LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes management, chronic weight management, and cardiovascular risk reduction. As its use expands, patients with Crohn's disease—a chronic inflammatory bowel condition—face important questions about safety and compatibility. Both semaglutide and Crohn's disease affect the gastrointestinal system, raising concerns about overlapping side effects, symptom management, and potential disease interactions. Understanding the current evidence, risks, and clinical considerations is essential for patients and healthcare providers navigating treatment decisions when these two conditions intersect.
Quick Answer: Semaglutide is not contraindicated in Crohn's disease, but requires individualized assessment based on disease activity, nutritional status, and gastrointestinal symptom tolerance.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under the brand names Ozempic and Rybelsus), chronic weight management (Wegovy), and cardiovascular risk reduction in specific populations. For patients with type 2 diabetes and established cardiovascular disease, Ozempic is indicated to reduce cardiovascular risk, while Wegovy is approved for cardiovascular risk reduction in adults with obesity/overweight and established cardiovascular disease. Semaglutide is not indicated for type 1 diabetes treatment.
The medication works by mimicking the naturally occurring GLP-1 hormone, which stimulates insulin secretion in response to food intake, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. These mechanisms contribute to improved glycemic control and significant weight loss in clinical trials.
Crohn's disease is a chronic inflammatory bowel disease (IBD) that can affect any part of the gastrointestinal tract from mouth to anus, though it most commonly involves the terminal ileum and colon. The condition is characterized by transmural inflammation, meaning it affects the full thickness of the bowel wall, and can lead to complications including strictures, fistulas, and abscesses. Patients with Crohn's disease often experience abdominal pain, diarrhea, weight loss, fatigue, and malnutrition.
The intersection of semaglutide use and Crohn's disease raises important clinical considerations. Both conditions involve the gastrointestinal system, and semaglutide's mechanism of slowing gastric emptying and its gastrointestinal side effect profile may have implications for individuals with pre-existing inflammatory bowel disease. Understanding how these two conditions may interact is essential for safe prescribing and patient counseling, particularly as semaglutide becomes increasingly prescribed for weight management in diverse patient populations.
Crohn's disease is not explicitly listed as a contraindication to semaglutide use in the FDA prescribing information. The primary contraindications include a personal or family history of medullary thyroid carcinoma and multiple endocrine neoplasia syndrome type 2 (MEN 2). For Wegovy specifically, pregnancy is a contraindication, and women of childbearing potential should use effective contraception during treatment. Additionally, semaglutide is not recommended in patients with severe gastroparesis, which may be relevant for Crohn's patients with motility complications.
Clinical judgment must be individualized based on several factors. Patients with well-controlled Crohn's disease in remission may be considered differently than those with active inflammation, frequent flares, or complications such as strictures or fistulas. The decision requires careful assessment of disease activity, current symptoms, nutritional status, and the specific indication for semaglutide therapy. For patients with type 2 diabetes and Crohn's disease, the benefits of improved glycemic control must be weighed against potential gastrointestinal risks.
Gastroenterologists and prescribing physicians should collaborate when considering semaglutide for patients with IBD. Key considerations include:
Disease activity status: Active inflammation may increase susceptibility to adverse effects
Nutritional state: Patients already experiencing malabsorption or weight loss may not be appropriate candidates for medications that further reduce appetite
Stricture presence: Delayed gastric emptying could theoretically worsen symptoms in patients with bowel narrowing
Medication interactions: While subcutaneous semaglutide has minimal effects on most oral drug absorption, specific medications (such as levothyroxine with oral semaglutide/Rybelsus) may require monitoring
Hypoglycemia risk: For patients with diabetes using insulin or sulfonylureas, dose reductions of these medications may be needed when starting semaglutide
Diabetic retinopathy: Patients with pre-existing diabetic retinopathy should be monitored for worsening eye disease
There is currently insufficient evidence to provide definitive guidance, making shared decision-making between patient and healthcare team essential.
