LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Semaglutide (Ozempic, Wegovy) is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and weight management. While highly effective, this medication commonly causes gastrointestinal side effects due to its mechanism of slowing gastric emptying. Many patients wonder whether semaglutide can trigger heartburn or acid reflux. Although not listed among the most frequent adverse effects in FDA labeling, some individuals report new or worsened reflux symptoms while taking this medication. Understanding the connection between semaglutide and heartburn—and knowing how to manage these symptoms—can help you continue treatment safely and comfortably.
Quick Answer: Semaglutide can potentially cause heartburn in some patients, though it is not among the most commonly reported side effects in clinical trials.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for managing type 2 diabetes (under the brand name Ozempic) and chronic weight management (Wegovy). This medication works by mimicking the natural hormone GLP-1, which stimulates insulin secretion, suppresses glucagon release, and slows gastric emptying. While these mechanisms contribute to improved glycemic control and weight loss, they also explain why gastrointestinal side effects are among the most commonly reported adverse reactions.
According to the FDA prescribing information, the most frequent adverse effects of semaglutide include nausea, vomiting, diarrhea, abdominal pain, and constipation. The incidence of these effects varies by dose and indication—with nausea occurring in approximately 20% of patients taking Ozempic (0.5-1 mg) but up to 44% of those taking Wegovy (2.4 mg). These symptoms occur because semaglutide delays the rate at which food leaves the stomach—a process known as delayed gastric emptying—though this effect may attenuate over time with continued use. Gastrointestinal effects tend to be most pronounced when initiating therapy or increasing the dose, and many patients experience improvement as their bodies adjust to the medication.
Understanding the pharmacological basis for these digestive symptoms is essential for both patients and healthcare providers. The delayed gastric emptying that contributes to satiety and weight loss can also lead to increased gastric distension and pressure, which may trigger or worsen symptoms related to the upper gastrointestinal tract. Notably, the FDA cautions against using semaglutide in patients with severe gastroparesis or severe gastrointestinal disease. While semaglutide offers significant therapeutic benefits for diabetes management and weight reduction, recognizing and managing its gastrointestinal side effects remains an important aspect of treatment optimization.
