LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
GLP-1 probiotics are marketed as natural alternatives to prescription weight loss medications like Ozempic and Wegovy, claiming to boost the body's production of glucagon-like peptide-1 through specific bacterial strains. Unlike FDA-approved medications that produce substantial, clinically proven weight loss, these dietary supplements lack regulatory approval and rigorous efficacy testing. While emerging research suggests gut bacteria may influence metabolic health, the evidence supporting probiotics for meaningful weight loss remains limited and preliminary. Understanding the critical differences between regulated medications and unregulated supplements is essential for patients and clinicians considering weight management options.
Quick Answer: GLP-1 probiotics lack robust clinical evidence for meaningful weight loss and are not FDA-approved alternatives to prescription medications like semaglutide or tirzepatide.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
"GLP-1 probiotics" is a marketing term (not recognized by the FDA) for dietary supplements promoted as natural alternatives to prescription medications like semaglutide (Ozempic, Wegovy) and tirzepatide (Mounjaro, Zepbound). These products typically contain specific bacterial strains—most commonly Akkermansia muciniphila, Lactobacillus species, and Bifidobacterium strains—that manufacturers claim can stimulate the body's natural production of glucagon-like peptide-1 (GLP-1).
The proposed mechanism centers on the gut microbiome's role in metabolic regulation. GLP-1 is an incretin hormone naturally produced by intestinal L-cells in response to food intake. It enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite through central nervous system pathways. Proponents suggest that certain probiotic strains may increase endogenous GLP-1 secretion by improving gut barrier function, reducing inflammation, or producing short-chain fatty acids that stimulate L-cells.
Unlike FDA-approved medications—which include GLP-1 receptor agonists (semaglutide, liraglutide) and the dual GIP/GLP-1 receptor agonist tirzepatide—probiotic supplements are classified as dietary supplements under the Dietary Supplement Health and Education Act (DSHEA). This classification means they do not require FDA approval for safety or efficacy before marketing, and manufacturers cannot legally claim to diagnose, treat, cure, or prevent disease. They may only make structure/function claims accompanied by a disclaimer stating these claims have not been evaluated by the FDA.
The fundamental difference is critical: prescription medications like semaglutide 2.4 mg (Wegovy) and tirzepatide (Zepbound) produce substantial, dose-dependent increases in receptor activation with clinical trial evidence showing approximately 15% and up to 21% body weight reduction, respectively. Probiotics, by contrast, would theoretically work by modestly influencing the body's own GLP-1 production—a far less direct and potentially much weaker effect.
The scientific evidence supporting probiotics for clinically meaningful weight loss remains limited and preliminary. While some research demonstrates that gut microbiota composition influences metabolic health, the translation to effective probiotic interventions is not straightforward.
Preclinical and mechanistic studies have shown promise. Research on Akkermansia muciniphila, for instance, indicates this bacterium may improve metabolic parameters in animal models, potentially through effects on gut barrier integrity and inflammation. Some studies suggest certain probiotic strains can modestly increase postprandial GLP-1 levels in controlled settings. However, these findings do not establish that oral probiotic supplementation produces sustained GLP-1 elevation sufficient for weight loss in humans.
Human clinical trials present mixed and modest results. A 2021 meta-analysis in Obesity Reviews examining probiotic supplementation for weight management found small effects—typically 0.5 to 2 kg greater weight loss compared to placebo over 8-12 weeks. Importantly, these studies rarely measured GLP-1 levels as a mechanism, and the strains tested varied widely. Most trials showing benefit used multi-strain formulations alongside caloric restriction, making it difficult to isolate probiotic effects.
Critical limitations include:
Heterogeneity: Different strains, doses, and formulations make comparisons difficult
Small effect sizes: Weight changes are typically modest and may not be clinically significant
Short duration: Most studies last 12 weeks or less, providing no data on sustained effects
Publication bias: Negative studies may be underreported
There is no high-quality evidence that probiotic supplements can replicate the substantial weight loss achieved with prescription medications like semaglutide or tirzepatide. No probiotic has FDA approval for weight management. The American Gastroenterological Association's 2020 guidelines on probiotics primarily address gastrointestinal conditions and do not recommend probiotics for obesity or metabolic conditions due to insufficient evidence.
