LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Tirzepatide (Mounjaro for type 2 diabetes, Zepbound for weight management) is a dual GIP/GLP-1 receptor agonist that offers powerful glycemic control and weight reduction through once-weekly subcutaneous injection. Maximizing therapeutic outcomes requires more than just administering the medication—proper injection technique, strategic side effect management, lifestyle integration, and correct storage practices are essential for treatment success. This comprehensive guide provides practical tirzepatide tips and tricks to help patients and healthcare providers optimize therapy, minimize adverse effects, and achieve sustainable results. From site rotation strategies to dietary modifications and travel considerations, these evidence-based recommendations address the real-world challenges of tirzepatide therapy.
Quick Answer: Optimizing tirzepatide therapy requires proper injection technique with systematic site rotation, proactive gastrointestinal side effect management through dietary modifications, integration with lifestyle changes including adequate protein intake and regular exercise, and correct storage at refrigerated temperatures.
Tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management (Mounjaro) and chronic weight management (Zepbound). This novel mechanism enhances insulin secretion, suppresses glucagon release, slows gastric emptying, and reduces appetite, making it effective for glycemic control and weight reduction.
Before initiating tirzepatide, patients should undergo comprehensive evaluation including assessment of renal function and obtaining personal and family history of medullary thyroid carcinoma (MTC) or multiple endocrine neoplasia syndrome type 2 (MEN 2). Routine calcitonin testing or thyroid ultrasound is not recommended. The medication carries a boxed warning regarding thyroid C-cell tumors observed in rodent studies, though there is no established link in humans. Contraindications include personal or family history of MTC or MEN 2. Tirzepatide is not recommended in patients with severe gastrointestinal disease, including severe gastroparesis, and is not indicated for type 1 diabetes.
Patients should understand that tirzepatide requires once-weekly subcutaneous injection, with dosing typically starting at 2.5 mg and gradually titrating upward every four weeks (up to 15 mg) to minimize gastrointestinal adverse effects. The American Diabetes Association recommends GLP-1 receptor agonists with proven cardiovascular benefit for patients with established cardiovascular disease, while SGLT2 inhibitors are preferred for chronic kidney disease protection. Tirzepatide should not be coadministered with other GLP-1 receptor agonists.
Additional important safety considerations include monitoring for gallbladder disease, acute kidney injury with dehydration, and diabetic retinopathy (particularly with rapid A1c reduction). Women of childbearing potential should be advised that tirzepatide may reduce the effectiveness of oral contraceptives; alternative contraception methods are recommended for 4 weeks after initiation and after each dose increase. Tirzepatide should be discontinued at least 1 month before a planned pregnancy.
Setting realistic expectations about gradual dose escalation, potential side effects, and the importance of adherence to both medication and lifestyle modifications is essential for treatment success. Patients should also verify insurance coverage, as cost can be a significant barrier to access.
Proper injection technique is fundamental to maximizing tirzepatide efficacy and minimizing injection site reactions. Tirzepatide is administered subcutaneously in the abdomen, thigh, or upper arm (upper arm injections should be administered by a caregiver, not self-administered). The medication comes in a single-dose pen with an integrated needle that should be used once and then properly disposed of.
Site rotation is critical to prevent lipohypertrophy (fatty lumps) or lipoatrophy (tissue depression), which can impair medication absorption and cause discomfort. Patients should maintain a systematic rotation pattern, never injecting into the same spot within at least one inch of a previous injection site. A practical approach involves dividing each injection area into quadrants and rotating through them sequentially, keeping a simple log or using smartphone reminders to track locations.
Before injection, allow the pen to reach room temperature for 30 minutes to reduce injection discomfort. Clean the injection site with an alcohol swab and allow it to dry completely—injecting through wet alcohol can cause stinging. To administer the injection, place the clear base flat against the skin, unlock the pen, press and hold the injection button, listen for clicks, and hold for approximately 10 seconds until you see the gray plunger in the window, then remove.
Never inject into areas with bruising, scarring, or active skin conditions. If injection site reactions such as redness, itching, or swelling occur and persist beyond a few days, patients should contact their healthcare provider to rule out hypersensitivity reactions or infection. After use, dispose of the entire pen in an FDA-cleared sharps container—do not attempt to reuse the pen or remove the needle.