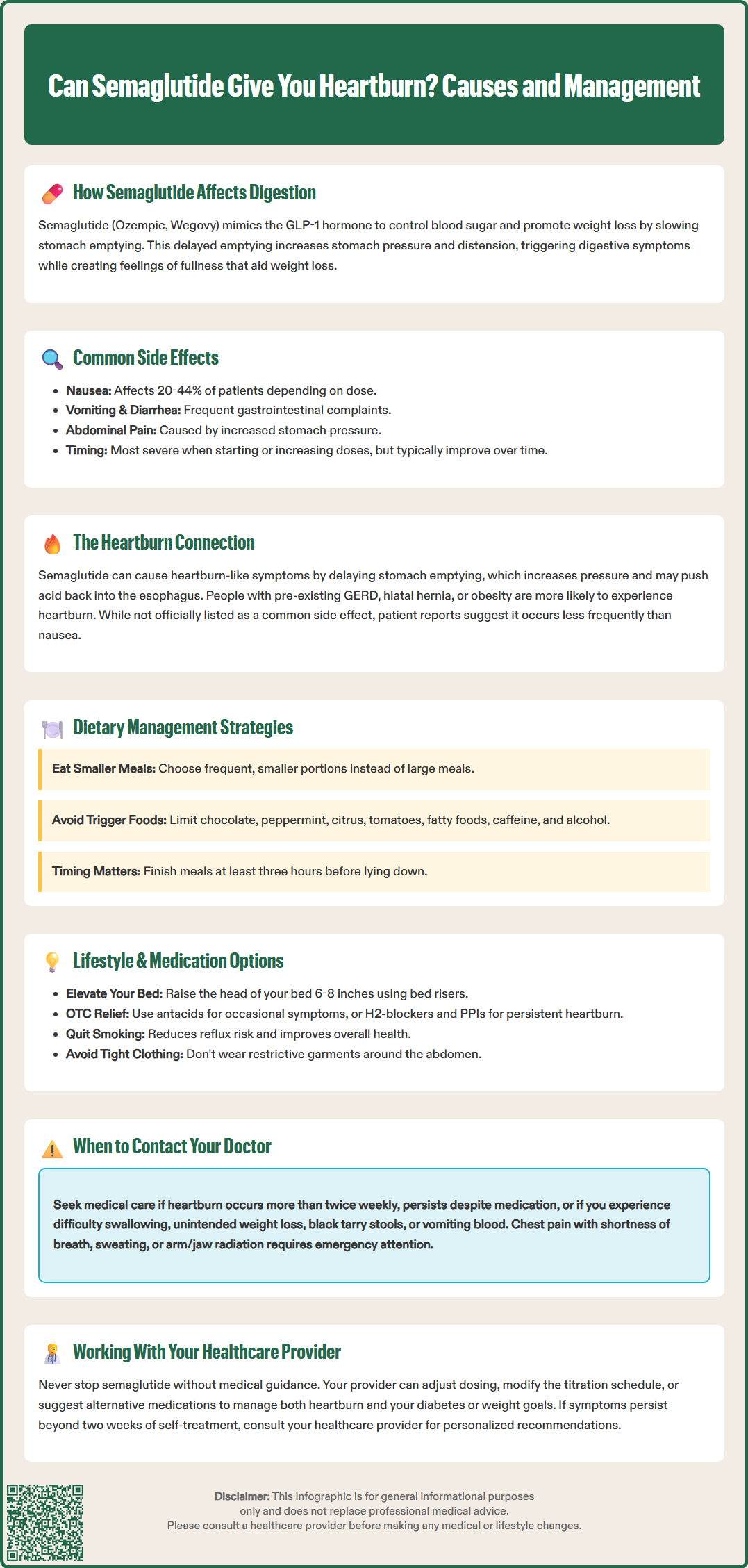
While heartburn (gastroesophageal reflux) is not specifically listed among the most common adverse effects in semaglutide's FDA labeling, related symptoms such as dyspepsia (indigestion) and eructation (belching) are documented side effects, particularly with Wegovy. These symptoms may overlap with what patients experience and report as "heartburn." Heartburn occurs when stomach acid flows backward into the esophagus, causing a burning sensation in the chest. The delayed gastric emptying induced by semaglutide can increase gastric pressure and volume, potentially promoting reflux of gastric contents into the esophagus.
Clinical trial data do not specifically highlight heartburn as a frequent adverse effect, but observational data and patient reports suggest that some individuals experience new-onset or worsened reflux symptoms while taking semaglutide. It is important to note that evidence is limited to observational data and case reports; causality has not been firmly established. The incidence appears to be relatively uncommon compared to other gastrointestinal effects like nausea. However, the physiological mechanism—prolonged gastric retention leading to increased intra-gastric pressure—provides a plausible explanation for why some patients may develop these symptoms.
Several factors may increase the likelihood of experiencing heartburn on semaglutide. Patients with pre-existing gastroesophageal reflux disease (GERD), hiatal hernia, or obesity may be more susceptible. Additionally, dietary choices, meal timing, and portion sizes can influence symptom severity. The medication's effect on gastric motility means that larger meals or foods that typically trigger reflux (such as fatty foods, caffeine, alcohol, or spicy dishes) may be more likely to cause discomfort. Healthcare providers should inquire about reflux symptoms during follow-up visits, particularly in patients with known risk factors for GERD.
If you experience heartburn while taking semaglutide, several evidence-based strategies can help manage symptoms without necessarily discontinuing the medication. Dietary modifications represent the first-line approach. Eating smaller, more frequent meals rather than large portions can reduce gastric distension and pressure. Avoiding known reflux triggers—including chocolate, peppermint, citrus fruits, tomato-based products, fatty or fried foods, caffeine, and alcohol—may significantly improve symptoms. Additionally, finishing meals at least three hours before lying down allows more time for gastric emptying.
