LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can metformin increase blood pressure? This common question arises among patients prescribed this first-line diabetes medication. Metformin, a biguanide antihyperglycemic agent, is widely used to manage type 2 diabetes by reducing hepatic glucose production and improving insulin sensitivity. Understanding metformin's actual effects on blood pressure is essential for patients and clinicians alike. Clinical evidence consistently shows that metformin does not elevate blood pressure and may even contribute to modest reductions. This article examines the relationship between metformin and blood pressure, explores factors that may influence readings, and provides guidance on when to seek medical attention.
Quick Answer: Metformin does not increase blood pressure and may actually contribute to modest reductions in both systolic and diastolic measurements.
Metformin is a first-line oral medication widely prescribed for the management of type 2 diabetes mellitus. As a biguanide antihyperglycemic agent, metformin works primarily by decreasing hepatic glucose production, reducing intestinal absorption of glucose, and improving insulin sensitivity in peripheral tissues. Unlike sulfonylureas or insulin, metformin does not typically cause hypoglycemia when used as monotherapy, though the risk increases when combined with insulin or insulin secretagogues.
The medication is available in immediate-release and extended-release formulations, with typical starting doses of 500 mg daily with meals, gradually titrated to effective doses ranging from 1,000-2,550 mg daily (divided or once daily depending on formulation). According to current American Diabetes Association (ADA) guidelines, initial therapy should be individualized; in patients with established atherosclerotic cardiovascular disease (ASCVD), heart failure, or chronic kidney disease, GLP-1 receptor agonists or SGLT2 inhibitors may be initiated independent of metformin.
Some evidence, primarily from the UKPDS 34 trial in overweight patients with type 2 diabetes, suggests potential cardiovascular benefits with metformin, though this is not an FDA-approved indication. Metformin is generally associated with weight neutrality or modest weight loss rather than the weight gain seen with some other diabetes medications.
Metformin is generally well-tolerated, though gastrointestinal side effects—including diarrhea, nausea, and abdominal discomfort—are common, particularly during initiation. These effects can often be minimized through gradual dose titration and taking the medication with meals. Long-term use may be associated with vitamin B12 deficiency, warranting periodic monitoring, especially in patients with anemia or neuropathy. Metformin is contraindicated in patients with an eGFR <30 mL/min/1.73m², should not be initiated in those with an eGFR between 30-45 mL/min/1.73m², and requires temporary discontinuation during iodinated contrast imaging procedures in certain risk groups.
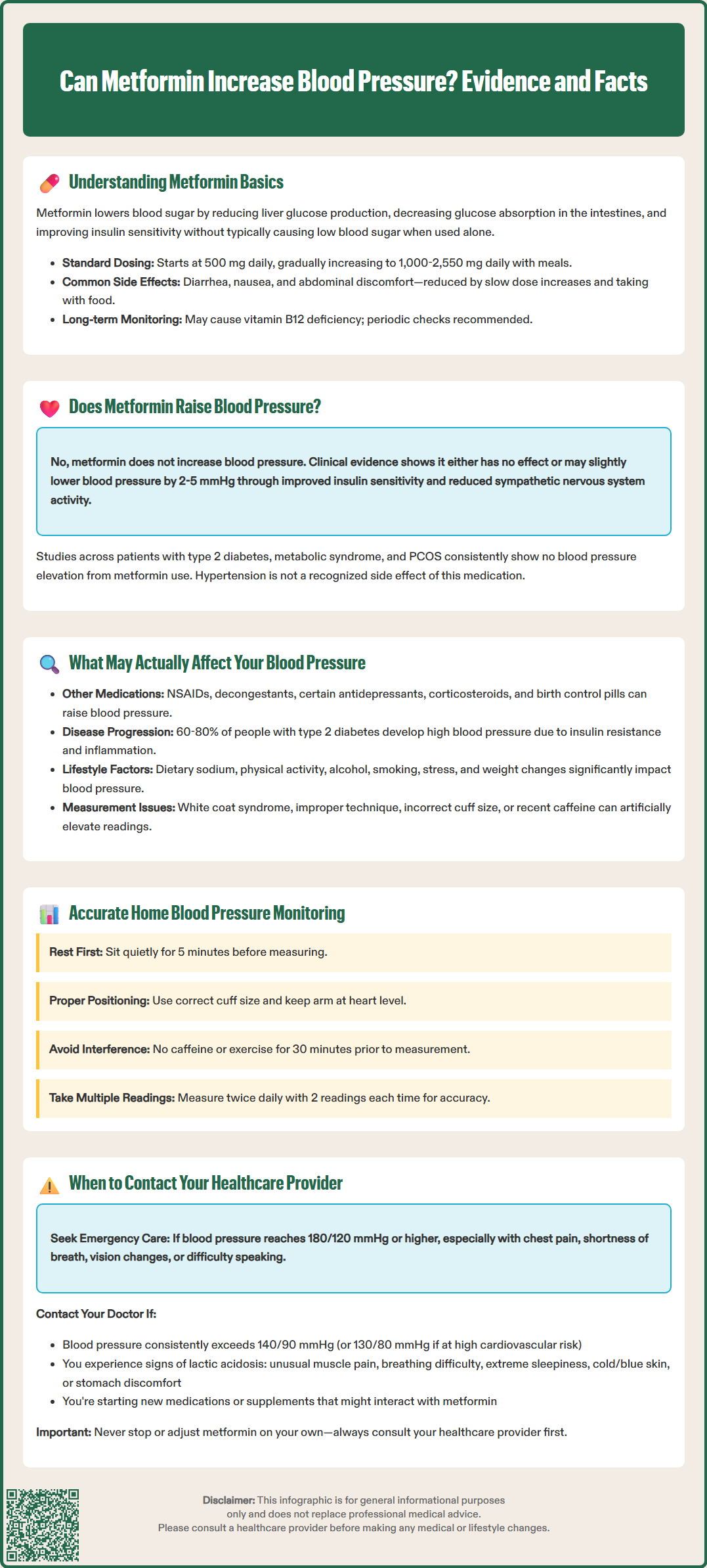