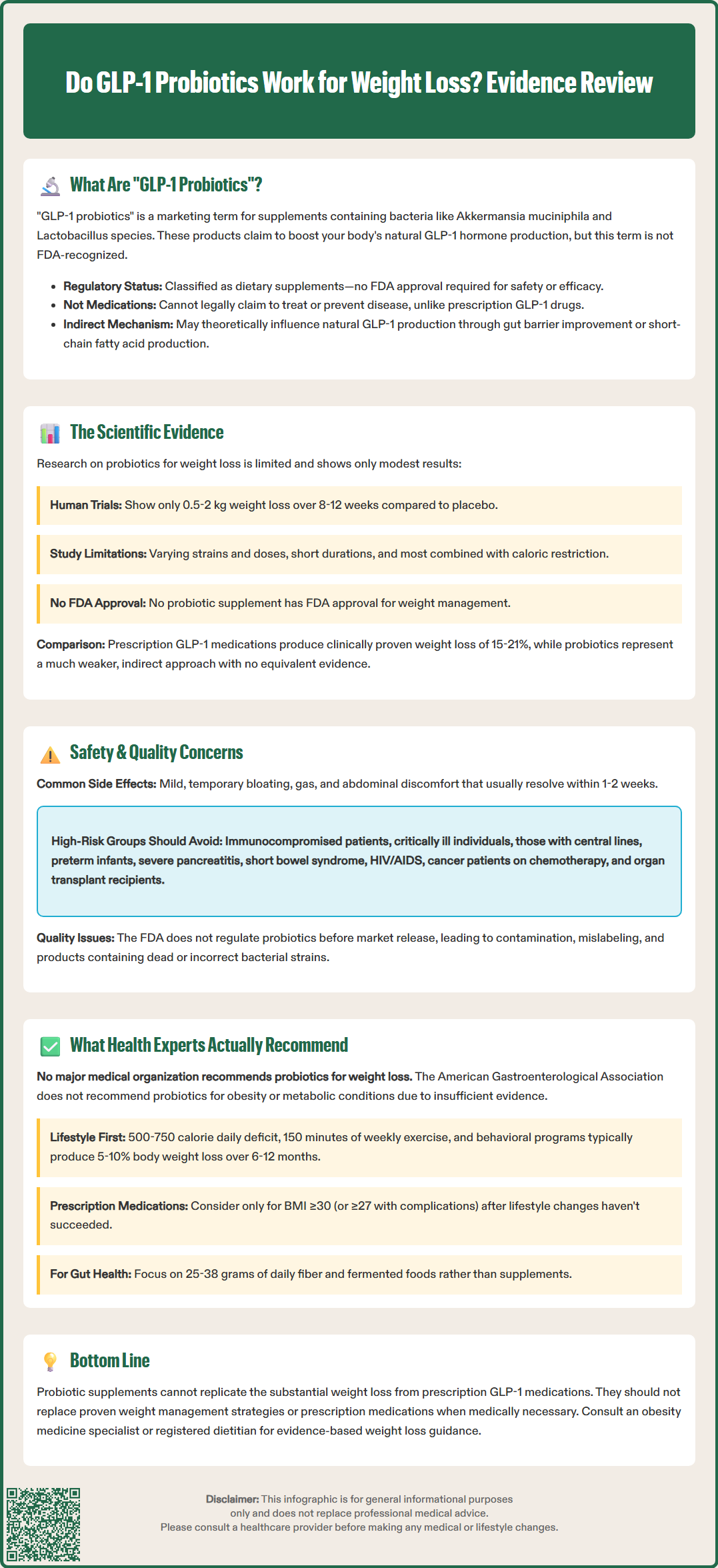
Probiotic supplements are generally considered safe for healthy individuals, but several safety considerations warrant attention, particularly given the unregulated nature of the supplement market.
Common adverse effects associated with probiotic use are typically mild and gastrointestinal in nature:
Bloating and gas, especially during the first few days of use
Abdominal discomfort or cramping
Changes in bowel habits (diarrhea or constipation)
Nausea (less common)
These symptoms usually resolve within one to two weeks as the gut microbiome adjusts. However, unlike prescription medications with standardized formulations and FDA oversight, probiotic supplements vary significantly in quality, strain viability, and actual content compared to label claims.
