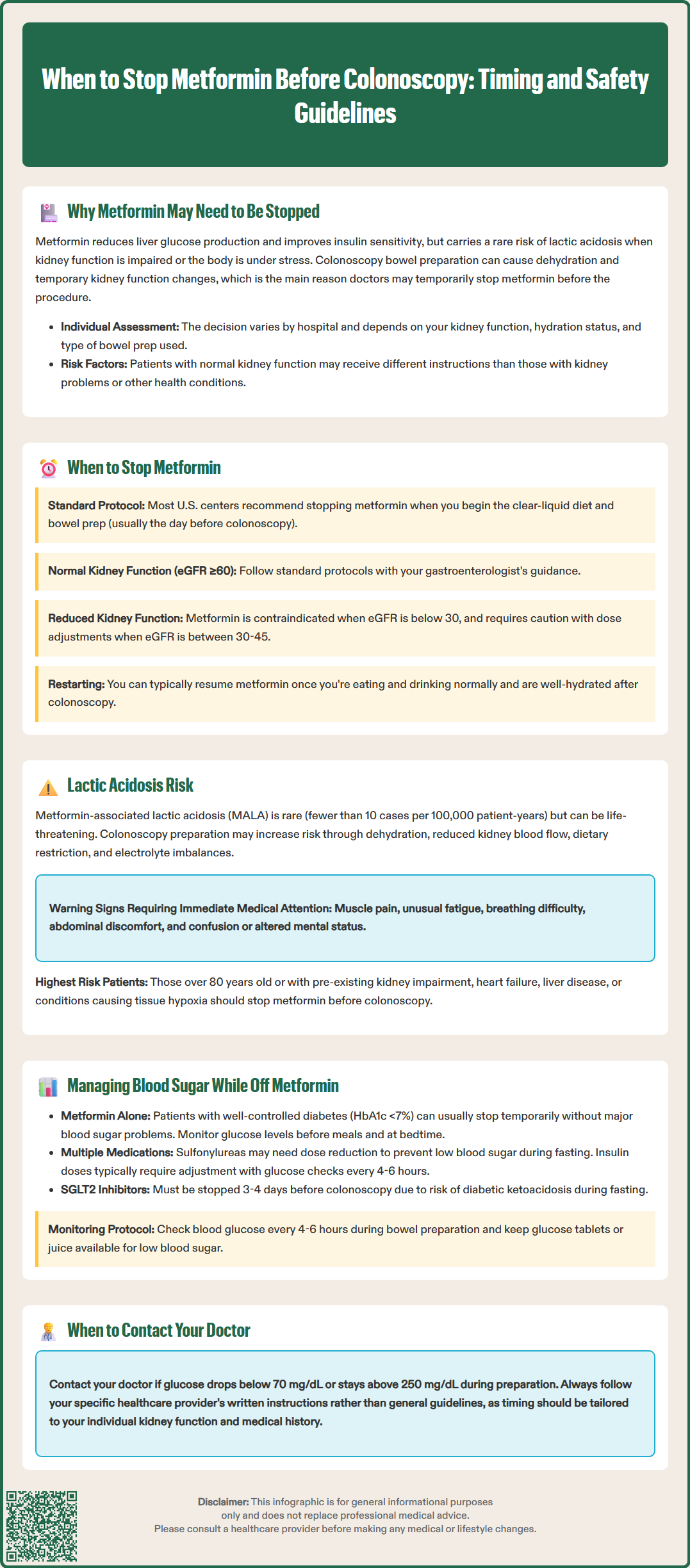
The timing of metformin discontinuation before colonoscopy varies based on institutional protocols and individual patient risk assessment. Practices differ across healthcare systems, and you should always follow the specific written instructions provided by your endoscopy center and healthcare provider.
For routine colonoscopy without contrast, many U.S. centers recommend holding metformin when the clear-liquid diet and bowel preparation begin (typically the day before the procedure) and on the morning of the procedure. This approach minimizes exposure during the period of greatest dehydration risk.
Patients with normal renal function (eGFR ≥60 mL/min/1.73 m²) generally follow standard institutional protocols. Those with reduced kidney function require more cautious management. According to FDA labeling, metformin is contraindicated in patients with eGFR below 30 mL/min/1.73 m², and caution with dose adjustments is advised for those with eGFR between 30-45 mL/min/1.73 m². Your gastroenterologist and primary care provider or endocrinologist should coordinate this decision based on your most recent kidney function tests.
Metformin can typically be restarted once you have resumed normal oral intake and are adequately hydrated after the colonoscopy, provided you have no complications suggesting kidney injury. If you undergo a separate procedure with iodinated contrast, different guidelines apply, and metformin would typically be held at the time of contrast administration with kidney function rechecked before restarting.
