LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Many people with hypothyroidism wonder whether weight loss injections are safe and effective alongside their thyroid medication. Hypothyroidism slows metabolism, making weight management particularly challenging even with optimal levothyroxine replacement. GLP-1 receptor agonists like semaglutide (Wegovy®) and tirzepatide (Zepbound®) have emerged as powerful tools for chronic weight management, but their use in patients with underactive thyroid requires careful medical evaluation. While these medications don't directly interfere with thyroid function, important safety considerations—including thyroid cancer risk factors and potential effects on thyroid hormone absorption—must be addressed before starting treatment.
Quick Answer: Weight loss injections (GLP-1 receptor agonists) can generally be used safely in patients with well-controlled hypothyroidism, as they don't directly interfere with thyroid hormone production or replacement therapy.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Hypothyroidism (underactive thyroid) occurs when the thyroid gland fails to produce sufficient thyroid hormones—primarily thyroxine (T4) and triiodothyronine (T3). These hormones regulate metabolism, energy expenditure, and numerous physiological processes throughout the body. When thyroid hormone levels drop, metabolic rate slows, often leading to unintended weight gain or difficulty losing weight despite dietary efforts.
The weight management challenges associated with hypothyroidism extend beyond simple caloric imbalance. Patients frequently experience fatigue, cold intolerance, constipation, and fluid retention, all of which can compound weight concerns. Untreated hypothyroidism may reduce basal energy expenditure, making traditional weight loss approaches less effective. Additionally, hypothyroidism can affect appetite regulation and lipid metabolism, contributing to elevated cholesterol levels alongside weight gain.
Many individuals with well-controlled hypothyroidism on levothyroxine replacement therapy continue to struggle with weight management. Even when thyroid-stimulating hormone (TSH) levels normalize within the laboratory-specific reference range, some patients report persistent difficulty achieving or maintaining a healthy weight. This has led to increased interest in adjunctive weight loss interventions, including newer injectable medications specifically designed for weight management.
Understanding the interplay between thyroid function and metabolism is essential when considering any weight loss intervention. Optimal thyroid hormone replacement remains the foundation of treatment, but additional strategies may be appropriate for select patients who continue to experience weight-related challenges despite adequate thyroid management. It's important to note that thyroid hormone should never be prescribed to treat obesity in people with normal thyroid function, as this is unsafe and carries an FDA boxed warning.
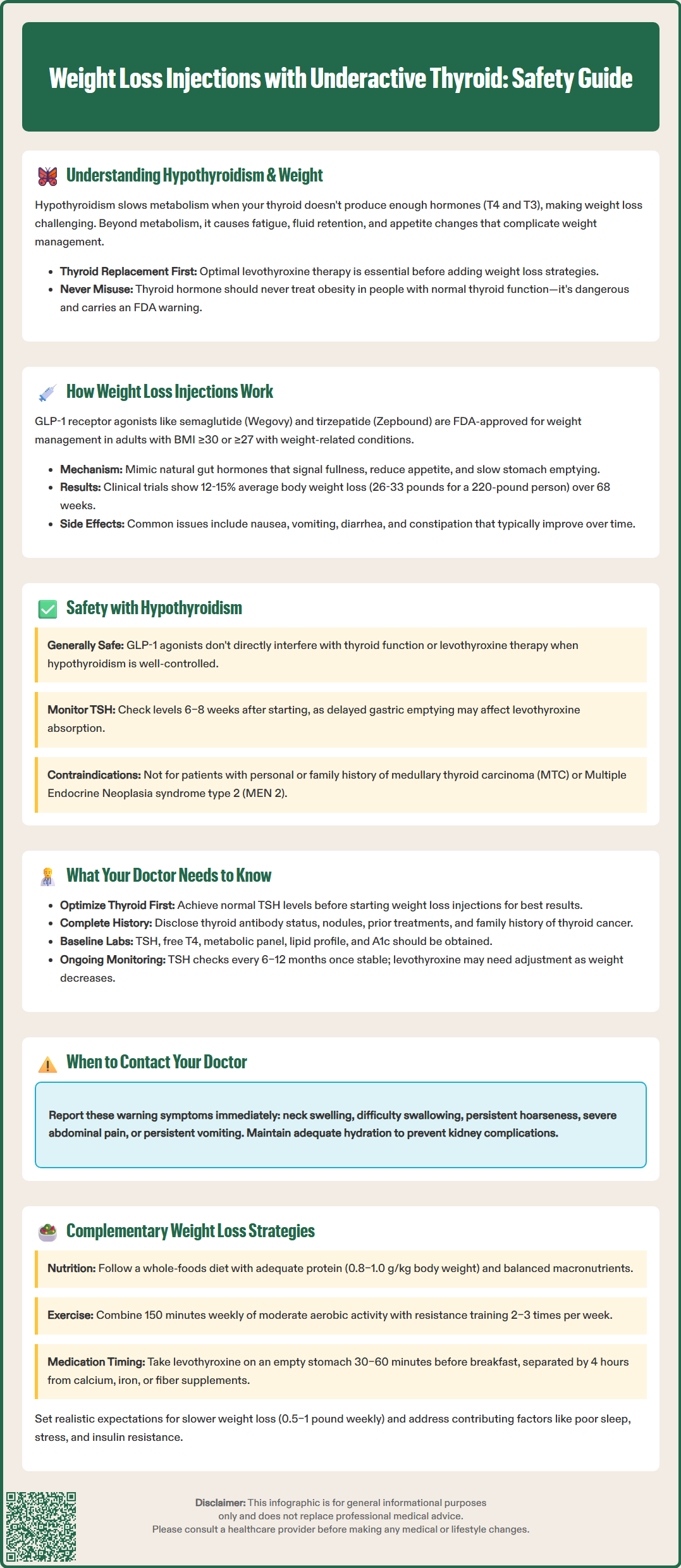
Weight loss injections primarily refer to glucagon-like peptide-1 (GLP-1) receptor agonists, a class of medications originally developed for type 2 diabetes management but now FDA-approved for chronic weight management in adults with BMI ≥30 kg/m² (or ≥27 kg/m² with at least one weight-related comorbidity such as hypertension, type 2 diabetes, or dyslipidemia). These include semaglutide (Wegovy®) and liraglutide (Saxenda®), along with newer combination agents like tirzepatide (Zepbound®), which targets both GLP-1 and glucose-dependent insulinotropic polypeptide (GIP) receptors.
These medications work through multiple complementary mechanisms. GLP-1 receptor agonists mimic naturally occurring incretin hormones that are released from the intestine in response to food intake. By binding to GLP-1 receptors in the brain—particularly in appetite-regulating centers like the hypothalamus—these agents reduce hunger signals and increase satiety. Patients typically report feeling fuller sooner during meals and experiencing reduced food cravings between meals, leading to decreased caloric intake without conscious restriction.
