LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Can semaglutide cause liver damage? This question concerns many patients prescribed Ozempic, Wegovy, or Rybelsus for type 2 diabetes or weight management. Current evidence does not establish semaglutide as a cause of clinically significant liver injury in most patients. In fact, research suggests this GLP-1 receptor agonist may improve liver health markers in individuals with fatty liver disease through weight loss effects. While the FDA prescribing information does not list hepatotoxicity as a recognized adverse effect, understanding the medication's safety profile—including rare case reports and labeled risks like gallbladder disease—helps patients and providers make informed treatment decisions.
Quick Answer: Semaglutide does not cause clinically significant liver damage in most patients and may improve liver health markers through weight loss effects.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus and chronic weight management. Available under brand names including Ozempic, Wegovy, and Rybelsus, this medication mimics the action of naturally occurring GLP-1, a hormone released by the intestines in response to food intake.
The mechanism of action involves binding to GLP-1 receptors located throughout the body, including the pancreas, brain, and gastrointestinal tract. By activating these receptors, semaglutide enhances glucose-dependent insulin secretion from pancreatic beta cells, suppresses inappropriate glucagon release, and slows gastric emptying. These combined effects help lower blood glucose levels in people with type 2 diabetes. Additionally, semaglutide acts on appetite-regulating centers in the hypothalamus, promoting satiety and reducing caloric intake, which contributes to weight loss.
Semaglutide is administered either as a once-weekly subcutaneous injection (Ozempic, Wegovy) or as a daily oral tablet (Rybelsus). The medication has demonstrated significant efficacy in clinical trials, with patients achieving meaningful reductions in hemoglobin A1c levels and body weight. According to the American Diabetes Association guidelines, GLP-1 receptor agonists like semaglutide with proven cardiovascular benefit are recommended for patients with type 2 diabetes who have established atherosclerotic cardiovascular disease and for appropriate candidates requiring weight management.
It's important to note that semaglutide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or in patients with Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
