LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do GLP-1 medications cause yeast infections? This question concerns many patients starting these increasingly popular diabetes and weight management therapies. GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound) are not directly linked to yeast infections in clinical trials or FDA prescribing information. Unlike SGLT2 inhibitors, which carry a well-documented risk of genital fungal infections, GLP-1 drugs do not share this mechanism. Understanding the actual relationship between these medications and infection risk helps patients make informed decisions and recognize when symptoms warrant medical attention.
Quick Answer: GLP-1 receptor agonists do not directly cause yeast infections and are not associated with increased fungal infection risk in clinical trials or FDA labeling.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for weight loss. These agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), while tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist. These medications work by mimicking naturally occurring hormones that stimulate insulin secretion in response to food intake, suppress glucagon release, slow gastric emptying, and promote satiety through central nervous system pathways.
The most commonly reported adverse effects of these medications are gastrointestinal in nature. According to FDA prescribing information, nausea occurs in approximately 15-44% of patients depending on the specific agent and dose, with vomiting, diarrhea, constipation, and abdominal pain also frequently reported. These effects typically diminish over time as patients develop tolerance, usually within the first few weeks of therapy. Other notable side effects include injection site reactions, fatigue, and headache.
More serious but less common adverse effects warrant clinical attention. These include pancreatitis (rare but reported in clinical trials and post-marketing surveillance), gallbladder disease, and acute kidney injury (particularly in the setting of severe dehydration from gastrointestinal effects). Hypoglycemia risk increases when these medications are combined with insulin or sulfonylureas. The FDA has issued a boxed warning regarding thyroid C-cell tumors observed in rodent studies, with a contraindication in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Cardiovascular outcome trials have demonstrated safety and, for specific agents (liraglutide, injectable semaglutide, dulaglutide), cardiovascular benefit, making them preferred options for patients with established cardiovascular disease. Semaglutide also carries a warning about potential worsening of diabetic retinopathy complications, particularly in patients with pre-existing retinopathy.
There is no established direct causal relationship between GLP-1 receptor agonists or tirzepatide and yeast infections in current medical literature or FDA prescribing information. Yeast infections, particularly vulvovaginal candidiasis and candidal balanitis, are not listed as recognized adverse effects specific to these medications in clinical trials or post-marketing surveillance data. This distinguishes these agents from sodium-glucose cotransporter-2 (SGLT2) inhibitors, another diabetes medication class that does carry a well-documented increased risk of genital mycotic infections due to their mechanism of causing glucosuria.
However, the question of whether GLP-1 drugs might indirectly contribute to yeast infection risk requires nuanced consideration. Any medication that affects glucose metabolism or immune function could theoretically influence infection susceptibility. The primary mechanism by which these medications might be associated with yeast infections would be through their effect on diabetes control itself—improved glycemic control generally reduces infection risk, while poorly controlled diabetes increases it.
Clinical trial data for GLP-1 receptor agonists and tirzepatide do not show elevated rates of fungal infections compared to placebo or active comparators. For example, the SUSTAIN trials evaluating semaglutide and the AWARD trials assessing dulaglutide did not identify yeast infections as a safety signal. When patients on these therapies develop yeast infections, it is more likely attributable to underlying diabetes, other medications (particularly SGLT2 inhibitors if used concomitantly), antibiotic use, or individual risk factors rather than the incretin-based agent itself. Clinicians should evaluate the complete medication regimen and clinical context when yeast infections occur in patients taking these medications.
