LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Can semaglutide cause skin sensitivity? While semaglutide—a GLP-1 receptor agonist approved by the FDA for type 2 diabetes and chronic weight management—is primarily associated with gastrointestinal side effects, some patients report skin-related symptoms during treatment. Understanding the relationship between semaglutide and dermatological reactions is important for safe medication use. This article examines the evidence for skin sensitivity with semaglutide, how to recognize concerning symptoms, and when to seek medical attention. Whether you're taking Ozempic, Wegovy, or Rybelsus, knowing what skin changes warrant evaluation helps ensure optimal treatment outcomes.
Quick Answer: Semaglutide can cause localized injection site reactions in approximately 1.4–2.4% of patients, and rare serious hypersensitivity reactions including rash and angioedema have been reported, though widespread skin sensitivity is not a common side effect.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for the treatment of type 2 diabetes mellitus (under the brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the action of the naturally occurring hormone GLP-1, which stimulates insulin secretion in a glucose-dependent manner, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways.
The most commonly reported adverse effects of semaglutide are gastrointestinal in nature. According to FDA prescribing information, nausea occurs in approximately 20% of patients taking Ozempic for diabetes and up to 44% of those using Wegovy for weight management. Other common gastrointestinal effects include vomiting, diarrhea, abdominal pain, and constipation. These symptoms typically emerge during dose escalation and often diminish over time as the body adjusts to the medication.
Other recognized side effects include injection site reactions (for subcutaneous formulations like Ozempic and Wegovy), fatigue, dizziness, and headache. Serious but less common adverse effects include pancreatitis, gallbladder disease, acute kidney injury, and hypoglycemia (primarily when used with insulin or sulfonylureas). Diabetic retinopathy complications may occur in patients with a history of retinopathy. The FDA label includes a boxed warning regarding thyroid C-cell tumors observed in rodent studies, with contraindications for patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Semaglutide is also contraindicated in patients with a prior serious hypersensitivity reaction to the medication or its components.
While skin sensitivity is not listed among the most common adverse effects of semaglutide, dermatological reactions have been reported in clinical practice and post-marketing surveillance. According to FDA prescribing information, injection site reactions occur in approximately 1.4% of patients receiving Ozempic and 2.4% of those receiving Wegovy. These localized reactions may include erythema, pruritus, swelling, and discomfort at the injection site. It's important to note that Rybelsus, being an oral formulation, does not cause injection site reactions.
There is no established direct pharmacological mechanism by which semaglutide would cause widespread skin sensitivity. However, the FDA labels for all semaglutide products note that serious hypersensitivity reactions, including anaphylaxis and angioedema, have been reported in patients treated with semaglutide. These reactions, while rare, require immediate medical attention and discontinuation of the medication.
Case reports and post-marketing data have documented various cutaneous reactions in patients taking GLP-1 receptor agonists, including urticaria, rash, and pruritus. A 2022 review in the Journal of Clinical and Aesthetic Dermatology noted that dermatological adverse events, while relatively uncommon, represent an important consideration in GLP-1 agonist therapy. It remains unclear whether these reactions result from direct drug effects or immune-mediated responses.
Some patients experiencing significant weight loss may notice changes in skin texture or elasticity, but these are generally related to the weight loss itself rather than a direct medication effect. Patients experiencing new or worsening skin symptoms should report these to their healthcare provider for appropriate evaluation, as distinguishing between benign reactions and potentially serious hypersensitivity is essential for safe continuation of therapy.