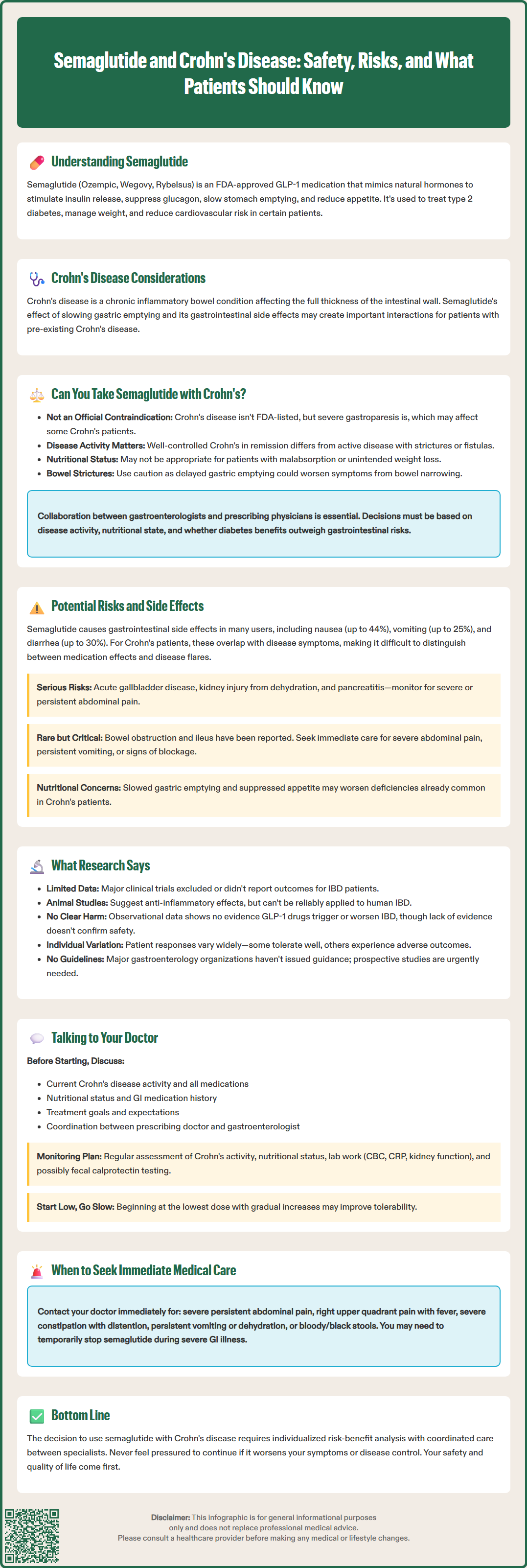
Semaglutide is associated with a well-established profile of gastrointestinal adverse effects, which occur in a substantial proportion of users. The most common side effects include nausea (occurring in up to 44% of patients at weight-loss doses), vomiting (up to 25%), diarrhea (up to 30%), abdominal pain, and constipation. These effects are typically dose-dependent, most pronounced during dose escalation, and tend to diminish over time as patients develop tolerance. However, for individuals with Crohn's disease, these overlapping symptoms may be particularly problematic.
The mechanism behind semaglutide's gastrointestinal effects relates primarily to delayed gastric emptying and effects on gastrointestinal motility. While this contributes to satiety and weight loss, it may complicate symptom management in Crohn's patients who already experience unpredictable bowel patterns. Distinguishing between medication side effects and disease flares becomes challenging when symptoms overlap significantly.
Specific concerns for Crohn's patients include:
Nausea and vomiting: May exacerbate existing symptoms or lead to dehydration, particularly concerning in patients with active disease
Diarrhea: Difficult to differentiate from Crohn's-related diarrhea, potentially delaying recognition of disease flares
Abdominal pain: May mask or mimic Crohn's-related pain, complicating clinical assessment
Reduced oral intake: Appetite suppression combined with nausea may worsen nutritional deficiencies common in IBD
Additional FDA-labeled risks include:
Acute gallbladder disease: Cholelithiasis and cholecystitis occur more frequently with semaglutide, particularly with rapid weight loss
Acute kidney injury: Dehydration from gastrointestinal side effects may lead to kidney injury
Pancreatitis: Patients should be monitored for severe, persistent abdominal pain, sometimes radiating to the back
Rare but serious gastrointestinal adverse events reported in post-marketing surveillance include cases of bowel obstruction and ileus. While causality remains uncertain, patients with pre-existing bowel disease may theoretically face elevated risk. Patients should be counseled to seek immediate medical attention for severe abdominal pain, persistent vomiting, or signs of bowel obstruction.
