LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
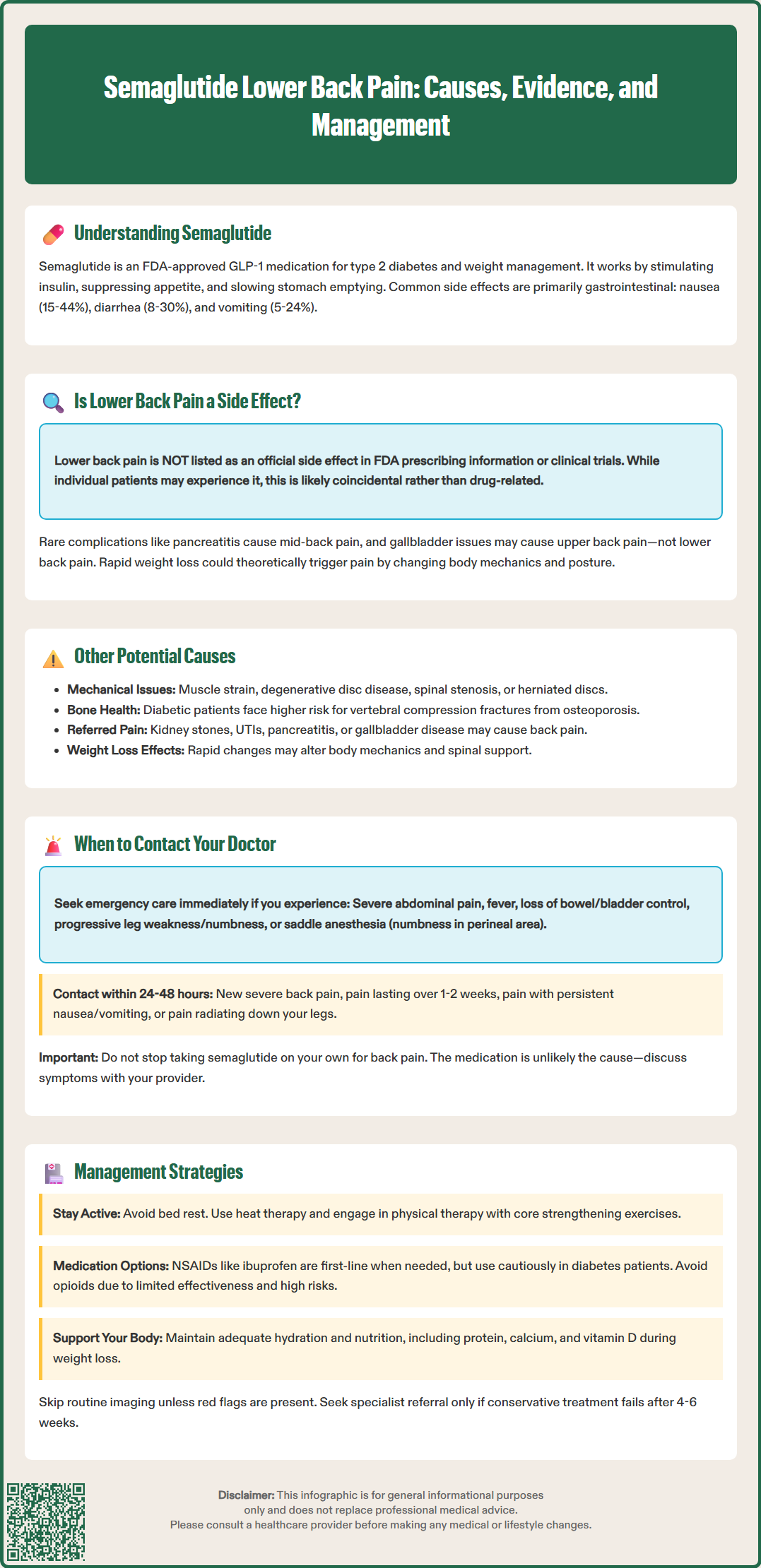
Semaglutide, marketed as Ozempic, Wegovy, and Rybelsus, is an FDA-approved GLP-1 receptor agonist used for type 2 diabetes and chronic weight management. While gastrointestinal side effects like nausea and diarrhea are well-documented, patients occasionally report musculoskeletal symptoms including lower back pain. Understanding whether semaglutide causes lower back pain requires examining clinical evidence, potential mechanisms, and alternative explanations. This article reviews the relationship between semaglutide and lower back pain, helping patients and clinicians distinguish medication-related effects from other common causes requiring appropriate evaluation and management.