There is no established clinical evidence that metformin increases blood pressure. In fact, the available research suggests the opposite relationship. Multiple clinical studies and meta-analyses have demonstrated that metformin either has a neutral effect on blood pressure or may contribute to modest reductions in both systolic and diastolic blood pressure measurements (approximately 2-5 mmHg in some studies). The FDA-approved prescribing information for metformin does not list hypertension or elevated blood pressure as a recognized adverse effect of the medication.
Several mechanisms may explain metformin's blood pressure-neutral or potentially beneficial effects. The medication improves insulin sensitivity, and insulin resistance is closely linked with hypertension through multiple pathways, including increased sympathetic nervous system activity, sodium retention, and vascular smooth muscle proliferation. By addressing insulin resistance, metformin may indirectly support healthier blood pressure regulation. Additionally, some studies have reported that metformin may improve endothelial function—the ability of blood vessels to dilate appropriately—which plays a role in blood pressure control.
Clinical trials in patients with type 2 diabetes, metabolic syndrome, and polycystic ovary syndrome (PCOS) have consistently failed to demonstrate blood pressure elevation with metformin therapy. It should be noted that metformin use for PCOS is considered off-label in the United States. The blood pressure effects have been observed across diverse patient populations, including those with and without baseline hypertension.
If a patient experiences elevated blood pressure readings after starting metformin, alternative explanations should be explored. These may include progression of underlying cardiovascular disease, dietary changes, medication interactions, stress, inadequate diabetes control itself, or the natural variability of blood pressure measurements. Healthcare providers should conduct a comprehensive evaluation rather than attributing blood pressure changes to metformin without considering other contributing factors.
While metformin itself does not increase blood pressure, several factors may influence blood pressure readings in patients taking this medication. Understanding these variables is essential for accurate clinical assessment and appropriate management decisions.
Concurrent medications represent a significant consideration. Many patients with type 2 diabetes take multiple medications, and some of these may affect blood pressure. Nonsteroidal anti-inflammatory drugs (NSAIDs), decongestants containing pseudoephedrine or phenylephrine, certain antidepressants (particularly SNRIs), corticosteroids, stimulants for ADHD, oral contraceptives/estrogens, calcineurin inhibitors, atypical antipsychotics, erythropoietin, COX-2 inhibitors, and even licorice can all elevate blood pressure. Additionally, some diabetes medications may influence blood pressure—SGLT2 inhibitors and GLP-1 receptor agonists often reduce blood pressure, while thiazolidinediones may cause fluid retention.
