LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Do you have to stay on tirzepatide for life? This question concerns many patients prescribed Mounjaro or Zepbound for type 2 diabetes or chronic weight management. Tirzepatide is a dual GIP/GLP-1 receptor agonist that improves blood sugar control and promotes weight loss through multiple metabolic pathways. While the FDA does not mandate lifelong use, clinical evidence shows that type 2 diabetes and obesity are chronic conditions requiring ongoing management. Treatment duration depends on individual response, goals, tolerability, and the underlying disease being treated. Most patients need continued therapy to maintain benefits, though some may attempt supervised discontinuation after achieving significant metabolic improvements.
Quick Answer: Tirzepatide does not require lifelong use for all patients, but most individuals need ongoing therapy to maintain blood sugar control and weight loss benefits since type 2 diabetes and obesity are chronic conditions.
Tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and glucagon-like peptide-1 (GLP-1) receptor agonist approved by the FDA for type 2 diabetes management and chronic weight management. This injectable medication works by enhancing insulin secretion in response to meals, suppressing glucagon release, slowing gastric emptying, and reducing appetite through central nervous system pathways. These combined mechanisms lead to improved glycemic control and significant weight loss in clinical trials.
Importantly, tirzepatide carries a boxed warning for thyroid C-cell tumors and is contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN 2). It is not indicated for type 1 diabetes. For obesity management, Zepbound is specifically indicated for adults with a BMI ≥30 kg/m² or ≥27 kg/m² with at least one weight-related comorbidity.
The question of lifelong treatment with tirzepatide reflects a broader challenge in managing chronic metabolic conditions. Unlike acute infections that resolve with short-term antibiotics, type 2 diabetes and obesity are chronic diseases characterized by underlying metabolic dysfunction that typically persists even after initial treatment success. Current evidence suggests that tirzepatide addresses symptoms and metabolic abnormalities rather than curing the underlying disease process.
Clinical trials have demonstrated sustained efficacy during treatment periods extending to 72-88 weeks for obesity (SURMOUNT trials) and up to 104 weeks for diabetes (SURPASS-4), with participants maintaining glycemic improvements and weight loss while actively using the medication. However, there is no official FDA guidance mandating lifelong use, and treatment duration remains an individualized clinical decision. The American Diabetes Association (ADA) emphasizes that pharmacotherapy for diabetes and obesity often requires long-term or indefinite continuation to maintain benefits, though this does not necessarily mean every patient must remain on the same medication permanently. Treatment plans should balance efficacy, tolerability, safety, cost, and patient preferences while recognizing that metabolic diseases generally require ongoing management strategies.
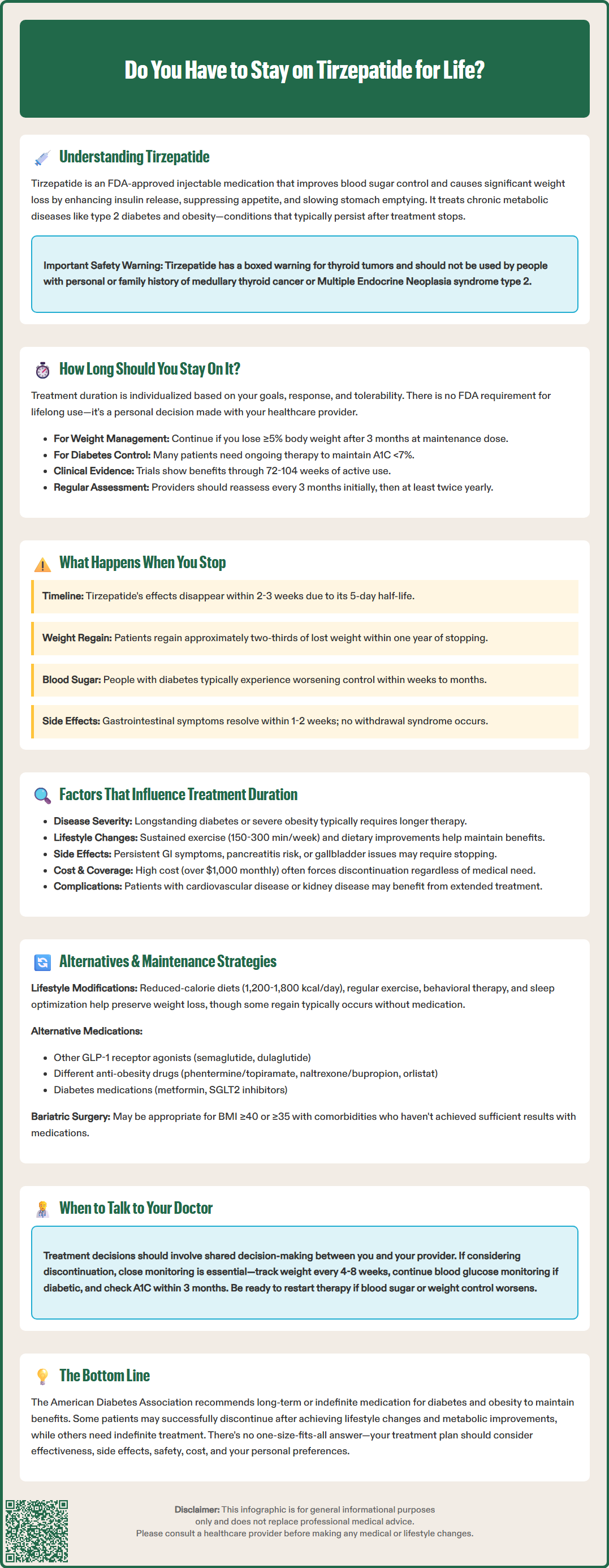
The optimal duration of tirzepatide therapy varies considerably among individuals and depends on treatment goals, response, tolerability, and the underlying condition being treated. For type 2 diabetes management, treatment duration is typically guided by glycemic control targets, with many patients requiring ongoing therapy to maintain A1C levels below 7% (or individualized targets). The ADA guidelines recommend continuing effective glucose-lowering medications as long as they remain beneficial and well-tolerated, with reassessment approximately every 3 months until glycemic targets are achieved, then at least twice yearly.