Beyond appetite suppression, GLP-1 receptor agonists slow gastric emptying, which prolongs the sensation of fullness after eating. They also modulate insulin secretion in a glucose-dependent manner, improving glycemic control without significantly increasing hypoglycemia risk in non-diabetic patients. In clinical trials, patients using semaglutide 2.4 mg weekly achieved average weight loss of 12–15% of body weight over 68 weeks (approximately 26-33 lbs for a 220-lb person), substantially greater than placebo.
The medications are administered via subcutaneous injection, typically weekly (semaglutide, tirzepatide) or daily (liraglutide). To minimize gastrointestinal side effects, doses are gradually increased over several weeks to months. Common adverse effects include nausea, vomiting, diarrhea, and constipation, which are generally dose-dependent and often diminish with continued use. More serious risks include pancreatitis, gallbladder disease, acute kidney injury with dehydration, suicidal ideation, and potential thyroid C-cell tumors (observed in rodent studies, though human relevance remains uncertain). Tirzepatide may reduce the effectiveness of oral contraceptives during dose initiation or escalation, requiring additional contraceptive methods during these periods.
There is no official contraindication to using GLP-1 receptor agonists in patients with hypothyroidism, and these medications do not directly interfere with thyroid hormone production or replacement therapy. The pharmacological mechanisms of GLP-1 agonists operate independently of thyroid function, targeting appetite regulation and glucose metabolism rather than thyroid hormone synthesis or action. Many patients with well-controlled hypothyroidism have safely used these weight loss injections under medical supervision.
However, important safety considerations warrant careful evaluation. GLP-1 receptor agonists carry a boxed warning regarding thyroid C-cell tumors, based on rodent studies showing increased incidence of medullary thyroid carcinoma (MTC) at high doses. While no definitive causal relationship has been established in humans, these medications are contraindicated in patients with personal or family history of MTC or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). Patients with pre-existing thyroid conditions should undergo thorough evaluation, including medical history and physical examination, before initiating treatment. The FDA does not recommend routine calcitonin testing or thyroid ultrasound screening solely for starting these medications in the absence of clinical findings.
The gastrointestinal effects of GLP-1 agonists may theoretically affect levothyroxine absorption, though clinical evidence for this interaction is limited. Levothyroxine is primarily absorbed in the small intestine, and delayed gastric emptying could potentially alter absorption kinetics. Clinicians should monitor TSH levels approximately 6–8 weeks after initiating weight loss injections to ensure thyroid hormone replacement remains adequate. Dosage adjustments may be necessary if TSH levels drift outside the therapeutic range. Additionally, significant weight loss itself may reduce levothyroxine requirements over time.
Patients should be counseled to report concerning symptoms such as neck swelling, difficulty swallowing, persistent hoarseness (potential thyroid issues), or severe abdominal pain, persistent vomiting, or right upper quadrant pain (potential pancreatitis or gallbladder issues). Maintaining adequate hydration is important to prevent acute kidney injury, especially if experiencing gastrointestinal side effects.