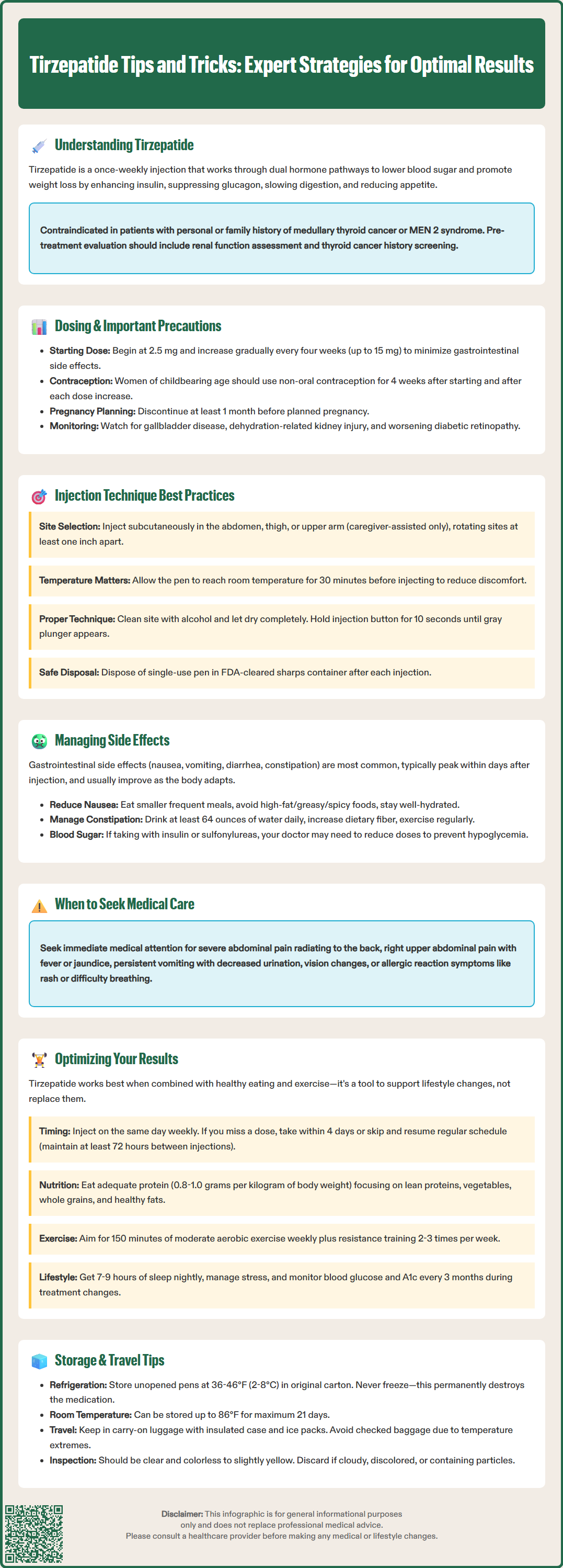
Gastrointestinal adverse effects are the most common challenges with tirzepatide, with frequency increasing at higher doses. Nausea, vomiting, diarrhea, constipation, and abdominal discomfort typically peak within the first few days after injection and often diminish with continued use as the body adapts to the medication's effects on gastric motility.
To minimize nausea, patients should eat smaller, more frequent meals rather than three large meals daily. Avoiding high-fat, greasy, or spicy foods can significantly reduce gastrointestinal distress, as tirzepatide already slows gastric emptying. Staying well-hydrated is essential, particularly if experiencing vomiting or diarrhea, to prevent dehydration and potential acute kidney injury. Ginger tea or peppermint may provide symptomatic relief for mild symptoms. For more significant nausea, patients should consult their healthcare provider about prescription antiemetics rather than relying on over-the-counter options. If nausea is severe or persistent, delaying dose escalation or temporarily reducing the dose may be appropriate.
Constipation management requires adequate fluid intake (at least 64 ounces daily unless fluid restricted), increased dietary fiber through fruits, vegetables, and whole grains, and regular physical activity. Over-the-counter stool softeners or osmotic laxatives like polyethylene glycol can be used as needed. For diarrhea, focus on oral rehydration solutions and easily digestible foods; the BRAT diet (bananas, rice, applesauce, toast) may be used short-term, but patients should return to a balanced diet as soon as tolerated.
When tirzepatide is combined with insulin or sulfonylureas, consider reducing doses of these medications to mitigate hypoglycemia risk, especially when initiating or uptitrating tirzepatide.
