LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Do weight loss injections cause loose skin? This common concern arises as medications like semaglutide (Wegovy) and tirzepatide (Zepbound) gain widespread use for chronic weight management. These FDA-approved GLP-1 and dual GIP/GLP-1 receptor agonists do not directly cause loose skin through any pharmacological effect on dermal tissue. Instead, loose skin may develop as a consequence of the substantial weight reduction these medications enable. Understanding the indirect relationship between injectable weight loss treatments and skin changes helps patients set realistic expectations and implement strategies to optimize skin health during their weight management journey.
Quick Answer: Weight loss injections do not directly cause loose skin but may lead to it indirectly through the substantial weight reduction they enable.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Weight loss injections approved for chronic weight management include semaglutide (Wegovy) and tirzepatide (Zepbound). Semaglutide is a glucagon-like peptide-1 (GLP-1) receptor agonist, while tirzepatide is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications work by binding to receptors in the brain, pancreas, and gastrointestinal tract, leading to reduced appetite, increased satiety, delayed gastric emptying, and improved insulin secretion. The FDA has approved these medications specifically for chronic weight management in adults with a BMI ≥30 kg/m² (obesity) or ≥27 kg/m² (overweight) with at least one weight-related comorbidity such as hypertension, type 2 diabetes, or dyslipidemia. Ozempic (semaglutide) and Mounjaro (tirzepatide) are FDA-approved for type 2 diabetes management, not for weight loss.
Clinical trials demonstrate that patients using these injectable medications can achieve substantial weight loss. In the STEP-1 trial, semaglutide 2.4 mg produced average weight loss of approximately 15% of initial body weight over 68 weeks, while the SURMOUNT-1 trial showed tirzepatide achieved up to 22% weight loss over 72 weeks. This degree of weight reduction significantly exceeds what most patients achieve through lifestyle modifications alone. There is no evidence that these medications directly affect skin structure or elasticity; rather, they facilitate caloric deficit through appetite suppression and metabolic changes.
The relationship between weight loss injections and loose skin is indirect. These medications do not cause loose skin through any known pharmacological action on dermal tissue. Instead, loose skin may develop as a consequence of the rapid and substantial weight loss these treatments enable. The skin, which previously stretched to accommodate excess adipose tissue, may not contract proportionally as fat mass decreases. This phenomenon occurs with any significant weight loss method—whether achieved through bariatric surgery, intensive lifestyle intervention, or pharmacotherapy—and is not unique to injectable medications. The rate and magnitude of weight loss, rather than the method itself, primarily determine whether loose skin develops.
Skin elasticity—the ability of skin to stretch and return to its original shape—depends on multiple intrinsic and extrinsic factors that determine whether loose skin develops during weight loss. Age represents one of the most significant determinants, as collagen and elastin production decline progressively after age 30. Older adults losing substantial weight face higher risk of persistent skin laxity compared to younger individuals whose skin retains greater regenerative capacity.
The amount and rate of weight loss critically influence skin adaptation. Losing 100 pounds creates more excess skin than losing 30 pounds, and rapid weight loss (more than 1-2 pounds weekly, per CDC guidance) gives skin less time to adapt compared to gradual reduction. Patients using weight loss injections who lose 15-20% of body weight over 12-18 months may experience more pronounced skin changes than those losing weight more slowly. Duration of obesity also matters—skin stretched over many years undergoes structural changes that reduce its ability to contract, including decreased elastin fiber density and altered collagen architecture.
Genetic factors determine baseline skin quality, collagen composition, and elasticity. Some individuals naturally possess more resilient skin that adapts better to volume changes. Sun exposure and smoking damage collagen and elastin fibers, significantly impairing skin elasticity and recovery potential. Chronic ultraviolet radiation causes photoaging with collagen degradation, while smoking reduces blood flow to dermal tissues and impairs wound healing.
Nutritional status during weight loss affects skin health. Adequate protein intake (1.2-1.5 grams per kilogram body weight during weight loss, with potentially higher needs in older adults) supports collagen synthesis, while deficiencies in vitamin C, zinc, and copper may impair connective tissue repair. Hydration status may influence skin turgor and appearance, with the National Academies of Sciences, Engineering, and Medicine recommending approximately 3.7 liters total water daily for men and 2.7 liters for women (from all sources, including food). Patients with significant weight loss should maintain balanced nutrition primarily from food sources to optimize skin adaptation, though this cannot completely prevent loose skin when other risk factors predominate. Patients with kidney or heart disease should follow their healthcare provider's guidance regarding fluid intake.