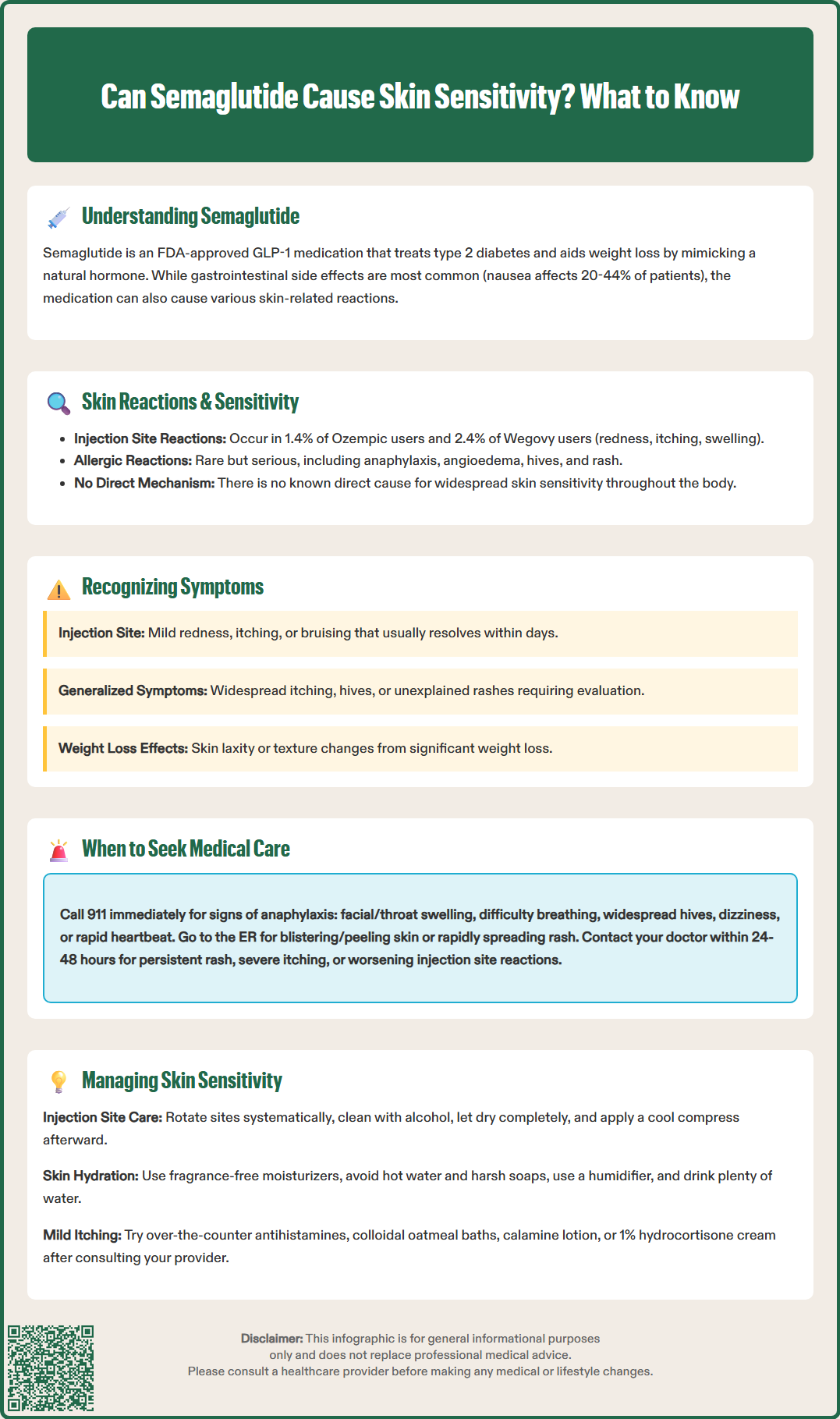
Patients taking semaglutide should be aware of various skin-related symptoms that may develop during treatment. Injection site reactions are the most commonly reported dermatological effects with subcutaneous semaglutide (Ozempic and Wegovy) and typically present as redness, itching, bruising, or mild swelling at the site of administration. These reactions are generally mild, self-limiting, and resolve within a few days without intervention. Rotating injection sites as recommended can help minimize these localized effects. Note that oral semaglutide (Rybelsus) does not cause injection site reactions.
Signs of injection site infection, such as expanding redness, warmth, purulence, or fever, require prompt medical evaluation as these may indicate a complication requiring antibiotic treatment.
Generalized skin symptoms that may warrant attention include widespread itching (pruritus) without visible rash, development of hives (urticaria), or unexplained rashes. While some patients report increased skin dryness or sensitivity to touch, temperature, or topical products during treatment, these symptoms are not definitively linked to semaglutide and may have other causes that should be evaluated by a healthcare provider.
Signs of potential allergic or hypersensitivity reactions require urgent evaluation. These include rapidly developing rash, facial swelling, swelling of the lips or tongue, difficulty breathing, or widespread hives appearing shortly after administration. Such symptoms may indicate angioedema or anaphylaxis, which are rare but serious complications requiring immediate medical attention.
Patients experiencing significant weight loss may notice skin changes including increased laxity or altered texture. Keeping a symptom diary noting the timing, location, and characteristics of any skin changes can provide valuable information for healthcare providers in determining the cause and appropriate management approach.