Serious adverse effects requiring immediate medical attention include severe abdominal pain radiating to the back (potential pancreatitis), right upper quadrant pain, fever, or jaundice (potential gallbladder disease), persistent vomiting preventing oral intake or reduced urination (dehydration/kidney injury risk), visual changes (diabetic retinopathy concerns), or signs of allergic reaction such as rash, difficulty breathing, or facial swelling.
Maximizing tirzepatide's therapeutic benefits requires integration with comprehensive lifestyle modifications. While the medication provides powerful pharmacological support for weight loss and glycemic control, outcomes are significantly enhanced when combined with evidence-based dietary patterns and physical activity. Patients should view tirzepatide as a tool that facilitates lifestyle changes rather than a replacement for them.
Timing of the weekly injection can be optimized based on individual schedules and side effect patterns. Many patients prefer injecting on the same day each week when they have flexibility to rest if gastrointestinal symptoms occur—often Friday evening or Saturday morning. The injection can be administered at any time of day, with or without meals, though consistency helps establish routine adherence. If a dose is missed, it should be administered within four days; if more than four days have passed, skip the missed dose and resume the regular schedule. When changing injection days or making up a missed dose, ensure at least 72 hours between injections.
Dietary optimization should focus on adequate protein intake (0.8-1.0 grams per kilogram body weight for most patients; those with chronic kidney disease may require individualized targets) to preserve lean muscle mass during weight loss, as tirzepatide's appetite suppression can inadvertently lead to inadequate protein consumption. Emphasize nutrient-dense foods including lean proteins, non-starchy vegetables, whole grains, and healthy fats while limiting ultra-processed foods and added sugars. The Mediterranean or DASH dietary patterns align well with diabetes management goals.
Physical activity recommendations include at least 150 minutes of moderate-intensity aerobic exercise weekly, combined with resistance training two to three times per week, individualized based on cardiovascular status and physical limitations. Exercise not only enhances weight loss but also improves insulin sensitivity, cardiovascular health, and helps maintain metabolic rate during caloric restriction. Patients should also prioritize sleep hygiene (7-9 hours nightly) and stress management, as both significantly impact metabolic health and weight regulation. Regular monitoring of blood glucose, weight trends, and hemoglobin A1c every three months during therapy changes (extending to every six months when stable at goal) allows for objective assessment of treatment response and timely adjustments.
Proper storage and handling of tirzepatide are essential to maintain medication stability and efficacy. Unopened tirzepatide pens must be refrigerated at 36-46°F (2-8°C) and should never be frozen—freezing permanently damages the medication, rendering it ineffective. Store pens in their original carton to protect from light until ready for use. Unopened pens may be kept at room temperature up to 86°F (30°C) for up to 21 days. Remember that tirzepatide pens are single-use only; use once and then properly dispose of the entire pen.
When traveling, patients should plan ahead to ensure medication integrity. For short trips, an insulated medication travel case with ice packs (ensuring the pen doesn't directly contact ice) maintains appropriate temperature. For air travel, tirzepatide should be carried in carry-on luggage rather than checked baggage, as cargo holds can experience temperature extremes. The Transportation Security Administration (TSA) permits medications and associated supplies; patients should carry their prescription or a letter from their healthcare provider documenting medical necessity. When traveling across time zones, maintain the weekly injection schedule based on the original time zone, or adjust by one to two days if necessary to accommodate the new schedule, ensuring at least 72 hours between doses.
Before each injection, inspect the medication visually—tirzepatide should be clear and colorless to slightly yellow. Do not use if the solution appears cloudy, discolored, or contains particles. Never share pens between patients due to infection risk. Used pens should be disposed of in an FDA-cleared sharps container; if unavailable, use a heavy-duty plastic container with a secure lid, labeled clearly. Many communities offer sharps disposal programs or mail-back services. Keep all medications out of reach of children and pets, and never dispose of medications in household trash or flush down toilets unless specifically instructed, as this can contaminate water supplies.
Eat smaller, more frequent meals rather than three large meals, avoid high-fat, greasy, or spicy foods, and stay well-hydrated. If nausea persists, consult your healthcare provider about prescription antiemetics or delaying dose escalation.
Rotate between the abdomen, thigh, and upper arm, never injecting within one inch of a previous injection site. Divide each area into quadrants and rotate systematically, keeping a log to track locations and prevent lipohypertrophy.
Yes, carry tirzepatide in your carry-on luggage using an insulated medication travel case with ice packs to maintain proper temperature. Unopened pens must stay refrigerated at 36-46°F or can be kept at room temperature up to 86°F for up to 21 days.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.