LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Which GLP-1 is right for me? Choosing the appropriate GLP-1 receptor agonist depends on your individual health profile, treatment goals, and lifestyle preferences. These medications—including semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda)—work by mimicking a natural hormone that regulates blood sugar and appetite. While all GLP-1 medications effectively lower hemoglobin A1c and promote weight loss, they differ in dosing frequency, formulation, cardiovascular benefits, and side effect profiles. Understanding these distinctions, alongside your medical history and comorbidities, enables you and your healthcare provider to select the most suitable option for managing type 2 diabetes or weight.
Quick Answer: The right GLP-1 medication for you depends on your cardiovascular status, weight management goals, dosing preference (daily versus weekly), renal function, and insurance coverage.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications that mimic the action of a naturally occurring hormone in your body. GLP-1 is released by intestinal cells after eating and plays several important roles in glucose metabolism and appetite regulation. Understanding how these medications work can help you make informed decisions about your treatment options.
GLP-1 receptor agonists work through multiple mechanisms to improve glycemic control. They stimulate insulin secretion from pancreatic beta cells in a glucose-dependent manner, meaning they promote insulin release only when blood glucose levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications. Additionally, these agents suppress glucagon secretion from pancreatic alpha cells, which helps prevent the liver from releasing excess glucose into the bloodstream.
Beyond their effects on insulin and glucagon, GLP-1 medications slow gastric emptying, which moderates the rate at which nutrients enter the bloodstream after meals. This effect is more pronounced with short-acting GLP-1 agents and tends to diminish over time with long-acting formulations. Perhaps most notably for many patients, GLP-1 receptor agonists act on appetite centers in the brain, promoting satiety and reducing food intake. This mechanism has made these medications valuable not only for type 2 diabetes management but also for weight management in appropriate patients.
The glucose-dependent nature of insulin secretion with GLP-1 therapy represents a significant safety advantage. Unlike sulfonylureas or insulin, GLP-1 receptor agonists carry a low intrinsic risk of hypoglycemia when used as monotherapy. However, hypoglycemia risk increases when these agents are combined with insulin or insulin secretagogues, necessitating dose adjustments of concomitant medications in many cases.