Serious safety concerns are rare but include:
Systemic infections: Immunocompromised individuals, those with central venous catheters, or patients with damaged gut barriers face increased risk of bacteremia or fungemia from probiotic organisms
Antibiotic resistance transfer: Some probiotic strains may carry antibiotic resistance genes
Metabolic complications: Rare cases of D-lactic acidosis have been reported with high-dose probiotic use
Specific populations requiring caution include patients with severe acute pancreatitis (based on the PROPATRIA trial showing increased mortality), short bowel syndrome, immunosuppression (HIV/AIDS, chemotherapy, organ transplant recipients), and critically ill individuals. The American Gastroenterological Association recommends against probiotic use in critically ill patients due to potential harm. The FDA issued a 2023 safety communication advising against probiotic use in preterm infants due to risk of invasive disease. Pregnant women and children should consult healthcare providers before using probiotics.
Regulatory concerns are significant. The FDA does not verify supplement contents before marketing, and independent testing has revealed problems with contamination, mislabeling, and lack of viable organisms in commercial products. Patients should be advised that "GLP-1 probiotic" marketing claims are not FDA-evaluated and may be misleading. Healthcare providers should counsel patients that these products are not substitutes for evidence-based weight management strategies or prescription medications when clinically indicated.
Evidence-based weight management requires a comprehensive approach, and health experts emphasize that no single supplement—including probiotics—should be considered a primary intervention for obesity or overweight.
First-line recommendations from the American Diabetes Association, American College of Physicians, and U.S. Preventive Services Task Force focus on lifestyle modification:
Caloric restriction: Creating a 500-750 kcal/day deficit through reduced intake
Physical activity: At least 150 minutes of moderate-intensity aerobic exercise weekly, plus resistance training
Behavioral interventions: Structured programs addressing eating behaviors, self-monitoring, and psychological factors
Dietary patterns: Mediterranean, DASH, or plant-based diets with emphasis on whole foods, fiber, and nutrient density
These interventions typically produce 5-10% body weight loss over 6-12 months when implemented consistently—modest but clinically meaningful for reducing cardiovascular and metabolic risk.
Pharmacotherapy should be considered for patients with BMI ≥30 kg/m² or BMI ≥27 kg/m² with weight-related comorbidities who have not achieved goals with lifestyle modification alone. FDA-approved options include GLP-1 receptor agonists (semaglutide, liraglutide) and the dual GIP/GLP-1 receptor agonist tirzepatide, which demonstrate superior efficacy compared to older agents. These medications require prescription, monitoring, and integration with lifestyle changes.
Regarding probiotics specifically, expert guidance suggests:
No major medical organization currently recommends probiotics as a weight loss intervention
Patients interested in gut health optimization should focus on dietary fiber (25g daily for women, 38g daily for men) and fermented foods rather than supplements
If patients choose to use probiotics, they should inform their healthcare provider and select products from reputable manufacturers with third-party testing (USP, NSF, ConsumerLab)
Clinical referral triggers include patients seeking probiotics as alternatives to indicated medical therapy, those with unrealistic weight loss expectations, or individuals with eating disorders. Clinicians should address underlying motivations and provide evidence-based counseling. For patients with obesity and comorbidities (type 2 diabetes, hypertension, sleep apnea), referral to obesity medicine specialists or registered dietitians is appropriate for comprehensive management.
No, GLP-1 probiotics are not as effective as prescription medications. Clinical trials show probiotics produce modest weight loss of 0.5-2 kg, while FDA-approved medications like semaglutide and tirzepatide demonstrate 15-21% body weight reduction with robust clinical evidence.
While generally safe for healthy individuals, probiotics can cause bloating, gas, and gastrointestinal discomfort. Serious risks include systemic infections in immunocompromised patients, and the FDA advises against use in critically ill patients and preterm infants due to potential harm.
Medical experts recommend evidence-based approaches including caloric restriction, at least 150 minutes of weekly exercise, behavioral interventions, and dietary patterns like Mediterranean or DASH diets. For patients with BMI ≥30 or ≥27 with comorbidities, FDA-approved pharmacotherapy may be appropriate alongside lifestyle modification.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.