LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Weight loss injections like semaglutide (Wegovy) and tirzepatide (Zepbound) have become important FDA-approved treatments for chronic weight management in the United States. While these GLP-1 and dual GIP/GLP-1 receptor agonists effectively reduce appetite and support weight loss, patients may experience side effects including fatigue. Understanding whether these medications directly cause tiredness, the contributing factors, and effective management strategies is essential for patients and healthcare providers. This article examines the relationship between weight loss injections and fatigue, exploring mechanisms, clinical evidence, and practical approaches to maintaining energy levels during treatment.
Quick Answer: Yes, weight loss injections can cause fatigue, which is listed as a common adverse reaction occurring in ≥5% of patients in FDA prescribing information for both Wegovy and Zepbound.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections have emerged as a significant therapeutic option for obesity management in the United States. The most commonly prescribed medications in this category include semaglutide 2.4 mg (Wegovy) and tirzepatide (Zepbound), which are FDA-approved specifically for chronic weight management. Semaglutide belongs to the GLP-1 receptor agonist class, while tirzepatide is a dual GIP/GLP-1 receptor agonist (incretin co-agonist). Ozempic (semaglutide) and Mounjaro (tirzepatide) are related medications approved for type 2 diabetes, not weight management.
These medications work by mimicking naturally occurring hormones that regulate appetite and blood sugar. GLP-1 (glucagon-like peptide-1) is an incretin hormone released by the intestines after eating. When these injections activate GLP-1 receptors in the brain, they reduce hunger signals and increase feelings of fullness. They also slow gastric emptying, meaning food stays in the stomach longer, which contributes to prolonged satiety.
Additionally, these medications improve insulin secretion from the pancreas in response to meals and reduce glucagon release, helping to stabilize blood glucose levels. This dual effect on appetite regulation and glucose metabolism makes them effective for both weight loss and type 2 diabetes management. The FDA has approved Wegovy and Zepbound for chronic weight management in adults with obesity (BMI ≥30 kg/m²) or overweight (BMI ≥27 kg/m²) with at least one weight-related comorbidity.
These injections are administered subcutaneously, typically once weekly, and are intended to be used alongside lifestyle modifications including reduced-calorie diet and increased physical activity. Understanding how these medications work provides important context for recognizing and managing potential side effects, including fatigue.
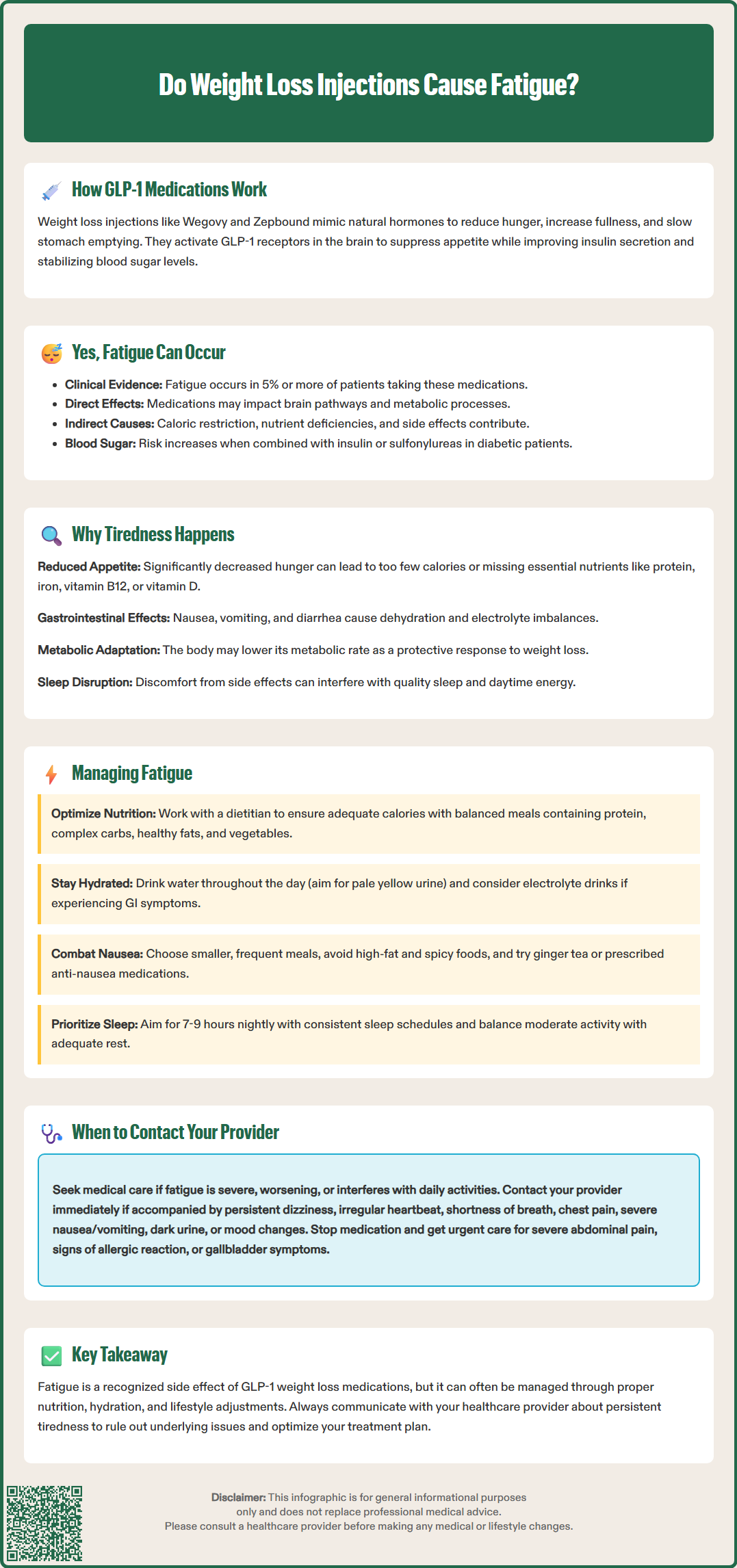
Fatigue is listed as a common adverse reaction (occurring in ≥5% of patients) in the FDA prescribing information for both Wegovy (semaglutide 2.4 mg) and Zepbound (tirzepatide), and occurred more frequently than with placebo in clinical trials. While gastrointestinal symptoms (nausea, vomiting, diarrhea, constipation, and abdominal pain) are the most frequently reported side effects, fatigue and asthenia (weakness) are recognized drug-associated effects.
