LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can semaglutide cause joint pain? This question concerns many patients prescribed this GLP-1 receptor agonist for type 2 diabetes or weight management. While joint pain is not listed among semaglutide's common side effects in FDA prescribing information, some patients report musculoskeletal discomfort during treatment. Understanding the relationship between semaglutide and joint symptoms—whether direct, indirect, or coincidental—is essential for appropriate clinical management. This article examines the evidence, explores potential mechanisms, and provides guidance on when joint pain warrants medical evaluation.
Quick Answer: Semaglutide is not established to directly cause joint pain based on FDA clinical trial data, though some patients report musculoskeletal discomfort that may result from indirect factors such as rapid weight loss or biomechanical changes.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, occurring in a substantial proportion of patients. According to the FDA prescribing information, these include nausea, vomiting, diarrhea, abdominal pain, and constipation. These symptoms typically emerge during dose escalation and often diminish over time as the body adjusts to the medication. The gastrointestinal effects are directly related to semaglutide's mechanism of slowing gastric emptying.
Other recognized adverse effects include injection site reactions (for subcutaneous formulations), headache, fatigue, and dizziness, with some variation between products. More serious but less common risks include pancreatitis, gallbladder disease, acute kidney injury (usually secondary to dehydration from gastrointestinal symptoms), and diabetic retinopathy complications, particularly in patients with pre-existing retinopathy who experience rapid improvement in blood glucose. Semaglutide carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2. Wegovy is also contraindicated during pregnancy.
The American Diabetes Association's Standards of Care emphasizes the importance of patient education regarding these potential adverse effects and appropriate monitoring during treatment initiation and dose titration.
Understanding the established safety profile of semaglutide provides important context when evaluating less commonly reported symptoms, including musculoskeletal complaints such as joint pain, which patients and clinicians may encounter in clinical practice.
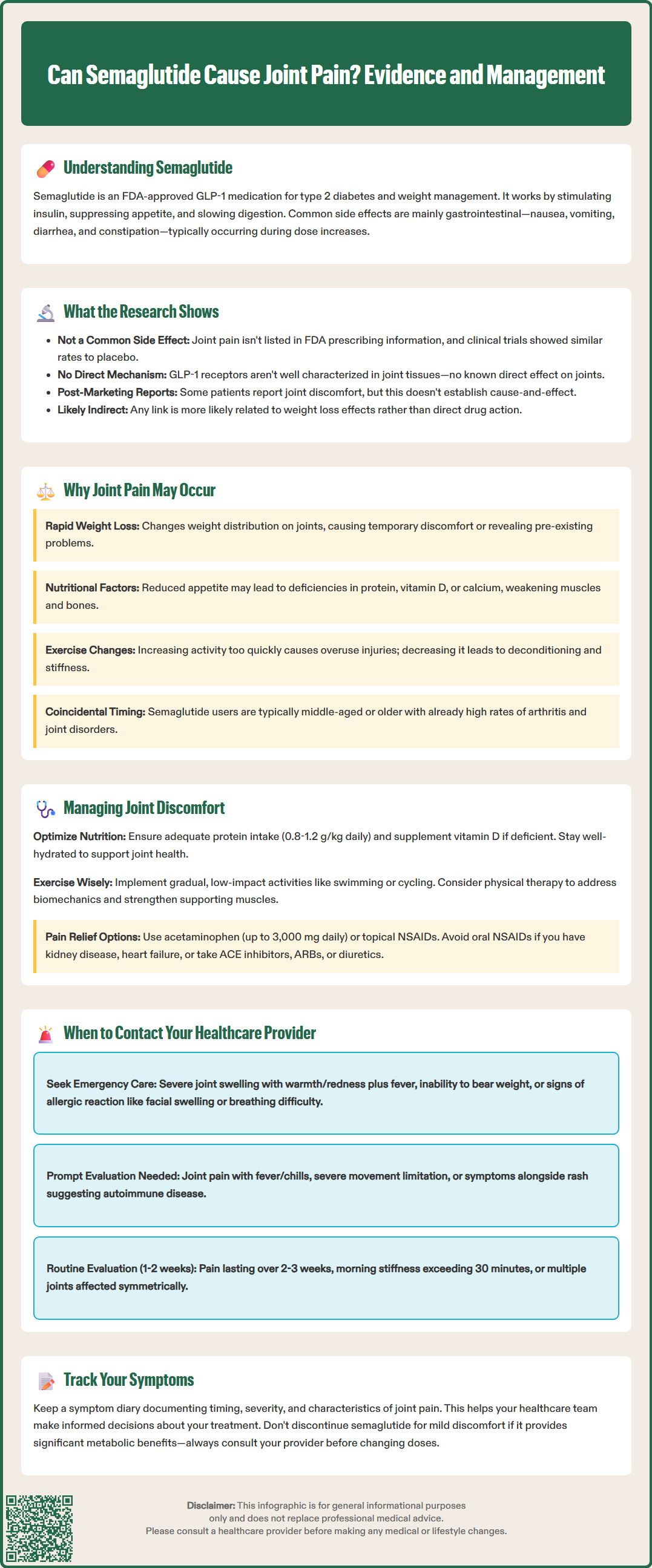
Joint pain, or arthralgia, is not listed among the common adverse effects in the FDA-approved prescribing information for semaglutide formulations. In the pivotal clinical trials that led to FDA approval—including the SUSTAIN trials for diabetes management and the STEP trials for weight management—musculoskeletal symptoms including joint pain were reported, but at rates generally comparable to placebo groups. This suggests there is no established direct causal relationship between semaglutide and joint pain based on controlled clinical trial data.