Quick Answer: Lower back pain is not an established side effect of semaglutide according to FDA prescribing information and clinical trial data.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the action of endogenous GLP-1, a hormone that stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and promotes satiety through central nervous system pathways.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature, reflecting its mechanism of delayed gastric emptying. According to FDA prescribing information, these include:
Nausea (occurring in 15–44% of patients depending on formulation and dose)
Vomiting (5–24% of patients)
Diarrhea (8–30% of patients)
Abdominal pain (5–11% of patients)
Constipation (3–24% of patients)
These gastrointestinal symptoms typically emerge during dose escalation and often diminish over time as physiological tolerance develops. Other documented adverse effects include injection site reactions, fatigue, dizziness, and headache.
Serious but rare risks include pancreatitis, gallbladder disease, and acute kidney injury (particularly in patients with renal impairment or those experiencing severe gastrointestinal adverse reactions causing dehydration). Diabetic retinopathy complications may occur in patients with pre-existing disease. Semaglutide carries a boxed warning for risk of thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), and is contraindicated in patients with a personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Semaglutide should not be used during pregnancy.
The delayed gastric emptying effect may also affect the absorption of concomitant oral medications, which is particularly important for drugs with narrow therapeutic indices.
Understanding the established adverse effect profile of semaglutide provides essential context when evaluating new or unexpected symptoms during treatment, including musculoskeletal complaints such as lower back pain.
Lower back pain is not listed as a common or characteristic adverse effect in the FDA-approved prescribing information for semaglutide formulations (Ozempic, Wegovy, or Rybelsus). Clinical trials conducted during the drug's development and post-marketing surveillance data have not established a direct causal relationship between semaglutide administration and musculoskeletal pain in the lumbar region.
However, the absence of an officially recognized association does not definitively exclude the possibility of lower back pain occurring in individual patients taking semaglutide. FDA Adverse Event Reporting System (FAERS) data may include reports of musculoskeletal symptoms in patients using GLP-1 receptor agonists, though these reports do not establish causation and may reflect coincidental timing rather than a true drug effect.
Several potential mechanisms could theoretically link semaglutide to back pain, though these remain speculative and lack substantial clinical evidence:
Pancreatitis: Acute pancreatitis, a recognized rare complication of GLP-1 agonists, typically presents with epigastric pain radiating to the mid-back rather than the lower lumbar region.
Gallbladder disease: Cholelithiasis and cholecystitis, which are associated with GLP-1 receptor agonists, can cause right upper quadrant pain sometimes radiating to the back.
Musculoskeletal strain: Rapid weight loss associated with semaglutide may alter body mechanics, posture, and center of gravity, potentially contributing to mechanical lower back pain.
Patients experiencing new-onset lower back pain while taking semaglutide should not automatically attribute the symptom to their medication, as alternative explanations are often more likely and require appropriate clinical evaluation.
When lower back pain develops in a patient taking semaglutide, clinicians should conduct a systematic evaluation for alternative etiologies, as most cases will have causes unrelated to the medication itself. The differential diagnosis for lower back pain is extensive and includes mechanical, inflammatory, infectious, neoplastic, and referred pain sources.
Mechanical and degenerative causes represent the most common etiologies in adults and include:
Lumbar strain or sprain from physical activity, poor posture, or occupational factors
Degenerative disc disease and facet joint arthropathy
Spinal stenosis, particularly in older adults
Herniated nucleus pulposus with or without radiculopathy
Spondylolisthesis or other structural abnormalities
Metabolic and systemic conditions that may coincide with diabetes treatment include:
Diabetic radiculoplexus neuropathy (diabetic amyotrophy), which typically presents with severe unilateral thigh/hip pain and weakness rather than primary lower back pain
Osteoporosis with vertebral compression fractures, particularly relevant in patients with long-standing diabetes or corticosteroid exposure
Infectious causes requiring urgent evaluation include:
Spinal epidural abscess
Vertebral osteomyelitis/discitis, especially in patients with diabetes, immunosuppression, or intravenous drug use
Visceral referred pain should be considered, especially given semaglutide's gastrointestinal effects:
Nephrolithiasis (kidney stones)
Pyelonephritis or other urinary tract pathology
Pancreatitis (though typically mid-back pain)
Cholecystitis or biliary colic
Weight loss-related factors specific to patients on semaglutide may include altered biomechanics, increased physical activity without proper conditioning, or changes in body composition affecting spinal support structures. A thorough history, physical examination, and targeted investigations based on clinical presentation are essential to identify the underlying cause.
Patients taking semaglutide who develop lower back pain should be educated about warning signs that warrant prompt medical evaluation. While most lower back pain is benign and self-limiting, certain clinical features suggest serious underlying pathology requiring urgent assessment.