The experience of fatigue during treatment with weight loss injections likely has multiple contributing factors. There may be direct pharmacological effects through central GLP-1 pathways, as well as indirect consequences of the medication's intended actions and associated side effects. The body's adaptation to significant caloric restriction and metabolic changes during weight loss can also contribute to feelings of tiredness.
It's important to note that these medications generally have a low risk of hypoglycemia when used alone. However, when combined with insulin or sulfonylureas (in patients with diabetes), the risk of low blood sugar increases significantly, which can manifest as fatigue, weakness, and other symptoms. Patients taking these combinations may require dose adjustments of their diabetes medications.
Healthcare providers should take patient reports of fatigue seriously and conduct appropriate evaluation to determine the underlying cause. Understanding both the direct and indirect factors contributing to fatigue helps guide appropriate management strategies and medication adjustments when necessary.
Several physiological and behavioral factors can contribute to fatigue during weight loss injection therapy. Understanding these mechanisms helps patients and providers address tiredness effectively.
Caloric deficit and nutritional inadequacy represent a common cause of fatigue. GLP-1 receptor agonists and GIP/GLP-1 co-agonists significantly reduce appetite, and some patients may inadvertently consume too few calories or miss essential nutrients. When caloric intake drops below the body's baseline needs, energy levels naturally decline. Additionally, inadequate protein intake can lead to muscle loss and weakness, while insufficient iron, vitamin B12, or vitamin D can cause fatigue.
Gastrointestinal side effects frequently contribute to tiredness. Persistent nausea may prevent adequate food and fluid intake, while vomiting and diarrhea can lead to dehydration and electrolyte imbalances. Severe or prolonged fluid losses can potentially lead to acute kidney injury in some cases. Dehydration commonly causes fatigue, headache, and difficulty concentrating. The body's effort to manage ongoing GI symptoms can also be physically draining.
Metabolic adaptation occurs as the body adjusts to weight loss. During significant caloric restriction, the body may reduce its metabolic rate as a protective mechanism, which can manifest as decreased energy. Additionally, rapid weight loss can temporarily affect thyroid hormone levels, though this is typically a normal adaptive response rather than medication-induced thyroid dysfunction.
Blood sugar fluctuations may occur, particularly in patients with diabetes or prediabetes. While these medications generally stabilize glucose levels, patients taking insulin or sulfonylureas may experience hypoglycemia if these medications aren't appropriately adjusted. Even in patients without diabetes, the body may need time to adapt to more stable glucose levels.
Sleep disruption can result from gastrointestinal discomfort or other factors. Poor sleep quality directly impacts daytime energy levels and overall well-being.