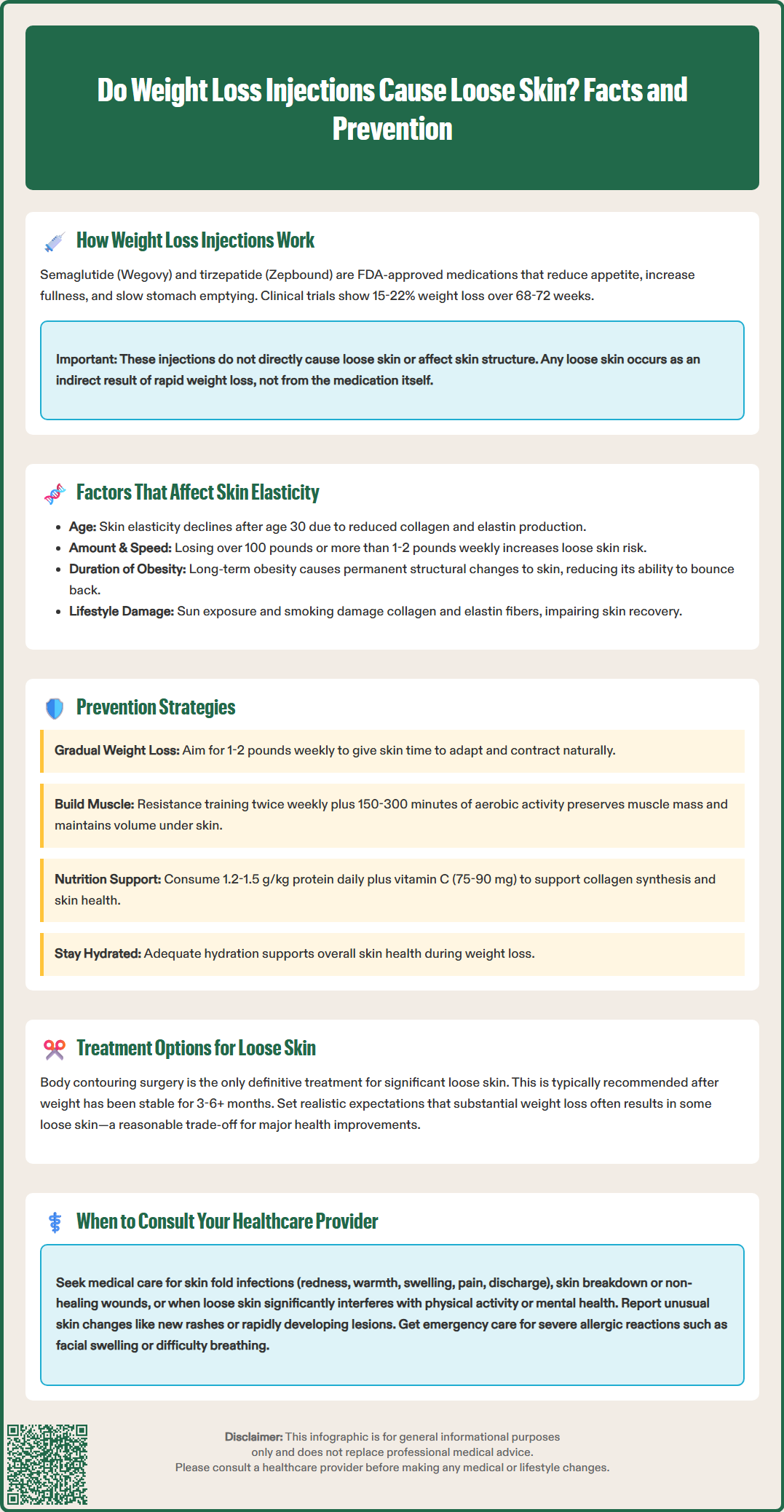
While weight loss injections themselves do not prevent loose skin, several strategies can optimize skin health during treatment and potentially minimize excess skin formation. Gradual weight loss represents the most evidence-based approach—aiming for 1-2 pounds weekly (per CDC recommendations) allows skin time to adapt as fat volume decreases. Healthcare providers titrate GLP-1 and GIP/GLP-1 medications primarily for tolerability and according to FDA-approved labeling, with any adjustments to influence weight loss rate requiring clinical supervision.