Understanding how semaglutide works provides important context when evaluating its safety profile, including potential effects on organ systems such as the liver. The medication's widespread use has prompted careful monitoring of adverse effects across diverse patient populations.
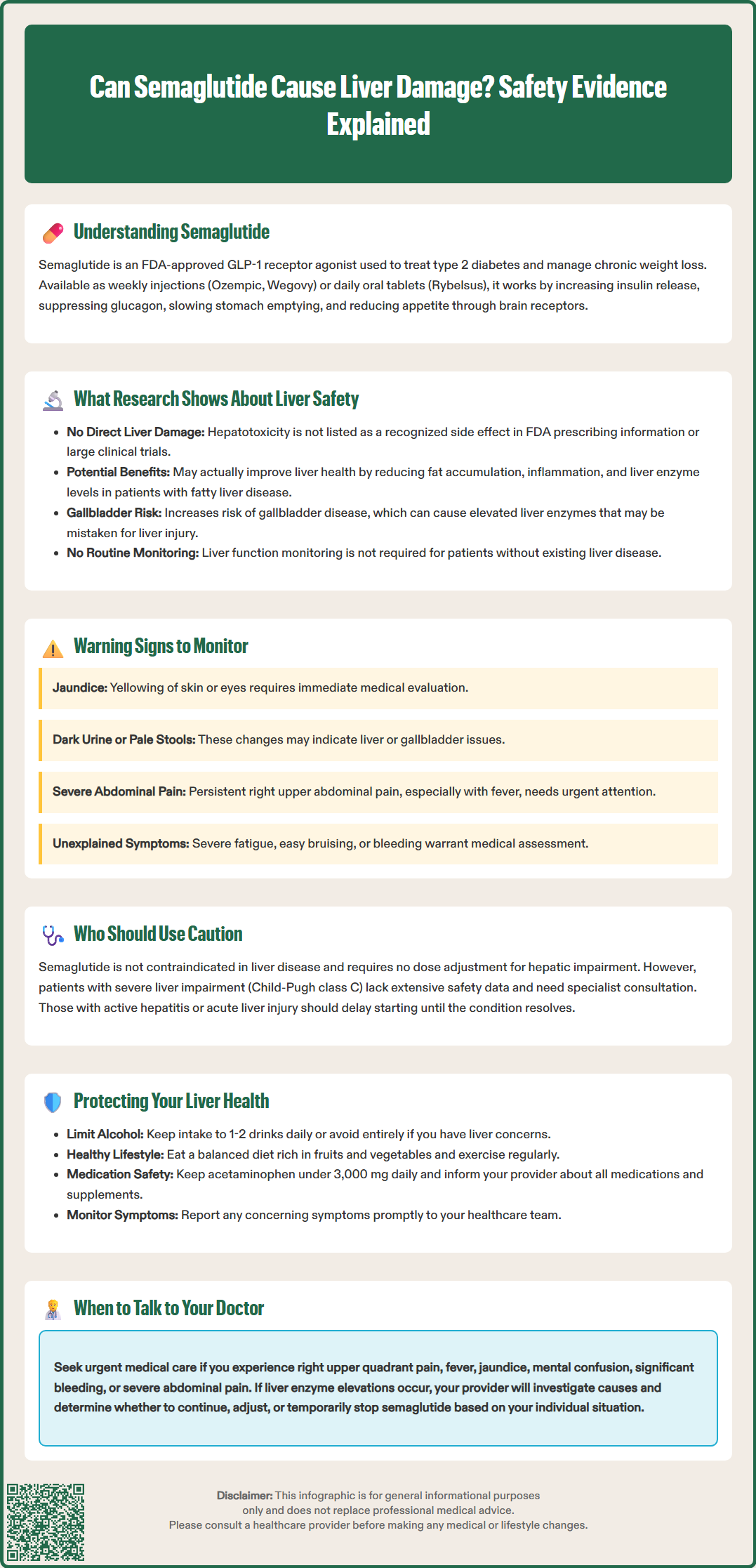
Current evidence does not establish a direct causal link between semaglutide and clinically significant liver damage in most patients. The FDA-approved prescribing information for semaglutide does not list hepatotoxicity as a recognized adverse effect, and large-scale clinical trials have not demonstrated an increased risk of liver injury compared to placebo or other diabetes medications.
Interestingly, research suggests that semaglutide may benefit liver health in certain contexts, primarily through weight loss effects. Multiple studies have shown improvements in markers of metabolic dysfunction-associated steatotic liver disease (MASLD, formerly NAFLD) and metabolic dysfunction-associated steatohepatitis (MASH, formerly NASH) among patients treated with GLP-1 receptor agonists. Weight loss induced by semaglutide can reduce hepatic steatosis (fat accumulation in the liver), decrease liver inflammation, and improve liver enzyme levels in individuals with obesity-related liver disease. Clinical trials, including the STEP program and a 2021 New England Journal of Medicine study on MASH, have documented reductions in alanine aminotransferase (ALT) and aspartate aminotransferase (AST) levels. However, it's important to note that semaglutide is not FDA-approved for the treatment of MASH.
It is essential to distinguish between direct hepatotoxicity and other labeled risks that may affect liver function tests. The FDA prescribing information for GLP-1 receptor agonists, including semaglutide, notes an increased risk of acute gallbladder disease (cholelithiasis, cholecystitis), which can present with jaundice and elevated liver enzymes that might be mistaken for direct liver injury.
Isolated case reports have described elevations in liver enzymes or rare instances of liver-related adverse events in patients taking semaglutide. These reports are uncommon and often involve patients with pre-existing liver conditions, concurrent medications, or other confounding factors. It remains unclear whether semaglutide directly caused these events or whether they resulted from underlying disease progression or other variables.