However, post-marketing surveillance and clinical experience have documented patient reports of joint discomfort during semaglutide treatment. The FDA Adverse Event Reporting System (FAERS) contains reports of arthralgia and musculoskeletal pain in patients taking GLP-1 receptor agonists, though these spontaneous reports have significant limitations including underreporting and inability to establish causation. These reports may reflect coincidental associations or indirect mechanisms rather than direct drug effects.
It is important to distinguish between a direct pharmacological effect and indirect consequences of treatment. The current evidence does not support a direct mechanism by which semaglutide would cause joint inflammation or damage. While GLP-1 receptors are expressed primarily in pancreatic beta cells, the gastrointestinal tract, and certain areas of the central nervous system, the expression and function of these receptors in joint tissues is not well characterized. Therefore, any association between semaglutide use and joint symptoms is more likely to be indirect rather than a direct drug effect on articular structures, though this remains an area of ongoing research.
Clinicians should maintain awareness that the absence of a recognized association does not mean patients will not experience joint symptoms during treatment, and each case warrants individual clinical assessment to determine the underlying cause and appropriate management strategy.
Several indirect mechanisms may explain why some patients experience joint discomfort while taking semaglutide, even in the absence of a direct pharmacological effect on joint tissues. Understanding these potential contributing factors is essential for appropriate clinical evaluation and management.
Rapid weight loss represents the most plausible explanation for musculoskeletal symptoms in patients taking semaglutide, particularly at higher doses used for weight management. Significant weight reduction alters biomechanical loading patterns on weight-bearing joints, potentially causing temporary discomfort as the musculoskeletal system adapts. Conversely, rapid weight loss may also unmask pre-existing degenerative joint disease that was previously asymptomatic or less symptomatic. Studies of bariatric surgery patients have documented similar phenomena, where rapid weight changes can temporarily exacerbate joint symptoms before eventual improvement occurs.
Nutritional factors may also contribute to musculoskeletal complaints. Patients experiencing significant appetite suppression and reduced caloric intake may inadvertently develop nutritional deficiencies, including inadequate protein intake, vitamin D deficiency, or insufficient calcium consumption. These nutritional imbalances can affect muscle strength, bone health, and overall musculoskeletal function. Additionally, dehydration resulting from gastrointestinal side effects may contribute to muscle cramping and joint stiffness.
Changes in physical activity patterns frequently accompany weight loss treatment. Patients may increase exercise intensity or duration as they lose weight and gain confidence, potentially leading to overuse injuries or delayed-onset muscle soreness that may be perceived as joint pain. Alternatively, some patients may reduce activity due to gastrointestinal side effects or fatigue, leading to deconditioning and subsequent discomfort when resuming normal activities.
Finally, coincidental conditions must always be considered. The demographic most commonly prescribed semaglutide—middle-aged and older adults with obesity and metabolic conditions—has a high baseline prevalence of osteoarthritis, inflammatory arthritis, and other musculoskeletal disorders. The temporal association between starting semaglutide and developing joint symptoms may be coincidental rather than causal, highlighting the importance of thorough clinical evaluation.
When patients report joint pain during semaglutide treatment, a systematic approach to management can help differentiate between medication-related effects, indirect consequences of treatment, and unrelated conditions requiring specific intervention.
Initial assessment should include a detailed history characterizing the joint symptoms: onset relative to medication initiation, location and pattern of joint involvement, severity and functional impact, aggravating and relieving factors, and any associated symptoms such as swelling, redness, or morning stiffness. Physical examination should assess for objective signs of joint inflammation, range of motion limitations, and patterns consistent with specific rheumatological or orthopedic conditions.