Always follow your specific healthcare provider's instructions, as they will tailor recommendations to your individual medical history, kidney function, and procedural details. Never stop or restart metformin without explicit guidance from your medical team.
Lactic acidosis is a rare but potentially life-threatening complication characterized by excessive lactate accumulation in the bloodstream, resulting in metabolic acidosis. Metformin-associated lactic acidosis (MALA) occurs in fewer than 10 cases per 100,000 patient-years according to FDA labeling, but mortality rates can be significant when it does occur. The mechanism involves metformin's inhibition of mitochondrial respiratory chain complex I, which can shift cellular metabolism toward anaerobic pathways and lactate production when the drug accumulates to toxic levels.
Under normal circumstances, metformin is eliminated unchanged by the kidneys through glomerular filtration and tubular secretion. When kidney function declines—even temporarily—metformin clearance decreases, potentially leading to drug accumulation. Colonoscopy preparation creates several conditions that theoretically increase lactic acidosis risk: dehydration from bowel cleansing reduces renal blood flow, dietary restriction limits substrate availability, and gastrointestinal losses may cause electrolyte disturbances. These factors can transiently impair kidney function in susceptible individuals.
Despite theoretical concerns, evidence of increased lactic acidosis during colonoscopy preparation in patients continuing metformin is limited. The risk appears highest in patients with pre-existing renal impairment, advanced age (over 80 years), heart failure, liver disease, or conditions predisposing to tissue hypoxia. The type of bowel preparation also matters—polyethylene glycol (PEG)-based preparations are generally preferred in patients with chronic kidney disease to minimize acute kidney injury risk.
Clinical signs of lactic acidosis include muscle pain or weakness, unusual fatigue, difficulty breathing, abdominal discomfort, and altered mental status. These symptoms warrant immediate medical evaluation. The key to prevention is appropriate patient selection and risk stratification. Patients at higher baseline risk should have metformin held as a precautionary measure, while those with robust kidney function and no complicating factors may safely continue the medication with adequate hydration during bowel preparation.
Temporary discontinuation of metformin for colonoscopy requires careful attention to glycemic control, particularly in patients whose diabetes is not well-controlled on metformin alone or who take additional glucose-lowering medications. The colonoscopy preparation period presents unique challenges: dietary restrictions limit carbohydrate intake, which may lower blood glucose, while physiological stress and altered medication timing can cause unpredictable fluctuations.
For patients taking metformin monotherapy with well-controlled diabetes (typically defined as HbA1c less than 7%, though targets are individualized per ADA Standards of Care), a brief interruption of metformin typically does not cause significant hyperglycemia. These individuals should monitor blood glucose more frequently during the preparation period—ideally before meals and at bedtime—but often require no additional intervention. Maintaining adequate hydration with clear, sugar-free liquids during bowel preparation helps support metabolic stability.
Patients on combination therapy require more intensive management. Those taking sulfonylureas (such as glipizide or glimepiride) face hypoglycemia risk during fasting and should discuss dose reduction or temporary discontinuation with their provider. Insulin users need individualized adjustments, with basal insulin doses often reduced during the fasting period while monitoring glucose every 4 to 6 hours. SGLT2 inhibitors should generally be held 3 days before colonoscopy (4 days for ertugliflozin) due to diabetic ketoacidosis risk during fasting states, per FDA recommendations. For most patients on GLP-1 receptor agonists, these medications can be continued before elective procedures, though individual assessment is needed.
Practical strategies for maintaining glycemic stability include: following your endoscopy center's allowed clear-liquid list and choosing options with known carbohydrate content when needed; checking blood glucose every 4 to 6 hours during preparation; having rapid-acting glucose available for hypoglycemia (glucose tablets, juice); and contacting your healthcare provider if glucose falls below 70 mg/dL or rises above 250 mg/dL persistently. After the procedure, resume your normal diabetes regimen once you tolerate regular meals, following your provider's specific instructions for restarting metformin. Patients with consistently elevated glucose readings during the metformin interruption should discuss this with their diabetes care team, as it may indicate need for treatment intensification.
Most protocols recommend holding metformin on the morning of colonoscopy to minimize exposure during peak dehydration from bowel preparation. Always follow your specific endoscopy center's written instructions, as recommendations vary based on your kidney function and individual risk factors.
Metformin can typically be restarted once you resume normal oral intake and are adequately hydrated after colonoscopy, provided there are no complications suggesting kidney injury. If contrast imaging was performed separately, kidney function may need rechecking before restarting metformin per your provider's instructions.
Signs of lactic acidosis include muscle pain or weakness, unusual fatigue, difficulty breathing, abdominal discomfort, and altered mental status. These symptoms warrant immediate medical evaluation, though metformin-associated lactic acidosis remains rare, occurring in fewer than 10 cases per 100,000 patient-years.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.