Resistance training and strength exercises during weight loss help preserve lean muscle mass, which maintains some volume beneath the skin and may reduce the appearance of laxity. The U.S. Department of Health and Human Services Physical Activity Guidelines recommend 150-300 minutes of moderate-intensity aerobic activity weekly plus muscle-strengthening activities at least twice weekly targeting all major muscle groups. Cardiovascular exercise improves circulation to skin tissues, potentially supporting collagen remodeling, though evidence specifically linking exercise to improved skin elasticity remains limited.
Optimizing nutrition includes ensuring adequate protein intake (1.2-1.5 g/kg for those losing weight), vitamin C (75-90 mg daily per NIH recommendations) for collagen synthesis, and appropriate hydration based on individual needs. Some patients consider collagen supplements, though clinical evidence supporting their efficacy for skin elasticity during weight loss is insufficient to make definitive recommendations. Prescription topical retinoids may modestly improve skin texture in limited areas but have minimal effect on significant skin laxity, are not appropriate for large body areas, and are contraindicated during pregnancy.
For patients who develop loose skin despite preventive measures, body contouring surgery (abdominoplasty, brachioplasty, thigh lift) remains the only definitive treatment for substantial excess skin. Most plastic surgeons recommend waiting until weight has been stable for several months (typically 3-6+ months) before considering surgical intervention. Non-surgical options including radiofrequency, ultrasound, and laser treatments show modest improvements in mild skin laxity but cannot address moderate to severe cases. Patients should maintain realistic expectations—significant weight loss often involves accepting some degree of loose skin as a trade-off for substantial health benefits including improved cardiometabolic risk factors.
Patients using weight loss injections should consult their healthcare provider if they experience specific skin changes that may indicate complications rather than expected laxity from fat loss. Skin infections can develop in areas where loose skin creates folds with persistent moisture, friction, and reduced air circulation. Warning signs include redness, warmth, swelling, pain, or discharge in skin folds—particularly in the abdominal pannus, under breasts, or in the groin. Urgent medical attention is needed for fever, chills, rapidly spreading redness, severe pain, or signs of systemic illness. Intertrigo (inflammatory condition in skin folds) and secondary bacterial or fungal infections require prompt medical evaluation and treatment with appropriate antimicrobials or antifungals.
Skin breakdown or ulceration in areas of loose skin represents a more serious concern requiring immediate attention. Chronic friction, moisture, and pressure can lead to skin maceration and wounds that heal poorly, particularly in patients with diabetes or peripheral vascular disease. Any non-healing wound, persistent irritation, or bleeding from skin folds warrants clinical assessment. Healthcare providers may recommend barrier creams, moisture-wicking garments, or referral to wound care specialists. Recurrent skin-fold infections or persistent ulcers may justify referral to dermatology, wound care, or plastic surgery.
Patients should also seek guidance when loose skin significantly impacts quality of life—interfering with physical activity, causing chronic discomfort, or affecting mental health. While loose skin itself is not medically dangerous, its psychological impact can be substantial. Healthcare providers can discuss realistic expectations, provide referrals to plastic surgeons for body contouring evaluation, or connect patients with support resources. Consultation is appropriate when weight has been stable for several months.
Unusual skin changes unrelated to expected laxity—including new rashes, significant color changes, or rapidly developing lesions—require evaluation to exclude dermatologic conditions or adverse medication effects. Though rare, GLP-1 and GIP/GLP-1 receptor agonists can cause injection site reactions or, very rarely, more serious skin manifestations. Seek immediate medical care for signs of severe allergic reactions such as facial swelling or difficulty breathing. Any concerning skin changes during weight loss treatment merit discussion with the prescribing provider to ensure appropriate diagnosis and management, distinguishing between expected consequences of weight loss and conditions requiring specific intervention.
While you cannot completely prevent loose skin, gradual weight loss of 1-2 pounds weekly, resistance training to preserve muscle mass, and adequate protein intake (1.2-1.5 g/kg) may help minimize its development. Body contouring surgery remains the only definitive treatment for substantial excess skin after weight stabilization.
The amount varies by individual, but losing more than 100 pounds creates higher risk than losing 30 pounds. Factors including age, duration of obesity, genetics, and rate of weight loss determine whether loose skin develops, not just the total amount lost.
Consult your healthcare provider if you develop skin infections in folds (redness, warmth, discharge), skin breakdown or ulceration, or if loose skin significantly impacts your quality of life or physical activity. Any non-healing wounds or unusual skin changes require prompt medical evaluation.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.