Routine liver function monitoring is not required for patients without pre-existing liver disease, though baseline assessment may be appropriate in certain clinical situations. Overall, the available evidence suggests that semaglutide poses minimal risk to liver health in the general population and may offer benefits for patients with fatty liver disease through its weight loss effects.
While serious liver damage from semaglutide is not a commonly recognized adverse effect, patients and healthcare providers should remain vigilant for signs and symptoms that could indicate hepatic dysfunction. Awareness of potential warning signs enables early detection and appropriate medical evaluation if concerns arise.
Key symptoms that warrant medical attention include:
Jaundice: Yellowing of the skin or whites of the eyes, indicating elevated bilirubin levels
Dark urine: Brown or tea-colored urine that persists beyond initial hydration status
Pale or clay-colored stools: Suggesting impaired bile flow
Persistent abdominal pain: Particularly in the right upper quadrant where the liver is located
Unexplained fatigue: Severe tiredness that interferes with daily activities
Nausea and vomiting: Especially when persistent and unexplained by other causes
Loss of appetite: Significant decrease in food intake beyond expected effects of the medication
Easy bruising or bleeding: Potentially indicating impaired liver synthetic function
Emergency warning signs requiring immediate medical care include mental status changes or confusion, significant bleeding, and severe abdominal pain with fever.
It is important to distinguish between common gastrointestinal side effects of semaglutide—such as nausea, vomiting, and decreased appetite—and symptoms specifically suggestive of liver dysfunction. The former are expected pharmacological effects related to delayed gastric emptying and typically improve with continued use or dose adjustment. Liver-specific symptoms, particularly jaundice or dark urine, require prompt medical evaluation.
Patients should also be aware that GLP-1 receptor agonists like semaglutide carry a labeled risk of acute gallbladder disease (cholelithiasis, cholecystitis), which can present with right upper quadrant pain, fever, and jaundice. These symptoms may overlap with those of liver dysfunction and warrant prompt evaluation, potentially including imaging studies.
Similarly, pancreatitis—another labeled risk with semaglutide—can present with persistent severe abdominal pain that may radiate to the back, with or without vomiting, and requires immediate medical attention.
Patients with pre-existing liver conditions should discuss appropriate monitoring strategies with their healthcare provider. While routine liver function testing is not standard for all patients on semaglutide, those with known hepatic disease may benefit from periodic assessment of ALT, AST, alkaline phosphatase, and bilirubin levels. Any significant elevation in these markers should prompt clinical correlation and consideration of alternative causes, including medication effects, disease progression, or new hepatic pathology.
Semaglutide is not contraindicated in patients with liver disease, and the FDA prescribing information does not list hepatic impairment as an absolute contraindication to its use. In fact, FDA labeling indicates that no dose adjustment is needed for patients with hepatic impairment. However, certain patient populations require careful consideration and individualized risk-benefit assessment before initiating therapy.
Patients with severe hepatic impairment (Child-Pugh class C) have not been extensively studied in clinical trials, and limited data exist regarding the safety and efficacy of semaglutide in this population. While semaglutide is a peptide that undergoes proteolytic degradation rather than hepatic metabolism, the overall physiological stress of advanced liver disease may influence treatment tolerability. Consultation with a hepatologist or endocrinologist experienced in managing complex cases is advisable before prescribing semaglutide to patients with decompensated cirrhosis.
Individuals with active hepatitis or acute liver injury from any cause should generally defer initiation of new medications, including semaglutide, until the acute process has resolved and liver function has stabilized. This precautionary approach, while not a labeled restriction, represents good clinical practice. It minimizes the risk of attributing disease-related changes to medication effects and allows for clearer assessment of treatment safety once the patient's condition improves.
Patients with alcohol-related liver disease who continue active alcohol consumption require special consideration. While semaglutide itself does not appear to cause liver damage, ongoing alcohol use can complicate the clinical picture and increase the risk of hepatotoxicity from multiple sources. Addressing alcohol use disorder should be prioritized as part of comprehensive care.