Seek immediate medical attention (emergency department or urgent care) if back pain is accompanied by:
Severe abdominal pain, particularly if radiating from the epigastrium to the back (possible pancreatitis)
Fever, chills, or signs of systemic infection
Bowel or bladder dysfunction, including new urinary retention or fecal incontinence (cauda equina syndrome)
Progressive lower extremity weakness or numbness
Saddle anesthesia (numbness in the perineal region)
Severe pain following trauma or in patients with known osteoporosis
Unintentional weight loss not explained by your treatment plan or >5% of body weight over 6–12 months, night sweats, or constitutional symptoms
History of cancer, immunosuppression, or intravenous drug use
Contact your healthcare provider within 24–48 hours for:
New-onset back pain that is severe or significantly impacts daily function
Pain persisting beyond 1–2 weeks despite conservative management
Pain associated with persistent nausea, vomiting, or changes in bowel habits
Radicular symptoms (pain, numbness, or tingling radiating down one or both legs)
Pain that worsens progressively rather than improving
Routine imaging is not recommended for nonspecific low back pain in the absence of red flags. Your healthcare provider will determine if imaging is necessary based on your specific symptoms and risk factors.
Patients should not discontinue semaglutide without medical guidance, as the back pain is unlikely to be medication-related in most cases. However, discussing all new symptoms with a healthcare provider ensures appropriate evaluation and management while maintaining diabetes or weight management treatment continuity.
Management of lower back pain in patients taking semaglutide should follow evidence-based guidelines for acute and chronic lower back pain, with consideration of the patient's overall metabolic health and treatment goals. The approach should be individualized based on pain severity, functional impairment, and underlying etiology once serious pathology has been excluded.
Nonpharmacologic management (first-line approach):
Continued activity: Patients should remain as active as tolerated, avoiding prolonged bed rest which can worsen outcomes. Gradual return to normal activities is encouraged.
Superficial heat: Local application of heat provides effective symptomatic relief for acute and subacute low back pain.
Physical therapy: Structured exercise programs focusing on core strengthening, flexibility, and posture can address mechanical causes and prevent recurrence.
Spinal manipulation: May provide modest benefit for some patients with acute low back pain.
Mind-body approaches: Tai chi, yoga, mindfulness-based stress reduction, and cognitive behavioral therapy can be beneficial, particularly for chronic low back pain.
Ergonomic assessment: Workplace and home modifications may reduce mechanical stress on the lumbar spine.
Pharmacological management requires careful consideration in patients with diabetes:
NSAIDs (such as ibuprofen or naproxen) are first-line when medication is needed and not contraindicated. Use cautiously in patients with diabetes due to potential renal, cardiovascular, and gastrointestinal risks, particularly if dehydration from semaglutide's gastrointestinal effects is present. Clinician supervision is recommended.
Acetaminophen has limited evidence of benefit for low back pain but may be considered when NSAIDs are contraindicated. Maximum daily dose should not exceed 3,000 mg, with caution in patients with liver disease or alcohol use.
Skeletal muscle relaxants may be considered for short-term use in acute low back pain.
Topical analgesics have limited evidence for low back pain but may be options for some patients.
Duloxetine may be beneficial for chronic low back pain.
Opioid analgesics should be avoided for non-specific lower back pain given limited efficacy and significant risks.
Addressing semaglutide-related factors:
Ensure adequate hydration to prevent dehydration-related complications
Optimize glycemic control, as improved diabetes management may reduce neuropathic contributions
Consider physical therapy or exercise programs tailored to patients experiencing rapid weight loss
Monitor for proper nutrition including adequate protein, calcium, and vitamin D intake
Routine imaging is not recommended for nonspecific low back pain without red flags. If conservative measures fail after 4–6 weeks, or if specific pathology is identified, referral to appropriate specialists (physiatry, orthopedics, neurosurgery, pain management, or rheumatology) may be warranted. The decision to continue, adjust, or discontinue semaglutide should be based on the overall risk-benefit assessment and whether a plausible connection between the medication and back pain can be established through clinical evaluation.
No, lower back pain is not listed as a common or recognized side effect in FDA prescribing information for semaglutide (Ozempic, Wegovy, Rybelsus). The most common adverse effects are gastrointestinal, including nausea, vomiting, and diarrhea.
Most back pain during semaglutide treatment results from mechanical causes like lumbar strain, degenerative disc disease, or altered biomechanics from weight loss. Other causes include kidney stones, infections, or referred pain from gastrointestinal conditions.
Seek immediate medical attention for back pain with fever, bowel or bladder dysfunction, progressive leg weakness, severe abdominal pain, or saddle anesthesia. Contact your provider within 24-48 hours for severe new-onset pain or symptoms persisting beyond 1-2 weeks.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.