Conservative management strategies are appropriate for mild, non-inflammatory joint discomfort:
Optimize nutrition: Ensure adequate protein intake (0.8–1.2 g/kg body weight daily, individualized based on age and renal function), maintain hydration, and consider evaluation of vitamin D levels with supplementation if deficient (target 25-hydroxyvitamin D >30 ng/mL)
Gradual exercise progression: Implement low-impact activities such as swimming, cycling, or walking, with gradual increases in intensity to avoid overuse injuries
Weight management expectations: Counsel patients that temporary joint discomfort during rapid weight loss may improve as weight stabilizes and biomechanical adaptation occurs
Over-the-counter analgesics: Acetaminophen (up to 3,000 mg daily in divided doses) may provide symptomatic relief for mild discomfort. Use with caution in liver disease, avoid with alcohol consumption, and check combination products to prevent overdose. Topical NSAIDs are preferred over oral NSAIDs, especially in patients with kidney disease, heart failure, or those taking ACE inhibitors, ARBs, or diuretics
For patients with more significant symptoms, physical therapy evaluation can be valuable for assessing biomechanics, providing targeted strengthening exercises, and addressing any movement pattern abnormalities that may contribute to joint stress. A physical therapist can design an individualized program that accommodates the patient's current fitness level and weight loss trajectory.
Medication adjustment should be considered if joint symptoms are severe or significantly impact quality of life. This might include temporarily holding the current dose, reducing to a previously tolerated dose, or slowing the titration schedule. Importantly, patients should never adjust their semaglutide dose without consulting their healthcare provider. Discontinuation of semaglutide solely for mild joint discomfort is generally not necessary if the medication is providing significant metabolic or weight management benefits and other causes have been excluded.
While mild, transient joint discomfort during semaglutide treatment may not require urgent medical attention, certain clinical features warrant prompt evaluation to exclude serious underlying conditions or complications requiring specific treatment.
Seek emergency care immediately for:
Acute monoarticular joint pain with severe swelling, warmth, and redness, especially with fever, which may indicate septic arthritis requiring emergency treatment
Inability to bear weight on an affected joint
Signs of hypersensitivity reaction including facial/lip swelling, widespread hives, or difficulty breathing (stop semaglutide and seek urgent care)
Prompt medical evaluation is indicated for:
Joint pain accompanied by fever, chills, or systemic symptoms, suggesting possible infection or systemic inflammatory condition
Severe pain that significantly limits function or mobility, particularly if onset is sudden
Joint symptoms associated with skin rash, oral ulcers, or other systemic manifestations that might indicate autoimmune or connective tissue disease
Routine but timely evaluation (within 1–2 weeks) is appropriate for:
Persistent joint pain lasting more than 2–3 weeks without improvement
Progressive worsening of symptoms despite conservative management
Morning stiffness lasting more than 30 minutes, suggesting inflammatory arthritis
Multiple joint involvement in a symmetric pattern
Joint symptoms accompanied by unexplained weight loss beyond expected treatment effects, night sweats, or profound fatigue
During the clinical evaluation, your healthcare provider may perform laboratory investigations including complete blood count, inflammatory markers (erythrocyte sedimentation rate and C-reactive protein), rheumatoid factor, anti-cyclic citrullinated peptide antibodies, uric acid level, or other tests based on clinical presentation. Imaging studies such as plain radiographs, ultrasound, or MRI may be indicated to assess for structural joint abnormalities, inflammatory changes, or other pathology.
Patients should maintain open communication with their healthcare team throughout semaglutide treatment. Keeping a symptom diary documenting the timing, severity, and characteristics of joint symptoms can provide valuable information for clinical decision-making. The goal is to balance the significant metabolic and weight management benefits of semaglutide against any adverse effects, ensuring that treatable conditions are not missed and that patients receive comprehensive, individualized care that addresses both their metabolic health and musculoskeletal well-being.
No, joint pain is not listed among the common side effects in FDA prescribing information for semaglutide. Clinical trials showed joint pain rates similar to placebo, indicating no established direct causal relationship.
Joint discomfort may result from indirect factors such as rapid weight loss altering biomechanical loading, nutritional deficiencies from reduced caloric intake, changes in physical activity patterns, or coincidental conditions like osteoarthritis common in the patient demographic.
Seek immediate care for severe joint swelling with fever, inability to bear weight, or signs of allergic reaction. Contact your provider promptly for persistent pain lasting over 2-3 weeks, progressive worsening, morning stiffness exceeding 30 minutes, or multiple joint involvement.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.