Conversely, patients with metabolic dysfunction-associated steatotic liver disease (MASLD) or metabolic dysfunction-associated steatohepatitis (MASH) may actually benefit from semaglutide therapy. The medication's weight loss effects can improve hepatic steatosis and inflammation, making it a potentially valuable treatment option for this population. The American Association for the Study of Liver Diseases recognizes weight loss as a cornerstone of MASLD management, and GLP-1 receptor agonists represent an effective pharmacological approach to achieving this goal. However, it's important to note that semaglutide is not FDA-approved specifically for the treatment of MASH, and benefits are largely mediated through weight loss.
Patients taking semaglutide can take proactive steps to support liver health and minimize potential risks, even though the medication itself is not associated with significant hepatotoxicity. A comprehensive approach to hepatic wellness involves lifestyle modifications, medication management, and appropriate medical monitoring.
Lifestyle strategies that support liver health include:
Limiting alcohol consumption: Excessive alcohol intake is a leading cause of liver disease. Patients should adhere to recommended limits (no more than one drink per day for women, two for men) or abstain entirely if they have existing liver concerns.
Maintaining a balanced diet: A diet rich in fruits, vegetables, whole grains, and lean proteins supports metabolic health and reduces hepatic fat accumulation.
Regular physical activity: Exercise enhances insulin sensitivity, promotes weight loss, and improves liver enzyme levels in patients with fatty liver disease.
Avoiding hepatotoxic substances: This includes limiting acetaminophen to recommended doses (generally no more than 3,000 mg daily for adults; lower limits may apply for those with chronic alcohol use or liver disease—consult your healthcare provider for personalized guidance).
Medication management is equally important. Patients should inform their healthcare provider about all medications, supplements, and over-the-counter products they use, as drug interactions or cumulative effects may impact liver function. Some medications can affect liver enzymes, and awareness of these potential interactions allows for appropriate monitoring. For example, while statins were once thought to require routine liver monitoring, current guidance indicates that after baseline testing, routine monitoring is not required unless clinically indicated.
Medical monitoring should be individualized based on risk factors. While routine liver function testing is not required for all patients on semaglutide, those with pre-existing liver disease, obesity, diabetes, or other metabolic conditions may benefit from periodic assessment. Baseline liver function tests before starting semaglutide can provide a reference point for future comparison.
Patients should remain aware of the FDA-labeled risk of acute gallbladder disease with GLP-1 receptor agonists like semaglutide. Right upper quadrant pain, fever, or jaundice should prompt urgent medical evaluation, potentially including imaging studies.
Patients should maintain open communication with their healthcare team and report any concerning symptoms promptly. If liver enzyme elevations are detected, the provider will evaluate potential causes, which may include medication effects, disease progression, dietary factors, or new hepatic pathology. If drug-induced liver injury is suspected, semaglutide should be held pending evaluation. In most cases with mild, isolated enzyme elevations, semaglutide can be safely continued with appropriate monitoring, though individual circumstances may warrant dose adjustment or discontinuation based on clinical judgment. The overall evidence suggests that semaglutide is a safe medication for most patients when used appropriately under medical supervision.
Routine liver function monitoring is not required for patients without pre-existing liver disease taking semaglutide. However, baseline assessment and periodic monitoring may be appropriate for patients with known hepatic conditions or metabolic risk factors.
Yes, patients with metabolic dysfunction-associated steatotic liver disease may actually benefit from semaglutide therapy. Clinical trials have shown improvements in hepatic steatosis, liver inflammation, and liver enzyme levels through the medication's weight loss effects.
Seek immediate medical care for jaundice (yellowing of skin or eyes), dark urine, pale stools, persistent right upper quadrant abdominal pain, severe fatigue, or mental status changes. These symptoms may indicate liver dysfunction or gallbladder disease and require prompt evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.