Before prescribing weight loss injections to patients with hypothyroidism, clinicians must conduct comprehensive medical evaluation to ensure safety and appropriateness. A detailed thyroid history is essential, including diagnosis date, current levothyroxine dosage, recent TSH and free T4 levels, presence of thyroid nodules, history of thyroid surgery or radioactive iodine treatment, and any family history of thyroid cancer or MEN 2 syndrome. Documentation of thyroid antibody status (anti-thyroid peroxidase, anti-thyroglobulin) helps characterize the underlying etiology.
Current thyroid function must be optimized before initiating weight loss medications. Patients with uncontrolled hypothyroidism (elevated TSH) should have their levothyroxine dose adjusted and thyroid function reassessed before considering additional weight loss interventions. The American Thyroid Association recommends maintaining TSH within the laboratory-specific reference range, though individual targets may vary based on age, pregnancy status, and cardiovascular risk factors. Weight loss attempts are generally less successful when thyroid function remains suboptimal.
Clinicians should evaluate for contraindications specific to GLP-1 receptor agonists, including:
Personal or family history of medullary thyroid carcinoma
Multiple Endocrine Neoplasia syndrome type 2
History of pancreatitis or gallbladder disease
Severe gastroparesis or gastrointestinal disease
History of suicidal ideation or behavior
Pregnancy or planned pregnancy (pregnancy testing when appropriate)
Diabetic retinopathy (requires monitoring in patients with diabetes)
Baseline investigations should include TSH, free T4, complete metabolic panel, lipid profile, and hemoglobin A1c (if diabetic or prediabetic). Physical examination should assess for thyroid abnormalities. Patients with palpable thyroid masses or suspicious symptoms may require further evaluation.
Ongoing monitoring includes TSH assessment 6–8 weeks after starting weight loss injections or dose changes, then every 6–12 months if stable, with levothyroxine adjustment as needed. Patients should be counseled about contraception (with backup methods during tirzepatide initiation/dose increases), hydration to prevent kidney injury, and monitoring for gallbladder symptoms.
For patients with hypothyroidism who are not candidates for weight loss injections or prefer alternative approaches, evidence-based lifestyle interventions remain foundational. Optimizing thyroid hormone replacement is the essential first step—ensuring TSH levels are within the laboratory-specific reference range maximizes metabolic function and creates a more favorable environment for weight management. Some patients benefit from combination T4/T3 therapy, though evidence supporting superiority over levothyroxine monotherapy remains limited and controversial.
Nutritional strategies should emphasize whole foods, adequate protein intake (0.8–1.0 g/kg body weight, adjusted for kidney function if needed), and mindful portion control rather than severe caloric restriction, which can further suppress metabolic rate. A balanced macronutrient distribution following US Dietary Reference Intakes (carbohydrates 45–65%, protein 10–35%, and fats 20–35%) supports satiety and metabolic health. Patients should be counseled to take levothyroxine consistently on an empty stomach, 30–60 minutes before breakfast, avoiding interference from calcium supplements, iron, fiber supplements, or certain foods that may impair absorption (separate by at least 4 hours).
Physical activity plays a crucial role despite the fatigue often associated with hypothyroidism. A combination of aerobic exercise (150 minutes weekly of moderate-intensity activity) and resistance training (2–3 sessions weekly) helps preserve lean muscle mass, which is particularly important given the metabolic slowdown in hypothyroidism. Exercise also improves insulin sensitivity, mood, and cardiovascular health—benefits that extend beyond weight management.
Complementary approaches may include:
Behavioral therapy or weight management counseling
Sleep optimization (7–9 hours nightly)
Stress management techniques
Evaluation and treatment of coexisting conditions (insulin resistance, sleep apnea, depression)
FDA-approved oral weight loss medications (orlistat, phentermine/topiramate ER, naltrexone/bupropion) as alternatives to injectables (note: phentermine monotherapy is approved for short-term use only)
Patients should maintain realistic expectations—weight loss may be slower with hypothyroidism, even when well-controlled. A goal of 0.5–1 pound weekly represents sustainable progress. Referral to endocrinology for complex cases or to registered dietitians for personalized nutrition guidance can enhance outcomes and provide additional support for patients struggling with weight management despite optimized thyroid treatment.
GLP-1 receptor agonists don't directly interfere with levothyroxine, but delayed gastric emptying may theoretically affect absorption. Your doctor should monitor TSH levels 6–8 weeks after starting treatment to ensure thyroid hormone replacement remains adequate.
Patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not use GLP-1 receptor agonists due to thyroid C-cell tumor risk observed in animal studies.
Yes, thyroid function should be optimized with TSH within the laboratory-specific reference range before initiating weight loss medications. Uncontrolled hypothyroidism makes weight loss less effective and should be addressed first.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.