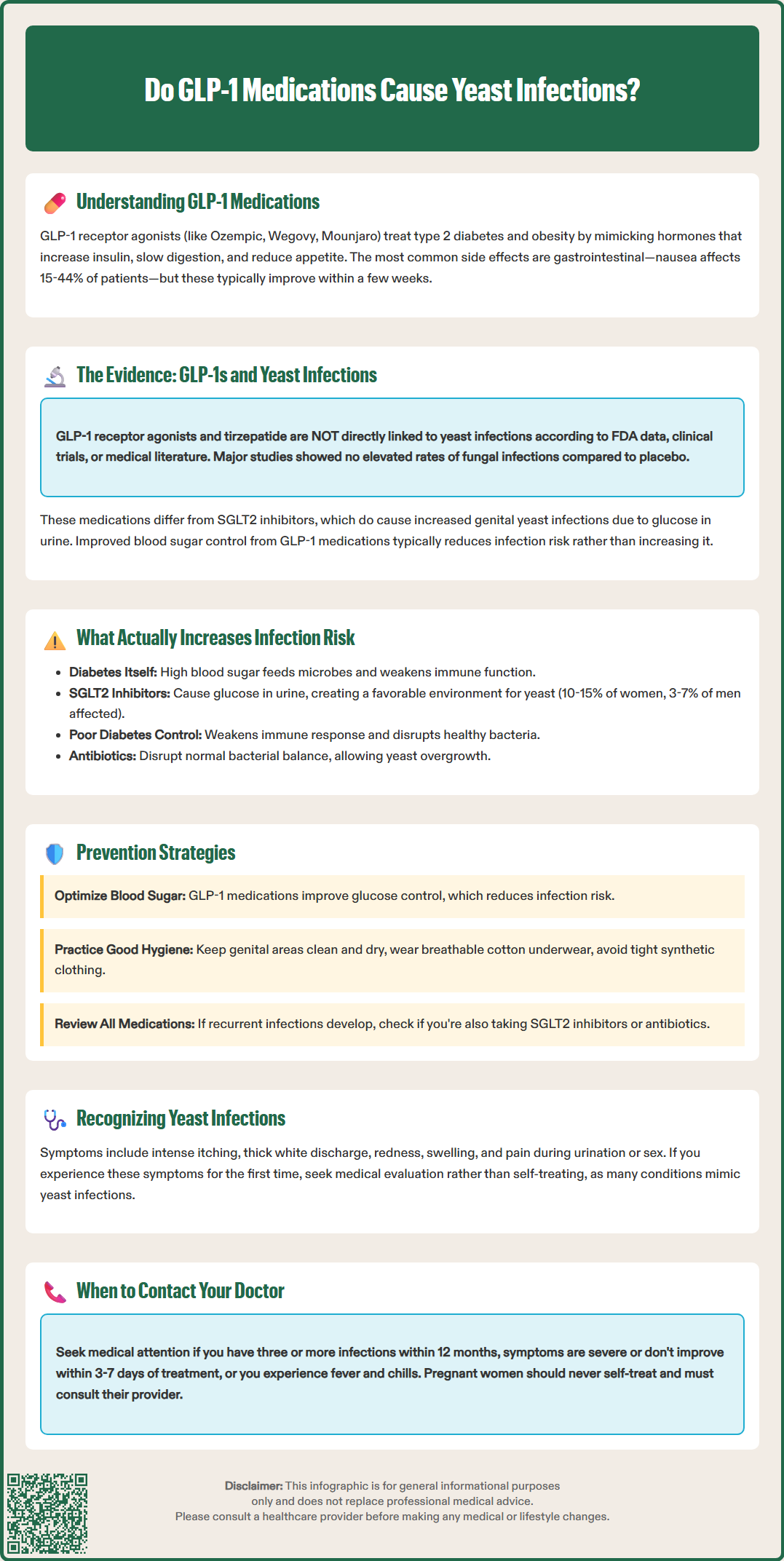
Diabetes itself, rather than most diabetes medications, represents the primary risk factor for increased infection susceptibility, including yeast infections. Elevated blood glucose levels create an environment conducive to microbial growth, particularly for Candida species. Glucose in bodily fluids and tissues provides an excellent nutrient source for yeast, while hyperglycemia impairs multiple aspects of immune function, including neutrophil chemotaxis, phagocytosis, and cell-mediated immunity. Studies demonstrate that individuals with poorly controlled diabetes have significantly higher rates of candidiasis compared to those with well-controlled diabetes or without diabetes, with risk increasing as hemoglobin A1c rises.
Certain diabetes medications do carry specific infection risks through their mechanisms of action. SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin) increase urinary glucose excretion, creating a glucose-rich environment in the genitourinary tract that promotes fungal overgrowth. Clinical trials show genital mycotic infections occur in approximately 10-15% of women and 3-7% of men taking SGLT2 inhibitors. This represents a direct pharmacological effect rather than an indirect consequence of diabetes control.
Other factors that may increase infection risk in diabetes patients include:
Immunosuppressive effects of poorly controlled hyperglycemia
Neuropathy leading to reduced sensation and delayed recognition of infections
Vascular complications impairing tissue perfusion and immune cell delivery
Frequent antibiotic use for other infections, disrupting normal flora
Obesity, which is common in type 2 diabetes and creates skin folds prone to moisture and fungal growth
Conversely, medications that improve glycemic control, including GLP-1 receptor agonists and tirzepatide, generally reduce infection risk by normalizing the metabolic environment. The American Diabetes Association emphasizes that optimal glucose management remains the cornerstone of infection prevention in diabetes patients.
