LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible

Does GLP-1 cause back pain? This question concerns many patients starting glucagon-like peptide-1 (GLP-1) receptor agonists like semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), or liraglutide (Victoza, Saxenda) for type 2 diabetes or weight management. While these medications commonly cause gastrointestinal side effects such as nausea and constipation, back pain is not listed as a characteristic adverse effect in FDA prescribing information. However, some patients report musculoskeletal discomfort during treatment. Understanding whether this represents a direct medication effect, an indirect consequence of therapy, or coincidental occurrence is essential for appropriate clinical management and informed decision-making.
Quick Answer: Back pain is not a recognized direct side effect of GLP-1 receptor agonists according to FDA prescribing information and clinical trial data.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications increasingly prescribed for type 2 diabetes management and, more recently, for chronic weight management. These agents include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), while tirzepatide (Mounjaro, Zepbound) is a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist. These medications work by mimicking the action of naturally occurring incretin hormones, which enhances glucose-dependent insulin secretion, suppresses glucagon release, slows gastric emptying, and promotes satiety through central nervous system pathways.
The most commonly reported adverse effects of GLP-1-based therapies are gastrointestinal in nature. According to FDA prescribing information, these include nausea (occurring in 15–44% of patients depending on the agent and dose), vomiting, diarrhea, constipation, and abdominal pain. These effects typically emerge during dose escalation and often diminish over several weeks as physiologic adaptation occurs. The gastrointestinal side effects result primarily from delayed gastric emptying and altered gut motility.
Other recognized adverse effects include injection site reactions, fatigue, headache, and dizziness. More serious risks include pancreatitis, gallbladder disease, and potential thyroid C-cell tumors (observed in rodent studies). Importantly, these medications carry a boxed warning and contraindication for patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Additional safety concerns include hypoglycemia risk when used with insulin or insulin secretagogues, potential acute kidney injury with dehydration, and with semaglutide, worsening of diabetic retinopathy in patients with pre-existing retinopathy.
The American Diabetes Association guidelines emphasize the importance of patient education regarding expected side effects and appropriate monitoring during therapy initiation and titration.
Understanding the established adverse effect profile provides essential context when evaluating less commonly reported symptoms, such as back pain, that patients may experience during treatment.
Back pain is not listed as a common or characteristic adverse effect in the FDA-approved prescribing information for GLP-1 receptor agonists or the dual GIP/GLP-1 agonist tirzepatide. Clinical trials that led to regulatory approval did not identify back pain as occurring at significantly higher rates in treatment groups compared to placebo. However, this does not definitively exclude the possibility that some patients may experience back pain during therapy.
In post-marketing surveillance and clinical practice, some patients have reported musculoskeletal symptoms, including back pain, while taking these medications. The challenge in establishing causality lies in distinguishing medication-related effects from coincidental occurrences. Back pain is extremely prevalent in the general population—the Global Burden of Disease Study estimates that low back pain affects approximately 540 million people worldwide at any given time. Among adults with type 2 diabetes and obesity (the primary populations receiving GLP-1-based therapy), baseline rates of back pain are particularly high due to biomechanical factors, inflammatory processes, and comorbid conditions.
There is no established pharmacologic mechanism by which GLP-1 receptor agonism would directly cause musculoskeletal pain. Unlike some medication classes with known musculoskeletal toxicity (such as fluoroquinolone antibiotics or statins), GLP-1-based medications do not have documented effects on muscle, bone, or connective tissue that would predictably result in back pain.
Current evidence suggests that if back pain occurs during treatment, it is more likely coincidental or related to indirect factors rather than a direct pharmacologic effect of the medication. Nonetheless, any new or worsening symptom during treatment warrants clinical evaluation to determine appropriate management.
