LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Should I take GLP-1 in the morning or at night? For most GLP-1 receptor agonists, the answer depends on your specific medication and personal routine. Daily formulations like liraglutide (Victoza, Saxenda) can be taken at any time, while oral semaglutide (Rybelsus) must be taken before your first meal of the day. Weekly injections such as semaglutide (Ozempic, Wegovy) and dulaglutide (Trulicity) offer even greater flexibility. Understanding FDA labeling guidance, your lifestyle factors, and how timing affects side effects will help you and your healthcare provider determine the optimal schedule for your GLP-1 therapy.
Quick Answer: Most GLP-1 medications can be taken at any consistent time of day, though specific formulations have different requirements based on FDA labeling.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications primarily used for managing type 2 diabetes and, in some formulations, for chronic weight management. These medications work by mimicking the action of naturally occurring GLP-1, an incretin hormone that stimulates insulin secretion in response to food intake, suppresses glucagon release, slows gastric emptying, and promotes satiety through central nervous system pathways.
FDA-approved GLP-1 medications in the United States include both daily and weekly formulations. Daily options include liraglutide (Victoza, Saxenda), while weekly injectable formulations include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and exenatide extended-release (Bydureon BCise). An oral formulation of semaglutide (Rybelsus) is also available. Each medication has specific FDA-approved dosing instructions that healthcare providers tailor to individual patient needs.
The pharmacokinetic properties of GLP-1 medications vary considerably. Short-acting formulations reach peak plasma concentrations within 1-3.5 hours and have shorter elimination half-lives, while long-acting agents like semaglutide have half-lives of approximately one week, allowing for sustained therapeutic effects. These pharmacological differences influence the timing recommendations in FDA labeling.
Dosing schedules for GLP-1 medications are established through clinical trials that evaluate efficacy, safety, and patient adherence. While manufacturers provide specific timing recommendations in FDA labeling, individual patient factors may influence the most appropriate administration time. The question of morning versus evening dosing is particularly relevant for daily formulations, where timing flexibility may improve treatment adherence and minimize side effects.
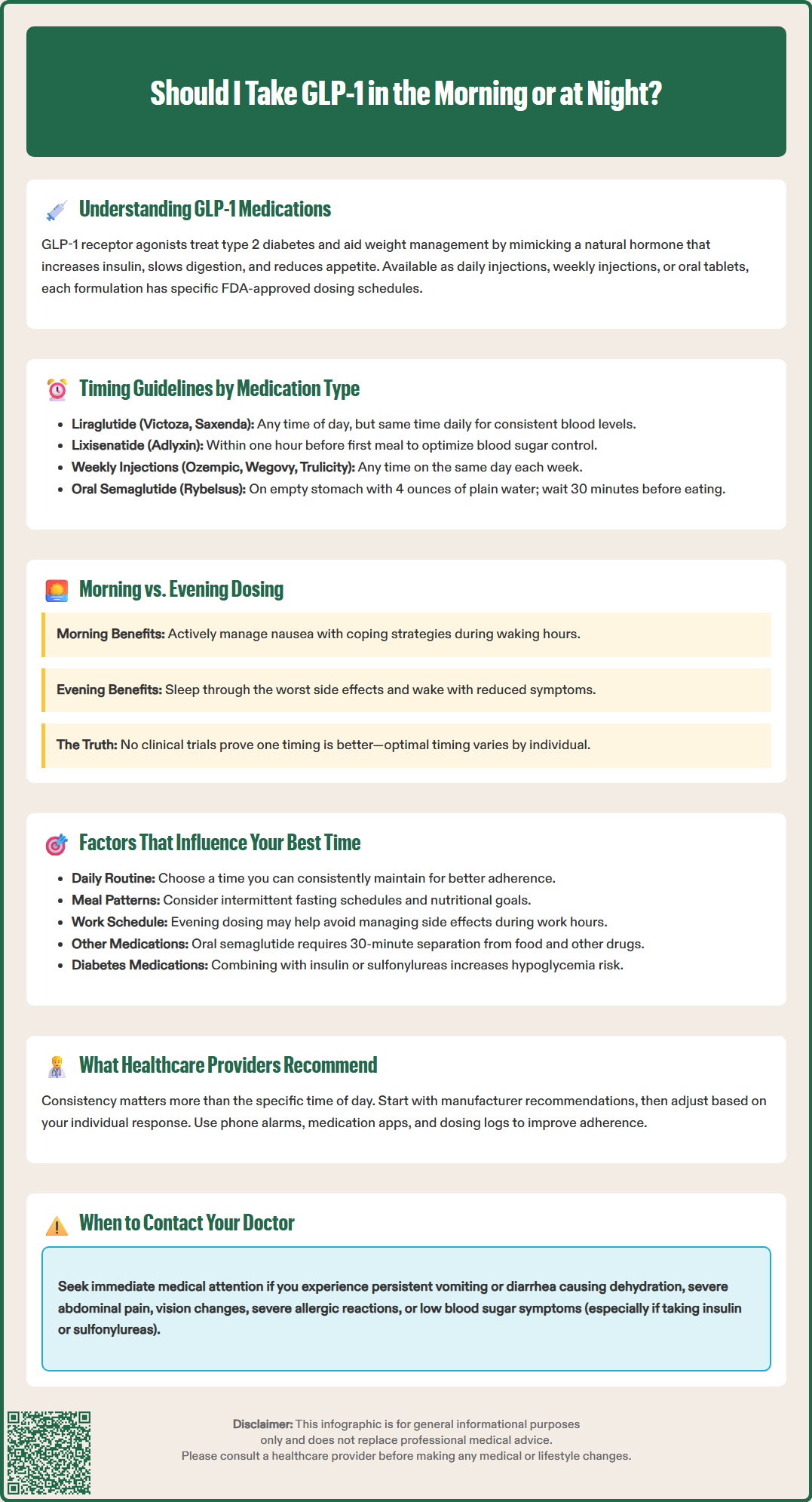
For most GLP-1 medications, the FDA labeling provides specific guidance on administration timing. Liraglutide (Victoza, Saxenda) can be administered at any time of day, with or without meals, but should be taken at approximately the same time each day to maintain consistent plasma levels. The prescribing information does not mandate morning or evening administration, allowing flexibility based on patient preference and lifestyle.
Lixisenatide (Adlyxin), when prescribed, is specifically indicated for administration within one hour before the first meal of the day. This timing recommendation is based on the medication's short-acting profile and its mechanism of slowing gastric emptying, which is most beneficial when timed with food intake. Taking lixisenatide before the first meal helps optimize postprandial glucose control throughout the day.