It's important to note that GLP-1 receptor agonists are not indicated for type 1 diabetes or for the treatment of diabetic ketoacidosis (DKA).
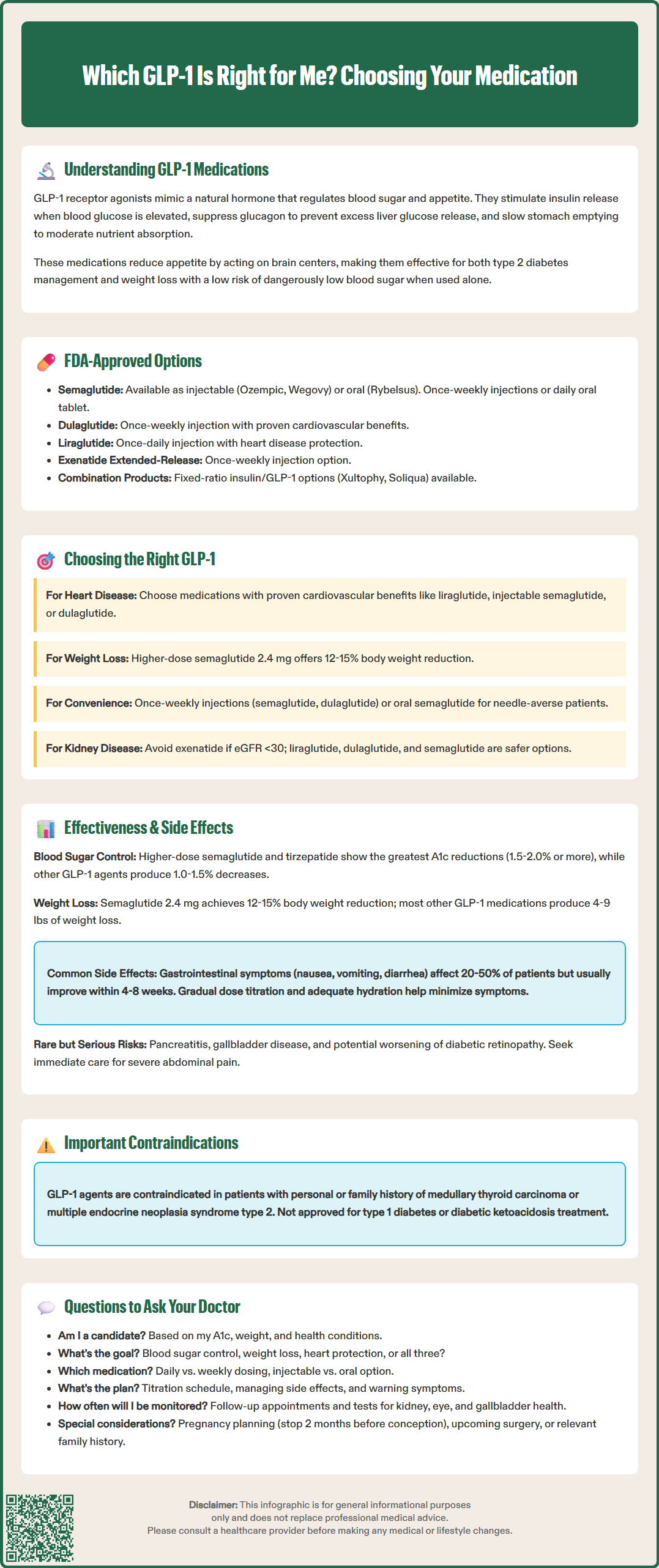
The FDA has approved several GLP-1 receptor agonists for clinical use, each with distinct characteristics regarding formulation, dosing frequency, and approved indications. Understanding these differences is essential for selecting the most appropriate option for individual patients.
Short-acting GLP-1 receptor agonists include exenatide (Byetta, with limited US availability) and lixisenatide (Adlyxin, discontinued in the US market). These medications are administered once or twice daily and have more pronounced effects on postprandial glucose due to their greater impact on gastric emptying. Exenatide is given twice daily within 60 minutes before morning and evening meals.
Long-acting GLP-1 receptor agonists offer less frequent dosing and include:
Dulaglutide (Trulicity): Once-weekly injection, available in single-dose pens ranging from 0.75 mg to 4.5 mg
Semaglutide (Ozempic, Wegovy): Once-weekly injection; Ozempic is approved for type 2 diabetes (0.25 mg to 2 mg), while Wegovy is approved for chronic weight management (up to 2.4 mg) and to reduce the risk of major adverse cardiovascular events in adults with established cardiovascular disease and either overweight or obesity
Exenatide extended-release (Bydureon BCise): Once-weekly injection using microsphere technology
Liraglutide (Victoza, Saxenda): Once-daily injection; Victoza for diabetes (up to 1.8 mg), Saxenda for weight management (up to 3 mg)
Oral GLP-1 option: Semaglutide (Rybelsus) is the only oral GLP-1 receptor agonist, taken once daily on an empty stomach with specific administration requirements: take with no more than 4 ounces of plain water, at least 30 minutes before eating, drinking, or taking other oral medications, and swallow tablets whole without breaking or chewing.
Fixed-ratio combinations of insulin and GLP-1 receptor agonists are also available, including insulin degludec/liraglutide (Xultophy 100/3.6) and insulin glargine/lixisenatide (Soliqua 100/33).
Several GLP-1 receptor agonists have demonstrated cardiovascular benefits in outcome trials. Liraglutide, injectable semaglutide, and dulaglutide have shown statistically significant reductions in major adverse cardiovascular events in patients with established cardiovascular disease or multiple risk factors. These cardiovascular benefits have influenced treatment algorithms, with guidelines recommending GLP-1 receptor agonists with proven cardiovascular benefit for patients with type 2 diabetes and atherosclerotic cardiovascular disease.
It's worth noting that tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist, representing a distinct but related medication class with similar clinical effects.