Lifestyle adjustments can also provide substantial relief. Elevating the head of your bed by 6–8 inches (using bed risers, not just pillows) helps prevent nocturnal reflux by using gravity to keep stomach contents in place. Maintaining a healthy weight, avoiding tight-fitting clothing around the abdomen, and not lying down immediately after eating are all recommended measures. If you smoke, cessation is strongly advised, as tobacco use weakens the lower esophageal sphincter and worsens reflux.
Pharmacological management may be appropriate for persistent symptoms. Over-the-counter antacids (such as calcium carbonate or magnesium hydroxide) can provide rapid but temporary relief for occasional heartburn. H2-receptor antagonists (like famotidine) or proton pump inhibitors (PPIs such as omeprazole or esomeprazole) offer more sustained acid suppression for frequent or severe symptoms. For typical GERD symptoms, an 8-week trial of once-daily PPI therapy is standard, followed by using the lowest effective dose for maintenance if needed. If you require over-the-counter remedies for more than two weeks without improvement, consult your healthcare provider.
It is essential to discuss any new or worsening heartburn with your healthcare team before starting self-treatment. Your provider may adjust your semaglutide dose, modify the titration schedule, or recommend specific investigations to rule out other causes of your symptoms. In some cases, temporary dose reduction or slower titration may allow your body to adapt while minimizing gastrointestinal side effects.
While mild, occasional heartburn may be manageable with lifestyle modifications and over-the-counter remedies, certain symptoms warrant prompt medical evaluation. Contact your healthcare provider if you experience:
Heartburn occurring more than twice weekly despite self-care measures
Persistent symptoms despite an adequate trial of proton pump inhibitors
Difficulty swallowing (dysphagia) or pain with swallowing (odynophagia)
Persistent nausea or vomiting, particularly if you cannot keep down food or fluids
Unintended weight loss beyond expected therapeutic effects
Symptoms of gastrointestinal bleeding, including black, tarry stools or vomiting blood or material resembling coffee grounds
Severe or persistent abdominal pain, especially if radiating to the back (which may indicate pancreatitis)
Right upper quadrant pain, fever, or yellowing of the skin/eyes (possible gallbladder disease)
Signs of dehydration (extreme thirst, dry mouth, decreased urination) with protracted vomiting
Chest pain, especially if accompanied by shortness of breath, sweating, or radiation to the arm or jaw
These warning signs may indicate complications such as esophagitis, gastric ulceration, or other serious conditions requiring investigation. It is crucial to distinguish cardiac chest pain from gastrointestinal symptoms—if you experience chest discomfort with concerning features, seek emergency medical attention immediately.
Your healthcare provider may recommend diagnostic evaluation, including upper endoscopy (esophagogastroduodenoscopy) if you have alarm symptoms, refractory GERD despite optimized therapy, or risk factors for Barrett's esophagus (such as chronic GERD plus male sex, age over 50, White race, central obesity, tobacco history, or family history). If heartburn significantly impacts your quality of life or adherence to semaglutide therapy, your provider can discuss alternative GLP-1 receptor agonists, dose adjustments, or complementary treatments to optimize both diabetes or weight management and gastrointestinal comfort. Never discontinue semaglutide without medical guidance, as abrupt cessation may affect glycemic control or weight management goals.
Heartburn is not among the most frequently reported side effects in clinical trials, though related symptoms like dyspepsia occur in some patients. The incidence appears relatively uncommon compared to nausea or vomiting, but observational data suggest some individuals experience new or worsened reflux symptoms.
Semaglutide slows gastric emptying, which can increase stomach pressure and volume, potentially promoting reflux of gastric contents into the esophagus. This mechanism provides a plausible explanation for heartburn symptoms in susceptible individuals.
Do not discontinue semaglutide without consulting your healthcare provider, as stopping may affect your diabetes control or weight management goals. Most cases of heartburn can be managed with dietary modifications, lifestyle changes, or acid-suppressing medications while continuing treatment.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.