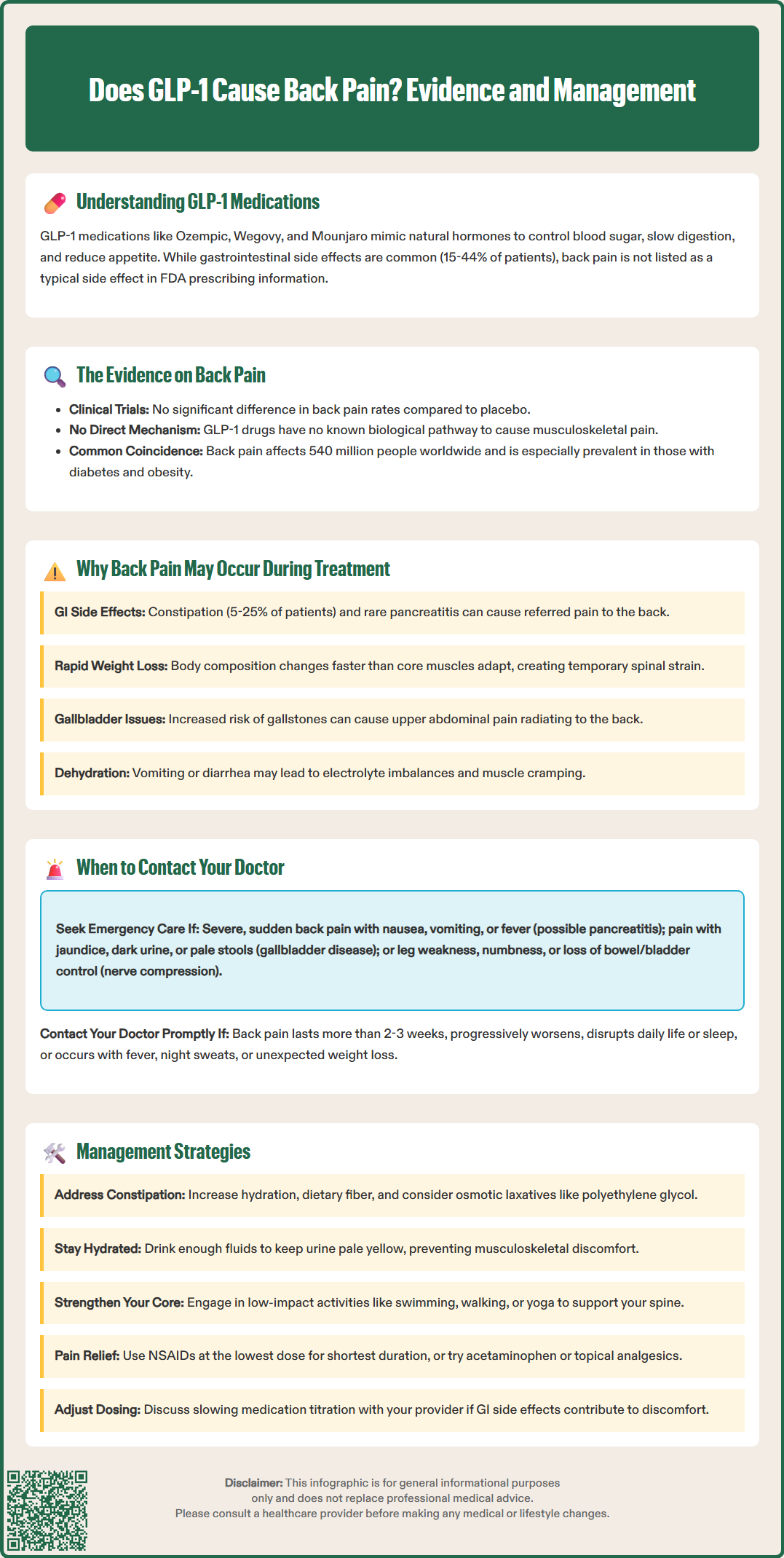
While GLP-1-based medications do not directly cause back pain through their primary mechanism of action, several indirect factors may contribute to musculoskeletal discomfort during treatment. Understanding these potential contributors helps clinicians and patients contextualize symptoms appropriately.
Gastrointestinal effects and referred pain: The pronounced gastrointestinal side effects of GLP-1 therapy—particularly nausea, constipation, and abdominal distension—can occasionally manifest as referred pain to the back. Constipation, which occurs in approximately 5–25% of patients depending on the specific product and dose, may cause lower back discomfort. Additionally, pancreatitis, though rare, typically presents with severe epigastric pain radiating to the back and requires immediate medical evaluation.
Rapid weight loss and biomechanical changes: Patients achieving significant weight reduction may experience temporary musculoskeletal adjustment. Based on observations from bariatric surgery literature, rapid loss of adipose tissue alters body mechanics, weight distribution, and postural alignment. Core muscle strength may not immediately adapt to the changing body composition, potentially resulting in increased mechanical stress on the lumbar spine. While this mechanism is hypothetical for pharmacologically induced weight loss, it represents a plausible explanation for some patients' experiences.
Gallbladder disease: GLP-1-based medications, particularly those approved for weight management, carry an increased risk of gallbladder disease, including gallstones and cholecystitis. FDA labels specifically warn about this risk. Gallbladder pain can present as right upper quadrant or epigastric pain that radiates to the back.
Dehydration and electrolyte disturbances: Gastrointestinal side effects, particularly vomiting and diarrhea, can lead to dehydration and electrolyte imbalances. Severe dehydration may lead to acute kidney injury, which can present with flank or back pain. Dehydration may also contribute to muscle cramping and generalized musculoskeletal discomfort.
Increased physical activity: Patients experiencing improved glycemic control and weight loss often increase their physical activity levels. Unaccustomed exercise or improper technique may result in musculoskeletal strain, including back pain, which is temporally associated with but not caused by the medication itself.