Selecting the most appropriate GLP-1 receptor agonist requires consideration of multiple patient-specific factors, clinical characteristics, and treatment goals. A personalized approach ensures optimal therapeutic outcomes while minimizing potential adverse effects and maximizing adherence.
Clinical indications and comorbidities play a primary role in medication selection. If you have established atherosclerotic cardiovascular disease, a GLP-1 receptor agonist with proven cardiovascular benefit would be appropriate. For heart failure or chronic kidney disease, the American Diabetes Association generally recommends SGLT2 inhibitors as first-line agents, with GLP-1 receptor agonists considered for their benefits on atherosclerotic cardiovascular disease, glycemic control, and weight management, or when SGLT2 inhibitors are not appropriate.
For patients primarily seeking weight management, either with or without type 2 diabetes, higher-dose formulations such as semaglutide 2.4 mg (Wegovy) or liraglutide 3 mg (Saxenda) may be more appropriate. Clinical trials have demonstrated greater weight loss with these higher doses compared to diabetes-indicated doses, with Wegovy producing average weight reductions of 12-15% of body weight. However, insurance coverage for weight management indications varies significantly and may influence practical treatment decisions.
Dosing frequency and administration preferences significantly impact adherence and patient satisfaction. Once-weekly options like semaglutide, dulaglutide, or exenatide extended-release offer convenience for patients who prefer less frequent injections. The oral formulation of semaglutide (Rybelsus) provides an alternative for patients with needle aversion, though it requires specific administration instructions—taken on an empty stomach with no more than 4 ounces of water, at least 30 minutes before any food, beverage, or other oral medications, and swallowed whole.
Renal function must be considered, as some GLP-1 agents require dose adjustment or have limitations in advanced chronic kidney disease. Exenatide products should be avoided in severe renal impairment (eGFR <30 mL/min/1.73m²), while liraglutide, dulaglutide, and semaglutide can generally be used across a broader range of renal function. Always consult product-specific labeling for current recommendations.
Additional considerations include diabetic retinopathy status (semaglutide may worsen retinopathy in some patients with pre-existing disease, particularly with rapid A1c improvement), history of pancreatitis (use GLP-1 agents with caution), and upcoming surgical procedures (discuss with your surgical/anesthesia team due to effects on gastric emptying). Patients with severe gastrointestinal disease may require careful consideration and monitoring.
While all GLP-1 receptor agonists effectively lower hemoglobin A1c and promote weight loss, there are meaningful differences in their magnitude of effect, titration schedules, and adverse effect profiles that influence clinical decision-making.
Glycemic efficacy varies across the GLP-1 class. Network meta-analyses suggest that higher-dose semaglutide (1 mg and 2 mg weekly) and tirzepatide (a dual GIP/GLP-1 receptor agonist) demonstrate superior A1c reductions compared to other agents in the class, with mean reductions of 1.5–2.0% or greater from baseline. Dulaglutide and liraglutide show intermediate efficacy with A1c reductions of approximately 1.0–1.5%, while exenatide twice daily demonstrates somewhat more modest effects. However, head-to-head comparisons are limited, and individual patient responses vary considerably.
Weight loss outcomes similarly show a gradient of effectiveness. In clinical trials, once-weekly semaglutide at diabetes doses (0.5–1 mg) produces mean weight loss of 4–6 kg (9–13 lbs), while the 2.4 mg dose (Wegovy) achieves average weight reductions of 12–15% of body weight. Liraglutide 3 mg produces mean weight loss of approximately 5–8 kg (11–18 lbs). Other GLP-1 agents typically result in weight reductions of 2–4 kg (4–9 lbs), which remains clinically meaningful for many patients.
Gastrointestinal side effects represent the most common adverse events across the GLP-1 class. Nausea, vomiting, diarrhea, and constipation occur in 20–50% of patients, though symptoms are typically mild to moderate and diminish over time. Gradual dose titration significantly reduces gastrointestinal intolerance. Starting at lower doses and increasing according to product-specific schedules (ranging from 1-4 weeks depending on the agent) allows physiologic adaptation. Patients should be counseled that gastrointestinal symptoms usually improve within 4–8 weeks of reaching a stable dose. Maintaining adequate hydration is important, as dehydration from gastrointestinal symptoms can increase the risk of acute kidney injury.