For weekly GLP-1 medications such as semaglutide (Ozempic, Wegovy) and dulaglutide (Trulicity), timing is less critical due to their extended half-lives and sustained therapeutic effects. These medications can be administered at any time of day, with or without meals, on the same day each week. If a dose is missed, patients should follow specific FDA guidance: for Ozempic, administer within 5 days of the missed dose; for Trulicity, administer if at least 3 days before the next scheduled dose; for Wegovy, administer if at least 2 days before the next scheduled dose.
Oral semaglutide (Rybelsus) requires specific administration instructions: it must be taken on an empty stomach before the first food, beverage, or other oral medications of the day, with no more than 4 ounces of plain water, and patients must wait at least 30 minutes before eating, drinking, or taking other medications. This strict regimen is necessary to optimize absorption, as food and other beverages significantly reduce bioavailability. While this typically means morning administration for many patients, the critical factor is taking it before the first intake of the day, which may be at different times for shift workers.
The most common adverse effects associated with GLP-1 medications are gastrointestinal in nature, including nausea, vomiting, diarrhea, constipation, and abdominal discomfort. These side effects occur in approximately 10-40% of patients depending on the specific medication and dose, typically appearing during dose initiation or escalation. The timing of GLP-1 administration may influence the tolerability of these symptoms, though this has not been definitively established in clinical trials.
Morning administration may be preferable for patients who experience nausea, as they can manage symptoms during waking hours when they can employ coping strategies such as eating small, low-fat meals, staying hydrated, or using anti-nausea medications if prescribed. Additionally, morning dosing may provide coverage during daytime meals when carbohydrate intake is typically higher.
Conversely, evening or bedtime administration may benefit some patients who find that sleeping through the initial hours after injection helps them avoid or minimize awareness of nausea. Some patients report that taking their GLP-1 medication before bed allows them to sleep through the period when side effects might be most noticeable, waking with reduced symptoms.
The relationship between timing and side effects is not definitively established in clinical trials, as most studies do not systematically compare morning versus evening administration. Individual variation in gastric emptying, meal patterns, and physiological responses means that optimal timing is highly personalized. Patients should monitor their symptom patterns and discuss timing adjustments with their healthcare provider if side effects are limiting treatment adherence.
Gradual dose titration, as recommended in FDA labeling, remains the most evidence-based strategy for minimizing gastrointestinal adverse effects regardless of administration time. Patients should contact their healthcare provider if they experience persistent vomiting or diarrhea that could lead to dehydration or kidney problems, or if they develop severe abdominal pain.