While most back pain during GLP-1-based therapy is likely unrelated to the medication and may resolve with conservative management, certain presentations warrant prompt medical evaluation. Patients should be educated to recognize warning signs that require clinical assessment.
Seek emergency medical care immediately (call 911 or go to the emergency department) if back pain is:
Severe and sudden in onset, particularly if accompanied by nausea, vomiting, or fever—this may indicate pancreatitis, which requires urgent evaluation. Pancreatitis-related pain is typically intense, constant, located in the upper abdomen radiating to the back, and worsens after eating.
Associated with right upper quadrant abdominal pain, especially if accompanied by jaundice, dark urine, or pale stools—these symptoms may suggest gallbladder disease (cholecystitis or cholelithiasis), which occurs at increased rates with GLP-1 therapy.
Accompanied by neurologic symptoms such as leg weakness, numbness, bowel or bladder dysfunction, or saddle anesthesia—these are red flags for cauda equina syndrome or severe nerve compression requiring emergency evaluation.
Contact your healthcare provider promptly if:
Back pain persists beyond 2–3 weeks despite conservative measures
Pain progressively worsens rather than improving
Pain significantly interferes with daily activities or sleep
Systemic symptoms develop (fever, night sweats) or unintentional weight loss beyond therapy goals
Pain occurs in patients with cancer history or other risk factors for metastatic disease
Flank pain accompanied by urinary symptoms (possible kidney stones or infection)
Clinicians should obtain a thorough history, perform physical examination, and consider laboratory evaluation (including serum lipase and liver function tests) when indicated. Imaging studies may be warranted based on clinical presentation and risk stratification, following American College of Physicians guidelines (avoiding routine imaging without red flags). The decision to continue, adjust, or discontinue therapy should be individualized based on the underlying cause of back pain and the overall benefit-risk assessment.
For patients experiencing non-emergent back pain during GLP-1-based therapy, a systematic approach to management can often provide relief while allowing continuation of beneficial metabolic treatment.
Conservative management strategies include:
Optimize gastrointestinal function: Address constipation proactively with adequate hydration (individualized to the patient's cardiovascular and renal status), dietary fiber supplementation, and when necessary, osmotic laxatives such as polyethylene glycol. Improved bowel function may alleviate referred back discomfort.
Maintain proper hydration and nutrition: Ensure adequate fluid intake, particularly if experiencing nausea or reduced appetite. Aim for pale yellow urine as a practical guide to hydration status. Dehydration can exacerbate musculoskeletal discomfort and potentially lead to kidney problems. Small, frequent meals may help manage gastrointestinal symptoms while maintaining nutritional adequacy.
Physical therapy and exercise modification: Engage in core strengthening exercises under professional guidance to support the spine during body composition changes. Low-impact activities such as swimming, walking, or yoga may be better tolerated than high-impact exercise during the adjustment period. Physical therapy evaluation can identify biomechanical issues and provide targeted interventions.
Pharmacologic pain management: In accordance with American College of Physicians guidelines, non-steroidal anti-inflammatory drugs (NSAIDs) may be considered first-line when appropriate, using the lowest effective dose for the shortest duration. NSAIDs should be used cautiously in patients with renal impairment, cardiovascular disease, or gastrointestinal risk factors. Acetaminophen has limited efficacy for low back pain but may be appropriate for some patients (up to 3,000 mg daily in divided doses for adults without liver disease). Topical analgesics such as diclofenac gel or lidocaine patches may offer localized relief without significant systemic effects.
Medication adjustment: If gastrointestinal side effects are contributing to back discomfort, discuss with your healthcare provider about slowing the titration schedule or temporarily holding at a lower dose until adaptation occurs.
Postural awareness and ergonomics: Evaluate workplace ergonomics, sleeping surface quality, and daily postural habits. Simple modifications can significantly reduce mechanical back strain.
If back pain persists despite conservative measures or significantly impacts quality of life, clinicians should reassess the benefit-risk ratio of continuing therapy. In most cases, however, back pain during GLP-1-based treatment is manageable and does not necessitate medication discontinuation. Collaborative decision-making between patient and clinician, informed by thorough evaluation and individualized risk assessment, guides optimal management.
No, back pain is not listed as a common or characteristic side effect in FDA prescribing information for GLP-1 receptor agonists. Clinical trials did not identify back pain occurring at significantly higher rates compared to placebo.
Seek emergency medical care immediately if you experience severe, sudden back pain with nausea and vomiting, as this may indicate pancreatitis. Also seek urgent evaluation for back pain with right upper quadrant abdominal pain, which may suggest gallbladder disease.
Rapid weight loss may contribute to temporary musculoskeletal adjustment as body mechanics and postural alignment change. Core muscle strength may not immediately adapt to changing body composition, potentially causing increased mechanical stress on the lumbar spine, though this mechanism remains hypothetical for pharmacologic weight loss.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.