LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

What foods make you sick on semaglutide? Many patients taking this GLP-1 medication experience nausea and digestive discomfort with certain foods, particularly high-fat, fried, and greasy items. Semaglutide slows gastric emptying—the rate food leaves your stomach—which increases satiety but also makes your digestive system more sensitive. Understanding which foods commonly trigger symptoms and how to adjust your diet can significantly reduce gastrointestinal side effects while maintaining adequate nutrition. This guide explains the mechanisms behind food-related reactions and provides practical strategies for eating comfortably during semaglutide treatment.
Quick Answer: High-fat foods, fried items, greasy dishes, and very sweet foods most commonly cause nausea and digestive discomfort in patients taking semaglutide due to the medication's gastric-slowing effects.
Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (under brand names Ozempic and Rybelsus) and chronic weight management (Wegovy). This medication works by mimicking the natural hormone GLP-1, which plays several important roles in metabolic regulation. Understanding how semaglutide affects your digestive system helps explain why certain foods may cause discomfort during treatment.
The primary mechanism involves slowing gastric emptying—the rate at which food moves from your stomach into your small intestine. By activating GLP-1 receptors in the gastrointestinal tract, semaglutide delays this process significantly, which contributes to increased satiety and reduced appetite. This delayed gastric emptying means food remains in your stomach longer than usual, creating a sensation of fullness that persists for extended periods. While this effect supports weight loss and glycemic control, it also makes your digestive system more sensitive to certain food types. It's worth noting that this gastric-emptying delay may diminish somewhat with continued use.
Semaglutide primarily affects the stomach, though it can also influence other aspects of digestion. Common gastrointestinal adverse effects include nausea, vomiting, diarrhea, and constipation. Clinical trials have shown that gastrointestinal side effects are among the most common, with nausea reported in 15-20% of patients taking semaglutide for diabetes and up to 44% of those on higher doses for weight management. These effects typically peak during dose escalation periods and often improve over time as your body adjusts to the medication.
Importantly, the delayed gastric emptying can affect the absorption of some oral medications. If you take other medications, especially those with a narrow therapeutic window, discuss potential timing adjustments with your healthcare provider.
Patients taking semaglutide frequently report that specific food categories consistently trigger nausea, bloating, or gastrointestinal discomfort. While individual tolerance varies, certain patterns emerge from clinical experience and patient reports. Recognizing these commonly reported triggers allows you to make informed dietary adjustments that may reduce adverse effects while maintaining adequate nutrition.
High-fat foods top the list of problematic items. Foods such as bacon, sausage, full-fat dairy products, butter-heavy dishes, and cream-based sauces tend to cause significant discomfort. Because fats naturally slow gastric emptying even in individuals not taking semaglutide, the combined effect with the medication can lead to prolonged feelings of uncomfortable fullness, nausea, and sometimes vomiting.
Fried and greasy foods similarly cause problems due to their high fat content and the way they're prepared. French fries, fried chicken, doughnuts, and other deep-fried items frequently trigger symptoms. The combination of high fat content and often high caloric density makes these foods particularly challenging for the slowed digestive system.
Spicy foods may exacerbate nausea in some patients, especially those already experiencing gastrointestinal sensitivity from semaglutide. Hot peppers, heavily spiced curries, and dishes with significant amounts of chili or hot sauce can irritate an already sensitive stomach lining.
Very sweet or sugary foods including candy, pastries, sweetened beverages, and desserts may trigger nausea or discomfort in some individuals. Additionally, many patients report that carbonated beverages can cause bloating and increased feelings of fullness that become uncomfortable when gastric emptying is already delayed by semaglutide. Remember that food tolerances are highly individual, and keeping a food diary can help identify your personal triggers.