Several patient-specific factors should guide the decision about when to administer GLP-1 medications. Lifestyle and daily routine are primary considerations. Patients with consistent morning routines may find it easier to remember daily injections before breakfast, while those with variable morning schedules might prefer evening dosing. Adherence to medication regimens is significantly improved when administration times align with established daily habits.
Meal patterns and eating schedules also influence optimal timing. For medications that must be taken before the first meal of the day, patients who practice intermittent fasting may need to adjust their medication schedule accordingly. Patients who experience appetite suppression as a therapeutic effect should consider whether morning or evening dosing better supports their nutritional goals and prevents excessive caloric restriction.
Work schedules and social commitments matter considerably. Healthcare workers, teachers, or others in demanding professions may prefer evening dosing to avoid managing potential side effects during work hours. Shift workers should follow label instructions regarding timing relative to meals rather than specific clock times—particularly for oral semaglutide, which should be taken before the first food or medication of the day regardless of when that occurs. Travel across time zones presents additional challenges, requiring advance planning with healthcare providers, especially for weekly medications where day-change rules apply.
Concurrent medications must be considered, particularly for oral semaglutide, which requires a 30-minute separation from other medications and food. Patients taking multiple morning medications, especially those requiring food intake, may find the strict requirements of oral semaglutide challenging. Injectable formulations offer more flexibility in this regard.
Medication combinations require special attention. Patients taking GLP-1 medications with insulin or sulfonylureas have an increased risk of hypoglycemia and should discuss timing of all medications with their healthcare provider to minimize this risk.
Individual side effect profiles vary considerably. Patients should track when symptoms occur relative to injection time and discuss patterns with their healthcare provider. These personalized adjustments, made in consultation with healthcare providers, can significantly improve treatment tolerability and long-term adherence.
Healthcare providers emphasize that consistency is more important than specific timing for most GLP-1 medications. The American Diabetes Association (ADA) Standards of Medical Care in Diabetes focus on adherence and individualization rather than prescribing universal timing rules. Providers typically recommend that patients choose a time they can reliably maintain, as missed doses or irregular administration can compromise glycemic control and weight management outcomes.
Clinical guidance suggests starting with manufacturer recommendations as outlined in FDA labeling, then adjusting based on individual response. For medications with flexible timing (liraglutide, weekly formulations), providers often suggest patients begin with the timing that best fits their schedule and monitor for side effects. If gastrointestinal symptoms are problematic, adjusting the timing may be considered, with reassessment after several weeks.
Providers also counsel patients on practical strategies to optimize GLP-1 therapy regardless of timing. These include setting phone alarms or using medication reminder apps, storing injectable pens properly (without attached needles and at recommended temperatures), and keeping a dosing log. For weekly medications, choosing a day that aligns with regular activities can improve adherence. Patients should never share pens or needles, even with family members.
When to contact healthcare providers is an essential part of timing discussions. Patients should reach out if they experience persistent nausea, vomiting, or diarrhea that prevents adequate nutrition or hydration (which may lead to dehydration and kidney problems); if they miss multiple doses due to timing challenges; or if they develop signs of more serious adverse effects such as severe abdominal pain (which may indicate pancreatitis), symptoms of gallbladder disease, visual changes, severe allergic reactions, or symptoms of thyroid nodules. Patients taking insulin or sulfonylureas with GLP-1 medications should be alert for hypoglycemia symptoms and contact their provider if these occur.
Ultimately, healthcare providers recognize that optimal GLP-1 timing is a collaborative decision. The goal is to maximize therapeutic benefits—improved glycemic control and weight management—while minimizing side effects and supporting long-term adherence. Patients should feel empowered to discuss timing preferences and challenges openly with their healthcare team, as personalized approaches yield the best clinical outcomes.
For most GLP-1 medications with flexible timing like liraglutide and weekly formulations, you can switch from morning to evening administration, but you should discuss this change with your healthcare provider first. The key is maintaining consistency once you establish a new time to ensure stable therapeutic effects and adherence.
Some patients report that evening or bedtime administration helps them sleep through the initial hours after injection when nausea might be most noticeable. However, this effect varies individually and has not been definitively established in clinical trials, so patients should monitor their own symptom patterns and discuss timing adjustments with their healthcare provider.
Missed dose guidance depends on your specific medication: for Ozempic, administer within 5 days of the missed dose; for Trulicity, administer if at least 3 days remain before the next scheduled dose; for Wegovy, administer if at least 2 days remain before the next dose. If you frequently miss doses due to timing challenges, contact your healthcare provider to develop a more sustainable schedule.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.