LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 cause colon cancer? This question has emerged as glucagon-like peptide-1 (GLP-1) receptor agonists—including semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), and dulaglutide (Trulicity)—have become widely prescribed for type 2 diabetes and weight management. While these medications produce gastrointestinal effects that have raised theoretical concerns, current evidence does not establish a causal link between GLP-1 drugs and colorectal cancer. Large clinical trials, population studies, and FDA surveillance have not identified colon cancer as a confirmed risk. Understanding the distinction between proven side effects and unsubstantiated concerns helps patients and clinicians make informed treatment decisions based on the best available evidence.
Quick Answer: Current evidence does not establish that GLP-1 receptor agonists cause colon cancer in humans.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications originally developed for type 2 diabetes management. Some of these medications are also FDA-approved for chronic weight management. These drugs include semaglutide (Ozempic for diabetes, Wegovy for weight management), liraglutide (Victoza for diabetes, Saxenda for weight management), dulaglutide (Trulicity for diabetes only), and tirzepatide (Mounjaro for diabetes, Zepbound for weight management)—with tirzepatide being a dual glucose-dependent insulinotropic polypeptide (GIP) and GLP-1 receptor agonist, not solely a GLP-1 agonist.
As these medications have gained popularity, questions about potential cancer risks have emerged in both medical literature and public discourse. Concerns about colon cancer specifically have surfaced due to the theoretical consideration that GLP-1 receptors are present in various tissues, potentially including parts of the gastrointestinal tract. These receptors may play roles in gut motility, inflammation modulation, and cellular processes—functions that could hypothetically relate to cancer development.
It is important to distinguish between theoretical concerns based on mechanism of action and actual clinical evidence of harm. The gastrointestinal effects of GLP-1 agonists—including delayed gastric emptying and altered bowel transit time—have raised questions about whether chronic exposure might influence colorectal cancer risk. However, the presence of drug receptors in tissue does not automatically indicate cancer risk.
Currently, there is no established causal link between GLP-1 receptor agonists and colon cancer in humans. Regulatory agencies including the FDA continue to monitor safety data from clinical trials and post-marketing surveillance. Understanding the distinction between ongoing scientific investigation and confirmed risk is essential for patients and clinicians making informed treatment decisions.
The scientific literature examining GLP-1 receptor agonists and colorectal cancer risk presents a complex and evolving picture. Several large observational studies and meta-analyses have investigated this relationship, with generally reassuring findings.
A systematic review and meta-analysis published in Diabetes, Obesity and Metabolism examined cardiovascular outcome trials involving over 60,000 patients treated with GLP-1 receptor agonists. The analysis found no increased incidence of gastrointestinal cancers, including colorectal cancer, compared to placebo or standard care. The follow-up periods in these trials typically ranged from 1.5 to 5 years, providing medium-term safety data.
Population-based cohort studies from Scandinavian registries have similarly found no association between GLP-1 agonist use and increased colorectal cancer risk. A study using Swedish and Danish national databases compared cancer incidence in over 20,000 GLP-1 users versus other diabetes medications and found no elevated risk for colon or rectal cancers during follow-up periods extending beyond three years.
Some preclinical laboratory research has suggested potential anti-inflammatory effects. Studies in cell cultures and animal models indicate that GLP-1 receptor activation might reduce inflammation and oxidative stress in colonic tissue—factors implicated in cancer development. However, these findings are preliminary and hypothesis-generating rather than evidence of protective effects in humans.
Important limitations exist in current research. Most studies have relatively short follow-up periods given that cancer development typically occurs over many years. Additionally, patients receiving GLP-1 medications often have metabolic conditions that independently affect cancer risk, making it challenging to isolate drug effects. Ongoing long-term surveillance studies will provide more definitive answers as data mature.