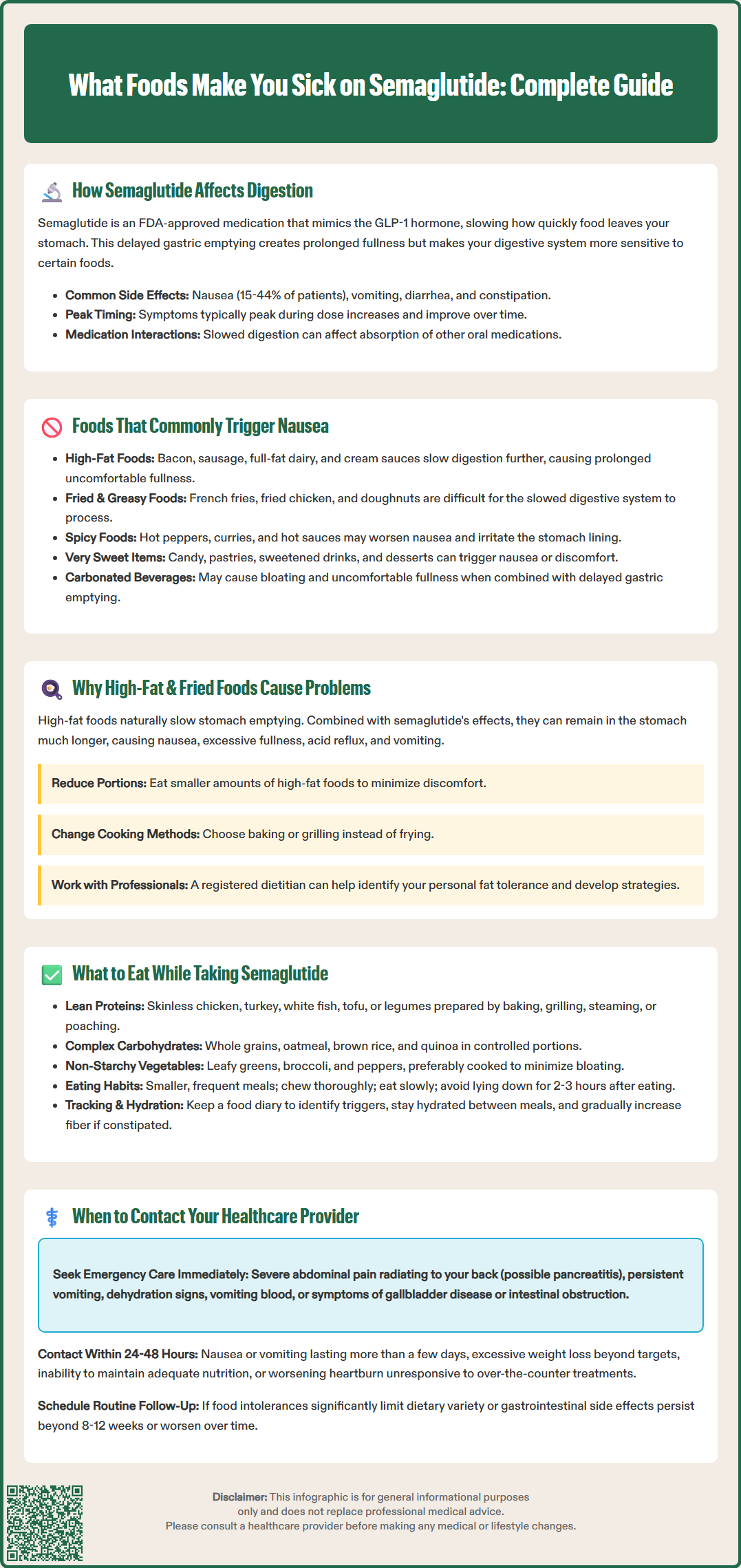
The relationship between high-fat foods and semaglutide-related gastrointestinal symptoms deserves particular attention due to the frequency and severity of reactions patients experience. Understanding the physiological basis for this interaction helps explain why dietary fat modification often becomes necessary during semaglutide treatment.
Fat is the macronutrient that naturally takes the longest to digest and empty from the stomach. Under normal circumstances, fatty foods trigger the release of cholecystokinin (CCK) and other hormones that slow gastric emptying to allow adequate time for fat digestion and absorption in the small intestine. When you add semaglutide's gastric-slowing effects to this natural process, the result is significantly prolonged retention of fatty foods in the stomach. This extended retention period increases the likelihood of nausea, a sensation of excessive fullness, acid reflux, and in some cases, vomiting.
Fried foods present additional challenges beyond their fat content. The frying process often creates foods that are not only high in fat but also more difficult to digest. For someone taking semaglutide, whose digestive system is already working more slowly, these foods can sit in the stomach for hours, leading to persistent discomfort.
Clinical experience suggests that fat tolerance varies significantly among individuals. Many patients find that reducing portion sizes of higher-fat foods and choosing lower-fat preparation methods helps manage symptoms. Working with a registered dietitian or your healthcare provider can help you identify your personal tolerance levels and adjust your fat intake accordingly. This typically involves choosing leaner proteins, using less oil in cooking, and modifying recipes to reduce fat content while maintaining flavor and nutritional value.
Successfully managing your diet while taking semaglutide involves both avoiding problematic foods and actively choosing options that are better tolerated. A strategic approach to meal planning can significantly reduce gastrointestinal side effects while ensuring you maintain adequate nutrition for overall health.