Determining when skin changes require medical evaluation is important for patient safety and optimal treatment outcomes. Seek emergency medical care immediately (call 911 in the US) if you experience signs of a serious allergic reaction, including facial swelling, swelling of the tongue or throat, difficulty breathing or swallowing, rapid onset of widespread hives, dizziness, or rapid heartbeat. These symptoms may indicate anaphylaxis, a medical emergency requiring prompt treatment with epinephrine.
Seek urgent medical attention (same day or emergency room) for blistering or peeling skin, mucosal involvement (mouth, eyes, genitals), or rapidly progressing rash. These symptoms could indicate severe cutaneous adverse reactions that require immediate evaluation and treatment.
Contact your healthcare provider within 24–48 hours if you develop a persistent rash, severe itching that interferes with daily activities or sleep, painful skin lesions, or injection site reactions that worsen rather than improve over several days. Additionally, any skin changes accompanied by fever, joint pain, or systemic symptoms should prompt timely medical evaluation, as these may indicate a more complex reaction or other underlying condition.
Routine discussion at your next scheduled appointment is appropriate for mild injection site reactions that resolve within a few days, minor itching without rash that is intermittent and tolerable, or gradual skin texture changes that may be related to weight loss. However, even seemingly minor symptoms that persist or cause concern warrant earlier discussion with your healthcare team.
When contacting your provider, be prepared to describe the timing of symptom onset relative to your semaglutide doses, the location and appearance of any skin changes, associated symptoms, and any new medications, supplements, or topical products you have started. Photographs of visible skin changes can be helpful for remote consultations. Patients who experience serious hypersensitivity reactions should not be rechallenged with semaglutide. Suspected adverse reactions may be reported to the FDA MedWatch program. Never discontinue semaglutide without medical guidance, particularly if using it for diabetes management, as abrupt cessation may affect glycemic control.
For patients experiencing skin sensitivity while taking semaglutide, several management strategies can help minimize discomfort while maintaining therapeutic benefits. For injection site reactions, proper injection technique is fundamental. Follow the manufacturer's Instructions for Use exactly, including proper storage requirements. Rotate injection sites systematically (abdomen, thigh, or upper arm), and avoid injecting into areas with existing irritation, scarring, or skin changes. Clean the injection site with alcohol and allow it to dry completely before injection. Applying a cool compress after injection may reduce local inflammation and discomfort.
For generalized skin sensitivity or dryness, maintaining optimal skin hydration is essential. Use fragrance-free, hypoallergenic moisturizers regularly, particularly after bathing when skin is still slightly damp to lock in moisture. Avoid harsh soaps, hot water, and excessive bathing, which can strip natural skin oils. Consider using a humidifier in dry environments and ensure adequate hydration by drinking sufficient water throughout the day. Some patients benefit from switching to gentler laundry detergents and avoiding fabric softeners that may irritate sensitive skin.
Symptomatic relief measures for mild itching include over-the-counter non-sedating oral antihistamines such as cetirizine or loratadine. Consult with your pharmacist or healthcare provider before starting any antihistamine to review potential interactions with your other medications and medical conditions. Topical treatments like colloidal oatmeal baths, calamine lotion, or hydrocortisone cream (1% over-the-counter strength) may provide relief for localized itching or mild rashes. However, avoid applying topical corticosteroids to large body surface areas or for extended periods without medical supervision.
If skin symptoms persist despite these measures, your healthcare provider may consider adjusting your semaglutide dose, temporarily holding treatment to assess symptom resolution, or prescribing prescription-strength topical or oral medications. In cases of serious hypersensitivity reactions, semaglutide should be permanently discontinued. If alternative therapy is needed, caution should be exercised when considering other GLP-1 receptor agonists due to potential cross-reactivity. The American Diabetes Association Standards of Care emphasize individualized treatment approaches, and medication adjustments should balance glycemic control or weight management goals with tolerability and quality of life considerations.
The most common skin reactions are injection site reactions occurring in 1.4–2.4% of patients using Ozempic or Wegovy, typically presenting as mild redness, itching, bruising, or swelling that resolves within a few days. Oral semaglutide (Rybelsus) does not cause injection site reactions.
Seek emergency care immediately if you experience facial swelling, swelling of the tongue or throat, difficulty breathing or swallowing, rapid onset of widespread hives, or dizziness, as these may indicate anaphylaxis requiring urgent treatment.
Rotate injection sites systematically between the abdomen, thigh, and upper arm, clean the site with alcohol and allow it to dry completely before injection, and avoid injecting into areas with existing irritation or scarring. Applying a cool compress after injection may also help reduce local inflammation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.