Addressing fatigue during weight loss injection therapy requires a multifaceted approach focused on nutrition, hydration, and lifestyle optimization.
Ensure adequate caloric and nutritional intake. Work with a registered dietitian nutritionist (RDN) to establish appropriate calorie targets that support weight loss while providing sufficient energy. Aim for balanced meals containing adequate protein, complex carbohydrates, healthy fats, and vegetables. Protein needs are individualized but generally important for preserving muscle mass during weight loss. Discuss with your healthcare provider whether nutritional supplements might be beneficial based on your specific needs and dietary intake.
Prioritize hydration. Aim for adequate fluid intake throughout the day, with a goal of pale yellow urine as a sign of good hydration. Fluid needs vary by individual; those with heart failure, kidney disease, or other conditions may have specific fluid restrictions that should be followed. Electrolyte-containing beverages may be beneficial if experiencing significant fluid losses from diarrhea or vomiting.
Optimize medication administration. Follow the prescribed dosing schedule, maintaining a consistent weekly injection day. Time of day for administration can be based on personal preference and schedule. If side effects are severe, your provider may recommend temporarily pausing dose escalation or reducing the dose according to the FDA-approved titration schedule.
Manage gastrointestinal symptoms proactively. Eat smaller, more frequent meals rather than large portions. Avoid high-fat, spicy, or heavily processed foods that may worsen nausea. Ginger tea, bland foods, and anti-nausea medications (if prescribed) can help manage symptoms that interfere with adequate nutrition.
Maintain appropriate physical activity. While exercise is important for weight loss maintenance and overall health, avoid overexertion if feeling fatigued. Focus on moderate activities like walking, and ensure adequate rest between exercise sessions. Physical activity can actually improve energy levels over time, but the intensity should match your current energy capacity.
Prioritize sleep hygiene. Aim for 7-9 hours of quality sleep nightly. Establish consistent sleep and wake times, create a comfortable sleep environment, and address any factors disrupting sleep quality.
While mild tiredness may be manageable with lifestyle adjustments, certain presentations of fatigue warrant prompt medical evaluation. Patients should contact their healthcare provider if they experience any of the following:
Severe or worsening fatigue that interferes with daily activities, work, or self-care, or fatigue that progressively worsens despite implementing management strategies. This may indicate an underlying medical condition requiring investigation.
Fatigue accompanied by other concerning symptoms including:
Persistent dizziness, lightheadedness, or fainting
Rapid or irregular heartbeat
Shortness of breath or chest pain
Severe or unrelenting nausea and vomiting
Inability to keep down food or fluids for more than 24 hours
Dark urine, markedly reduced urination, or swelling (signs of dehydration or kidney problems)
Yellowing of skin or eyes
Severe abdominal pain
Mood changes, depression, or difficulty concentrating
Signs of potential complications require immediate attention:
Stop the medication and seek urgent medical care if you experience severe abdominal pain (especially radiating to the back) which could suggest pancreatitis
Stop the medication and seek urgent care if you develop symptoms of severe allergic reaction (rash, itching, swelling, severe dizziness, trouble breathing)
Symptoms suggesting gallbladder disease (right upper abdominal pain, especially after eating)
Hypoglycemia in patients taking diabetes medications (shakiness, sweating, confusion)
Inability to meet nutritional needs despite best efforts, or unintentional weight loss exceeding recommended rates (generally more than 1-2 pounds per week after the initial period).
Your provider may recommend laboratory testing to evaluate for anemia, thyroid dysfunction, electrolyte imbalances, vitamin deficiencies, kidney function, or liver function. They can also assess whether medication adjustment, additional supportive therapies, or referral to specialists (such as a dietitian nutritionist or endocrinologist) would be beneficial. In most cases, do not discontinue weight loss injections without consulting your healthcare provider, as they can help determine whether fatigue is related to the medication or another treatable cause.
Fatigue is listed as a common adverse reaction in FDA prescribing information, occurring in 5% or more of patients taking Wegovy (semaglutide 2.4 mg) and Zepbound (tirzepatide), with higher frequency than placebo in clinical trials.
Tiredness may result from multiple factors including direct medication effects, inadequate caloric or nutritional intake due to reduced appetite, dehydration from gastrointestinal side effects, metabolic adaptation to weight loss, and blood sugar fluctuations in patients taking diabetes medications.
Contact your healthcare provider for severe or worsening fatigue interfering with daily activities, fatigue accompanied by dizziness, chest pain, severe nausea, inability to keep down fluids for over 24 hours, dark urine, severe abdominal pain, or signs of allergic reaction.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.