Injection site reactions occur with subcutaneous formulations but are generally mild. Exenatide extended-release may cause small, persistent nodules at injection sites. Rare but serious adverse effects include pancreatitis (though causality remains uncertain), gallbladder disease, and potential thyroid C-cell tumors (observed in rodent studies but not conclusively demonstrated in humans). Semaglutide carries a warning about potential worsening of diabetic retinopathy, particularly in patients with pre-existing retinopathy and rapid improvement in glucose control.
GLP-1 receptor agonists are contraindicated in patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2. Patients should be advised to seek immediate medical attention for severe, persistent abdominal pain that may indicate pancreatitis.
Engaging in informed discussion with your healthcare provider is essential for determining whether GLP-1 therapy is appropriate for you and, if so, which specific agent best aligns with your clinical needs and personal preferences. Preparing thoughtful questions facilitates shared decision-making and ensures you understand the rationale, expectations, and monitoring requirements for your treatment plan.
Questions about appropriateness and goals:
Based on my current A1c, weight, and other health conditions, am I a candidate for GLP-1 therapy?
What are the primary goals of treatment—is it mainly for blood sugar control, weight management, cardiovascular protection, or a combination?
How does a GLP-1 medication fit with my other diabetes medications? Will any of my current medications need to be adjusted?
Do I have any contraindications or conditions that would make GLP-1 therapy inappropriate for me?
Should I consider an SGLT2 inhibitor instead of or in addition to a GLP-1 medication, especially if I have heart failure or kidney disease?
Questions about medication selection:
Which specific GLP-1 medication do you recommend for me, and why?
Are there alternatives within the GLP-1 class that might also be suitable?
How does dosing frequency (daily versus weekly) affect the choice?
Is the oral formulation an option for me if I'm uncomfortable with injections?
Questions about practical considerations:
What is the titration schedule, and how long before I reach the target dose?
What side effects should I expect, and how can I manage them?
What symptoms would require me to contact you or seek urgent medical attention?
How will we monitor my response to treatment, and how often will I need follow-up appointments?
Will you be monitoring my kidney function, retinopathy status, and checking for gallbladder disease?
Does my insurance cover the recommended medication, and are there more affordable alternatives if coverage is an issue?
If I'm planning to have surgery or a procedure requiring anesthesia, how should I manage my GLP-1 medication?
Your physician should also assess for contraindications, including personal or family history of medullary thyroid carcinoma, multiple endocrine neoplasia syndrome type 2, or history of severe gastrointestinal disease. If you're planning pregnancy or currently pregnant, GLP-1 therapy is generally not recommended, and alternative treatments should be discussed. For those planning pregnancy, specific washout periods apply (e.g., discontinue semaglutide at least 2 months before planned conception). Open communication about your lifestyle, preferences, and concerns enables your healthcare team to tailor GLP-1 therapy to your individual circumstances, optimizing both clinical outcomes and quality of life.
Once-weekly GLP-1 medications like semaglutide (Ozempic) and dulaglutide (Trulicity) offer greater convenience with less frequent injections, while once-daily options like liraglutide (Victoza) may provide more consistent day-to-day effects. Both formulations effectively lower blood sugar and promote weight loss, with the choice depending on your lifestyle preferences and adherence patterns.
Most GLP-1 medications can be used in chronic kidney disease, but exenatide products should be avoided when eGFR is below 30 mL/min/1.73m². Semaglutide, dulaglutide, and liraglutide generally do not require dose adjustment across a broader range of renal function, though you should always consult your healthcare provider for personalized recommendations.
Liraglutide (Victoza), injectable semaglutide (Ozempic), and dulaglutide (Trulicity) have demonstrated statistically significant reductions in major adverse cardiovascular events in clinical trials. If you have established atherosclerotic cardiovascular disease, your healthcare provider will likely recommend one of these agents with proven cardiovascular benefit.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.