Current research specifically examining semaglutide or other GLP-1 receptor agonists in patients with inflammatory bowel disease remains limited. The pivotal clinical trials for semaglutide (SUSTAIN and STEP programs) did not specifically enroll or report outcomes for patients with Crohn's disease or ulcerative colitis, representing a significant knowledge gap in the literature.
Emerging evidence suggests complex interactions between GLP-1 pathways and intestinal inflammation. Some preclinical studies have identified GLP-1 receptors in the intestinal epithelium and immune cells, with animal models suggesting potential anti-inflammatory properties of GLP-1 agonists. A 2019 study in experimental colitis models demonstrated that GLP-1 receptor activation reduced inflammatory markers and improved intestinal barrier function. However, translating these findings to human IBD requires caution, as animal models do not fully replicate the complexity of Crohn's disease.
Recent US observational cohort studies and pharmacovigilance databases have not identified a clear signal of IBD exacerbation with GLP-1 medications, though systematic studies are limited by confounding factors and selection bias. There is no established evidence that semaglutide triggers new-onset IBD or worsens existing disease, but the absence of evidence should not be interpreted as evidence of safety in this specific population.
Case reports and small case series have described both tolerability and adverse outcomes in IBD patients receiving GLP-1 agonists, highlighting the need for individualized assessment. The American Gastroenterological Association and other professional societies have not issued specific guidance on GLP-1 use in IBD, reflecting the current uncertainty. Prospective studies examining safety, efficacy, and disease activity markers in IBD patients receiving semaglutide are needed to inform evidence-based recommendations.
If you have Crohn's disease and are considering semaglutide for diabetes management or weight loss, open communication with your healthcare team is essential. This conversation should involve both your prescribing physician (endocrinologist or primary care provider) and your gastroenterologist to ensure coordinated care and comprehensive risk assessment.
Before starting semaglutide, discuss the following with your medical team:
Current disease status: Provide detailed information about your Crohn's activity, recent flares, and symptom patterns
Treatment regimen: Review all current medications, including immunosuppressants, biologics, and symptom management drugs
Nutritional status: Discuss any weight loss, malabsorption issues, or dietary restrictions
Previous gastrointestinal tolerance: Share your history with medications that affect the GI tract
Treatment goals: Clarify whether semaglutide is being considered for diabetes control, weight management, or cardiovascular risk reduction, and discuss alternative options
Pregnancy planning: Women of childbearing potential should discuss contraception, as Wegovy is contraindicated in pregnancy
Your physician should establish a monitoring plan that includes regular assessment of Crohn's disease activity, nutritional parameters, and medication side effects. Laboratory monitoring (CBC, CRP, kidney function) and possibly fecal calprotectin testing may help distinguish between medication side effects and disease flares. For patients with diabetes, blood glucose monitoring and potential insulin/sulfonylurea dose adjustments should be planned.
Seek immediate medical attention for these red-flag symptoms:
Severe persistent abdominal pain, especially if radiating to the back (possible pancreatitis)
Right upper quadrant pain with fever or jaundice (possible gallbladder disease)
Severe constipation with abdominal distention or inability to pass gas (possible obstruction)
Persistent vomiting or signs of dehydration
Bloody or black stools
Consider temporarily holding semaglutide during acute severe gastrointestinal illness or dehydration, in coordination with your prescribing physician. If semaglutide is initiated, starting at the lowest dose with gradual titration may improve tolerability. Regular follow-up appointments during the initial months allow for timely intervention if problems arise. Ultimately, the decision to use semaglutide in Crohn's disease requires individualized risk-benefit analysis, and patients should never feel pressured to continue a medication that worsens their quality of life or disease control.
Semaglutide is not contraindicated in Crohn's disease, but safety depends on individual factors including disease activity, nutritional status, and presence of complications like strictures. Patients should work closely with both their gastroenterologist and prescribing physician to assess risks and benefits.
There is no established evidence that semaglutide triggers Crohn's flares, but its gastrointestinal side effects (nausea, diarrhea, abdominal pain) can overlap with and potentially mask disease symptoms. Distinguishing between medication effects and disease activity requires careful monitoring.
Patients should monitor for severe persistent abdominal pain, persistent vomiting, signs of dehydration, bowel obstruction symptoms, or worsening Crohn's symptoms. Regular follow-up with healthcare providers and laboratory monitoring can help distinguish medication side effects from disease flares.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.