Disease progression and comorbidities also play important roles. Type 2 diabetes is frequently accompanied by hypertension, with approximately 60-80% of patients with diabetes eventually developing high blood pressure. Other conditions like obstructive sleep apnea and chronic kidney disease can further complicate blood pressure control. The coexistence of these conditions reflects shared pathophysiologic mechanisms, including insulin resistance, inflammation, and endothelial dysfunction. As diabetes progresses, particularly if glycemic control is suboptimal, the risk of developing or worsening hypertension increases independently of medication effects.
Lifestyle factors significantly impact blood pressure in patients with diabetes. Dietary sodium intake, physical activity levels, alcohol consumption, smoking status, and stress all influence blood pressure regulation. Patients initiating metformin may simultaneously make dietary changes—some beneficial, others potentially problematic—that affect blood pressure. Weight changes, whether intentional or unintentional, also correlate with blood pressure fluctuations.
Measurement technique and timing can introduce variability. Blood pressure naturally fluctuates throughout the day, and readings may be elevated due to "white coat hypertension" (anxiety in medical settings), improper cuff size, incorrect arm positioning, or recent caffeine intake. For home blood pressure monitoring, the American Heart Association recommends resting 5 minutes before measurement, using the correct cuff size, avoiding caffeine/exercise for 30 minutes prior, positioning the arm at heart level, and taking 2 readings twice daily for several days.
Patients taking metformin should maintain regular communication with their healthcare providers regarding any changes in their health status, including blood pressure concerns. Specific situations warrant prompt medical attention to ensure appropriate evaluation and management.
Contact your healthcare provider if you experience:
Consistently elevated blood pressure readings above your target range, particularly if systolic pressure exceeds 140 mmHg or diastolic pressure exceeds 90 mmHg on multiple occasions. For patients with diabetes, the American Diabetes Association generally recommends blood pressure targets of less than 140/90 mmHg for most individuals; targets of less than 130/80 mmHg may be considered for those at high atherosclerotic cardiovascular disease risk if they can be safely achieved.
Blood pressure readings of 180/120 mmHg or higher should be rechecked after 5 minutes. If readings remain at this level, especially with symptoms such as chest pain, shortness of breath, back pain, numbness/weakness, change in vision, or difficulty speaking, call 911 or seek emergency medical care immediately as this may indicate a hypertensive emergency.
Symptoms potentially related to high blood pressure, including severe headaches, vision changes, chest pain, shortness of breath, irregular heartbeat, or nosebleeds. While hypertension is often asymptomatic, these symptoms may indicate hypertensive urgency or emergency requiring immediate evaluation.
Signs of possible lactic acidosis (a rare but serious side effect of metformin) such as unusual muscle pain, difficulty breathing, unusual sleepiness, cold or blue skin, dizziness, or stomach discomfort with nausea/vomiting. If these occur, stop taking metformin and seek emergency medical care immediately.
New or worsening symptoms after starting metformin or adjusting the dose, even if they seem unrelated to blood pressure.
Concerns about medication interactions, particularly if you've started new medications—prescription, over-the-counter, or supplements—that might affect blood pressure or interact with metformin.
Regular monitoring is essential for patients with diabetes. The American College of Physicians (ACP) and ADA recommend blood pressure screening at every routine diabetes visit. Initial evaluation of elevated blood pressure typically includes basic metabolic panel, kidney function tests, urine albumin-to-creatinine ratio, lipid panel, and A1C measurement. Your healthcare provider may refer you to a specialist if you have resistant hypertension (requiring 3 or more medications including a diuretic), chronic kidney disease stage 3 or higher, or suspected secondary causes of hypertension.
Never discontinue metformin or adjust your dose without medical guidance, except in cases of suspected lactic acidosis or as instructed before certain imaging procedures with iodinated contrast. Your provider should reassess kidney function before restarting metformin after such procedures.
No, metformin does not cause high blood pressure. Clinical evidence shows metformin has either neutral effects or may modestly reduce blood pressure by approximately 2-5 mmHg, and hypertension is not listed as a recognized adverse effect in FDA prescribing information.
If blood pressure increases after starting metformin, alternative explanations should be explored, including concurrent medications (NSAIDs, decongestants, corticosteroids), progression of underlying cardiovascular disease, dietary changes, stress, inadequate diabetes control, or natural blood pressure variability rather than metformin itself.
The American Diabetes Association generally recommends blood pressure targets of less than 140/90 mmHg for most individuals with diabetes. Targets of less than 130/80 mmHg may be considered for those at high atherosclerotic cardiovascular disease risk if they can be safely achieved.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.