Yeast infections most commonly manifest as vulvovaginal candidiasis in women or candidal balanitis in men, though oral thrush and cutaneous candidiasis can also occur. Typical symptoms include:
Intense itching and irritation in the affected area
Thick, white, cottage cheese-like vaginal discharge (in women)
Redness, swelling, and soreness of the vulva or glans penis
Pain or discomfort during urination or sexual intercourse
Burning sensation in the affected tissues
Patients starting GLP-1 therapy should understand that while these medications do not directly cause yeast infections, maintaining good diabetes control and practicing preventive measures remains important. Prevention strategies include:
Glycemic optimization: Work with your healthcare provider to achieve target blood glucose levels, as this represents the most effective prevention strategy. GLP-1 medications typically improve glucose control, which should theoretically reduce infection risk.
Hygiene practices: Keep the genital area clean and dry. Avoid douching, which disrupts normal vaginal flora. Change out of wet clothing (swimsuits, exercise attire) promptly. Choose breathable, cotton underwear and avoid tight-fitting synthetic garments.
Dietary considerations: While evidence is limited, some patients find that reducing refined sugar intake helps prevent recurrent yeast infections. Probiotic supplementation, particularly with Lactobacillus species, may help maintain healthy vaginal flora, though clinical evidence for this approach remains limited and inconclusive.
Medication review: If you develop recurrent yeast infections after starting GLP-1 therapy, review your complete medication list with your provider. If you're also taking an SGLT2 inhibitor, this medication is more likely responsible. Antibiotic use for other conditions can also trigger yeast overgrowth.
Monitoring: Patients with recurrent infections (three or more episodes per year, per CDC definition) require further evaluation to identify underlying causes, which may include uncontrolled diabetes, immunosuppression, or non-albicans Candida species that may require culture and susceptibility testing.
While yeast infections are generally not medical emergencies, certain situations warrant prompt medical evaluation. Contact your healthcare provider if you experience:
First-time symptoms: If you've never had a yeast infection diagnosed, don't self-treat. Many conditions can mimic yeast infections, including bacterial vaginosis, sexually transmitted infections, and dermatological conditions. Proper diagnosis ensures appropriate treatment.
Recurrent infections: Three or more yeast infections within 12 months suggests an underlying issue requiring investigation. Your provider should assess your diabetes control (hemoglobin A1c), review medications, and consider testing for resistant or non-albicans Candida species or other immunocompromising conditions.
Severe or worsening symptoms: Extensive redness, swelling, fissures, or ulcerations may indicate complicated infection requiring prescription antifungal therapy rather than over-the-counter treatments.
Symptoms unresponsive to treatment: If over-the-counter antifungal therapy doesn't resolve symptoms within 3-7 days, or if symptoms recur immediately after treatment, medical evaluation is necessary.
Systemic symptoms: Fever, chills, or feeling generally unwell alongside local symptoms may indicate a more serious infection requiring urgent assessment.
Pregnancy: Pregnant women should not self-treat yeast infections and require provider guidance on safe treatment options.
When discussing yeast infections with your healthcare provider while on GLP-1 therapy, provide complete information about all medications, including over-the-counter products and supplements. Your provider may check your hemoglobin A1c to assess diabetes control, review your medication regimen for potential contributors (particularly SGLT2 inhibitors), and consider whether treatment adjustments are needed. In most cases, yeast infections can be effectively treated with topical or oral antifungal medications while continuing GLP-1 therapy. While no major drug interactions between GLP-1 medications and antifungals are known, it's always best to have your healthcare provider or pharmacist review your complete medication list, as GLP-1 agents can affect the absorption of some oral medications by delaying gastric emptying. The focus should remain on optimizing diabetes management, which GLP-1 medications facilitate, thereby reducing long-term infection risk.
Semaglutide (Ozempic, Wegovy) is not associated with increased yeast infection risk in clinical trials or FDA prescribing information. Unlike SGLT2 inhibitors, GLP-1 medications do not cause the glucosuria that promotes fungal growth.
SGLT2 inhibitors (empagliflozin, dapagliflozin, canagliflozin) carry well-documented risk of genital yeast infections, occurring in approximately 10-15% of women and 3-7% of men. These medications increase urinary glucose excretion, creating an environment conducive to fungal overgrowth.
Contact your healthcare provider for first-time symptoms requiring proper diagnosis, recurrent infections (three or more per year), symptoms unresponsive to over-the-counter treatment within 3-7 days, or severe symptoms with extensive redness and swelling. Your provider should assess diabetes control and review all medications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.