For chronic weight management, the FDA-approved indication for Zepbound (tirzepatide for obesity) does not specify a maximum treatment duration. US obesity treatment guidelines recommend continuing anti-obesity medications if patients achieve ≥5% weight loss after approximately 3 months at the maintenance dose; if this threshold is not met, discontinuation or switching to an alternative medication should be considered. Clinical evidence from the SURMOUNT trials demonstrated continued weight loss and maintenance through 72 weeks of treatment, with participants who discontinued therapy experiencing significant weight regain.
Clinicians typically assess treatment continuation at regular intervals, evaluating several factors: achievement of therapeutic goals (A1C reduction of 0.5-1% or weight loss of 5-15% or more), absence of intolerable adverse effects, patient adherence and satisfaction, and cost-effectiveness. Some patients may achieve sufficient lifestyle modifications and metabolic improvements to attempt medication discontinuation under medical supervision, while others may require indefinite therapy to maintain benefits.
Referral to specialists should be considered when patients have persistent A1C elevations despite combination therapy, complex obesity requiring specialized care, or when evaluating bariatric surgery options (typically for BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities).
The decision to continue or discontinue tirzepatide should involve shared decision-making between patient and healthcare provider, considering individual circumstances rather than following a universal timeline. Patients who achieve target goals and wish to attempt discontinuation should do so under close monitoring, recognizing that resumption of therapy may become necessary if metabolic parameters deteriorate. Unlike some medications, tirzepatide does not require tapering when discontinuing.
Discontinuation of tirzepatide typically results in reversal of many therapeutic benefits, as the medication's pharmacological effects cease once it is eliminated from the body. Tirzepatide has a half-life of approximately five days, meaning drug levels decline substantially within two to three weeks after the last injection. As medication effects wane, the underlying metabolic dysfunction that was being managed pharmacologically re-emerges.
Clinical trial data consistently demonstrate weight regain following tirzepatide discontinuation. In the SURMOUNT-4 trial published in the New England Journal of Medicine, participants who switched from tirzepatide to placebo regained approximately two-thirds of their lost weight over the subsequent 52 weeks, while those continuing treatment maintained their weight loss and achieved additional reductions. This rebound effect reflects the return of increased appetite, normalization of gastric emptying, and loss of the medication's metabolic benefits rather than any unique withdrawal phenomenon.
For patients with type 2 diabetes, stopping tirzepatide often leads to deterioration in glycemic control within weeks to months. A1C levels typically rise as insulin secretion decreases and glucagon suppression is lost. The rate and extent of glycemic deterioration depend on individual factors including baseline diabetes severity, beta-cell function, insulin resistance, and adherence to lifestyle modifications. Some patients may maintain acceptable control through diet, exercise, and other medications, while others experience rapid decompensation requiring treatment intensification.
Adverse effects associated with tirzepatide—primarily gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation—generally resolve within one to two weeks after discontinuation as drug levels decline. There is no evidence of a specific withdrawal syndrome, though patients may notice increased hunger and changes in satiety signals as the medication's appetite-suppressing effects dissipate.
After discontinuation, close monitoring is essential: weight should be checked every 4-8 weeks initially, and for diabetes patients, self-monitoring of blood glucose or continuous glucose monitoring should continue as indicated, with A1C assessment within approximately 3 months of stopping to detect metabolic deterioration early and implement alternative management strategies.