Lean proteins form an excellent foundation for semaglutide-compatible meals. Skinless chicken breast, turkey, white fish (such as cod or tilapia), and plant-based proteins like tofu or legumes are generally well-tolerated. These foods provide essential amino acids without excessive fat content. Preparation methods matter significantly—baking, grilling, steaming, or poaching are preferable to frying.
Complex carbohydrates including whole grains, oatmeal, brown rice, quinoa, and whole wheat bread typically cause fewer problems than refined carbohydrates or sugary foods. These foods provide sustained energy and fiber, which supports digestive health. However, portion control remains important, as even well-tolerated foods can cause discomfort when consumed in large quantities given the delayed gastric emptying.
Non-starchy vegetables such as leafy greens, broccoli, cauliflower, peppers, and zucchini are usually well-tolerated and provide essential vitamins, minerals, and fiber. Steamed or roasted vegetables prepared with minimal added fat work well for most patients. Some individuals find that raw vegetables in large quantities cause bloating, so cooked vegetables may be preferable initially.
Practical eating strategies can be as important as food choices:
Eat smaller, more frequent meals rather than three large meals daily
Chew food thoroughly and eat slowly to aid digestion
Stay hydrated with water throughout the day, but avoid drinking large amounts with meals
Wait 2-3 hours after eating before lying down to reduce reflux risk
Keep a food diary to identify your personal triggers and tolerance patterns
Limit alcohol consumption, especially during dose escalation or when experiencing symptoms
For constipation, which can occur with semaglutide, gradually increase fiber intake and ensure adequate hydration. For diarrhea, focus on bland, lower-fat foods and maintain fluid and electrolyte balance. If dietary strategies don't adequately control symptoms, discuss dose adjustments with your healthcare provider.
While gastrointestinal side effects are common with semaglutide, certain symptoms warrant prompt medical evaluation. Understanding when food-related reactions require professional assessment ensures your safety and helps distinguish between expected medication effects and potentially serious complications.
Seek immediate medical attention if you experience severe, persistent abdominal pain, especially if it radiates to your back, as this could indicate pancreatitis—a rare but serious adverse effect associated with GLP-1 receptor agonists. The FDA label for semaglutide includes a warning about acute pancreatitis, and patients should discontinue the medication and seek emergency care if this condition is suspected.
Also seek emergency care for:
Persistent vomiting that prevents you from keeping down fluids or medications
Signs of dehydration (decreased urination, extreme thirst, dizziness)
Vomiting blood
Severe upper right abdominal pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Progressive abdominal distension with inability to pass gas or stool (possible intestinal obstruction)
Contact your healthcare provider within 24-48 hours if you experience persistent nausea or vomiting lasting more than a few days, as this may require dose adjustment or additional management strategies. Unintentional weight loss exceeding clinical targets, inability to maintain adequate nutrition or hydration, or new or worsening heartburn or reflux symptoms that don't respond to over-the-counter treatments also warrant medical consultation. Some patients may benefit from prescription antiemetic medications or temporary dose reduction.
If you take insulin or sulfonylureas along with semaglutide, monitor your blood glucose closely when your food intake is reduced, as you may be at risk for hypoglycemia. Contact your provider if you're unable to maintain adequate caloric intake.
Schedule a routine follow-up if you notice patterns of food intolerance that significantly limit your dietary variety, as this raises concerns about nutritional adequacy. A registered dietitian referral may be appropriate to ensure you're meeting your nutritional needs while managing symptoms. Additionally, if gastrointestinal side effects persist beyond the first 8-12 weeks of treatment or worsen over time rather than improving, discuss this with your provider, as it may indicate the need for alternative treatment approaches.
Your healthcare team can help distinguish between normal medication adjustment periods and situations requiring intervention, ensuring both the safety and effectiveness of your semaglutide therapy.
High-fat foods naturally slow gastric emptying, and when combined with semaglutide's gastric-slowing effects, they remain in the stomach for extended periods, causing prolonged fullness, nausea, and sometimes vomiting.
Lean proteins like skinless chicken and white fish, complex carbohydrates such as oatmeal and brown rice, and non-starchy vegetables prepared with minimal fat are generally well-tolerated and provide essential nutrition.
Seek immediate care for severe abdominal pain (possible pancreatitis), persistent vomiting preventing fluid intake, or signs of dehydration. Contact your provider within 24-48 hours for nausea lasting more than a few days or inability to maintain adequate nutrition.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.