Multiple clinical, metabolic, and practical factors influence how long an individual should remain on tirzepatide therapy. Disease severity and duration play crucial roles—patients with longstanding type 2 diabetes, significant beta-cell dysfunction, or severe obesity typically require longer treatment durations than those with early-stage disease or modest metabolic abnormalities. Individuals who achieve remission criteria for type 2 diabetes (A1C <6.5% off medication for three months or longer) may be candidates for supervised discontinuation attempts, though this remains uncommon.
Lifestyle modification success significantly impacts treatment duration decisions. Patients who implement and sustain meaningful dietary changes, regular physical activity (150-300 minutes weekly of moderate-intensity exercise per US Physical Activity Guidelines), and behavioral modifications may maintain some benefits after medication discontinuation, whereas those unable to adopt lifestyle changes typically experience rapid relapse. The degree of weight loss achieved also matters—greater weight reduction (15% or more) may provide more durable metabolic improvements that partially persist after stopping medication.
Tolerability and safety considerations influence continuation decisions. While most gastrointestinal side effects improve over time, some patients experience persistent symptoms that affect quality of life. Safety concerns requiring monitoring include pancreatitis risk, gallbladder disease, and thyroid issues (patients should report symptoms like severe abdominal pain or neck mass/hoarseness). Tirzepatide is contraindicated in patients with personal/family history of MTC or MEN 2. Patients taking oral contraceptives should use backup contraception for 4 weeks after initiation and each dose increase due to potential reduced efficacy.
Cost and access considerations represent practical limitations for many patients. Tirzepatide's list price exceeds $1,000 monthly without insurance coverage, though actual costs vary by pharmacy and insurance. Insurance formulary changes, prior authorization denials, or financial hardship may force discontinuation regardless of clinical appropriateness. Some patients cycle on and off medication based on affordability rather than medical indication.
Comorbidity management affects duration decisions. Patients with cardiovascular disease, chronic kidney disease, or other obesity-related complications may benefit from extended treatment, though cardiovascular and renal outcome trials with tirzepatide are still ongoing, and definitive risk reduction benefits remain under investigation. Individual risk-benefit assessment should guide these decisions in consultation with specialists when appropriate.
For patients discontinuing tirzepatide, several strategies can help maintain achieved benefits and manage underlying metabolic conditions. Lifestyle interventions form the foundation of any maintenance plan. Continued adherence to reduced-calorie diets (typically 1,200-1,800 kcal/day depending on individual needs), regular physical activity (150-300 minutes weekly of moderate-intensity exercise), behavioral therapy, and sleep optimization can help preserve weight loss and glycemic improvements, though most patients regain some weight without pharmacological support.
Alternative pharmacotherapy options include other GLP-1 receptor agonists such as semaglutide (Ozempic, Wegovy) or dulaglutide (Trulicity), which share similar mechanisms and may be more affordable or accessible. Other FDA-approved anti-obesity medications include phentermine/topiramate ER (Qsymia), naltrexone/bupropion (Contrave), and orlistat (Xenical, Alli), each with different mechanisms, efficacy profiles, and side effects. For type 2 diabetes, transitioning to metformin, SGLT2 inhibitors, or other agents may provide adequate glycemic control in some patients, though typically with less weight loss benefit. Note that combining GLP-1/GIP receptor agonists with DPP-4 inhibitors is not recommended due to overlapping mechanisms.
Bariatric surgery should be considered for eligible patients (typically BMI ≥40 kg/m² or ≥35 kg/m² with comorbidities) who have not achieved or maintained sufficient weight loss with medications and lifestyle interventions. Surgical approaches often provide more durable metabolic improvements than pharmacotherapy alone.
Structured maintenance programs incorporating regular monitoring, accountability, and support improve outcomes after medication discontinuation. These may include frequent follow-up visits, continuous glucose monitoring for diabetes patients, regular weight checks, dietitian consultations, and participation in weight management support groups. Early detection of metabolic deterioration allows for timely intervention before significant regain occurs.
Intermittent or reduced-dose strategies lack robust clinical trial support and may result in partial benefit loss. Some clinicians attempt dose reduction to the lowest effective level, but this approach should be undertaken only under medical supervision with appropriate monitoring of A1C, weight, and metabolic parameters. Resumption of full-dose therapy remains an option if alternative strategies prove insufficient to maintain therapeutic goals.
Most patients experience weight regain and worsening blood sugar control within weeks to months after stopping tirzepatide. Clinical trials show patients who discontinue treatment regain approximately two-thirds of lost weight over the following year, while A1C levels typically rise as the medication's metabolic effects cease.
Some patients may attempt supervised discontinuation after achieving significant metabolic improvements and implementing sustainable lifestyle changes. This decision should be made with your healthcare provider and requires close monitoring of weight and blood sugar levels to detect any deterioration early.
Clinical trials demonstrate sustained efficacy for 72-88 weeks in obesity management and up to 104 weeks for type 2 diabetes. Participants maintained glycemic improvements and weight loss while actively using the medication, though there is no FDA-mandated maximum treatment duration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.