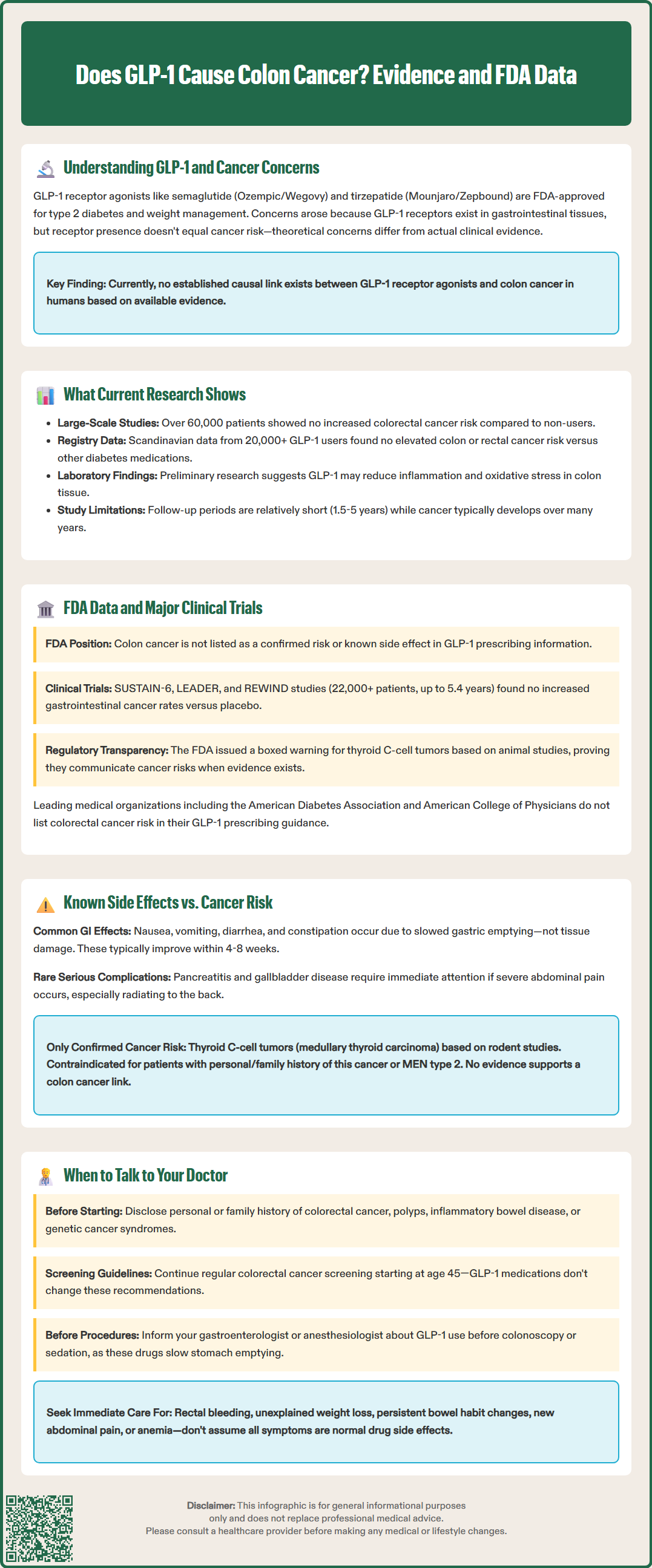
The FDA's evaluation of GLP-1 receptor agonists has not identified colon cancer as a confirmed risk associated with this drug class. Prescribing information for approved GLP-1 medications does not list colorectal cancer as a known adverse effect, though the FDA requires ongoing post-marketing surveillance for all novel therapeutic agents.
The landmark cardiovascular outcome trials that led to expanded indications for several GLP-1 drugs provide the most robust safety data available. The SUSTAIN-6 trial for semaglutide (3,297 patients, median 2.1 years), LEADER trial for liraglutide (9,340 patients, median 3.8 years), and REWIND trial for dulaglutide (9,901 patients, median 5.4 years) all included comprehensive adverse event monitoring. None demonstrated increased rates of gastrointestinal malignancies compared to placebo.
The FDA Adverse Event Reporting System (FAERS) collects post-marketing safety reports, but such spontaneous reporting systems have inherent limitations and cannot establish causation or absence of risk. To date, no FDA safety communication has identified colorectal cancer as a safety signal for GLP-1 receptor agonists.
Importantly, the FDA has identified and communicated other potential cancer concerns with this drug class. A boxed warning exists for thyroid C-cell tumors (medullary thyroid carcinoma) based on rodent studies, though no conclusive increase in human cases has been established. This demonstrates the agency's willingness to highlight cancer risks when evidence warrants concern.
The American Diabetes Association's Standards of Medical Care in Diabetes does not list colorectal cancer risk as a consideration when prescribing GLP-1 receptor agonists. Similarly, the American College of Physicians' guidance on type 2 diabetes management does not identify colon cancer as a contraindication or precaution for GLP-1 use. These professional society positions reflect the current evidence base showing no established link between these medications and colorectal malignancy.
GLP-1 receptor agonists have a well-characterized side effect profile that differs substantially from cancer risk. Understanding the distinction between common, expected adverse effects and unproven long-term concerns helps contextualize patient experiences and clinical decision-making.
Common gastrointestinal side effects occur in many patients and include:
Nausea (most common, typically improving after 4-8 weeks)
Vomiting
Diarrhea
Constipation
Abdominal pain or discomfort
Decreased appetite
These effects result from the drugs' mechanism of action—slowing gastric emptying and affecting gut motility—rather than indicating tissue damage or malignancy. Most gastrointestinal symptoms are dose-dependent and improve with gradual titration or dose reduction.
Serious but rare gastrointestinal complications that require medical attention include:
Pancreatitis (rare but requires immediate medical attention)
Gallbladder disease including cholecystitis (risk may be increased with rapid weight loss)
Severe delayed gastric emptying
Intestinal obstruction or ileus (FDA labels for semaglutide include postmarketing reports of ileus)
These conditions require prompt evaluation but are not cancer-related. Persistent or severe abdominal pain, especially if radiating to the back, warrants immediate medical assessment to exclude pancreatitis.
The confirmed cancer concern with GLP-1 agonists involves thyroid C-cell tumors, based on rodent studies showing medullary thyroid carcinoma at high drug exposures. This risk appears specific to thyroid tissue. Patients with personal or family history of medullary thyroid carcinoma or Multiple Endocrine Neoplasia syndrome type 2 should not receive GLP-1 agonists.
No similar mechanistic concern or animal data supports a colon cancer link. The gastrointestinal symptoms patients experience reflect the drugs' intended pharmacological effects on gut hormone signaling rather than cellular transformation or malignant changes.
Hypoglycemia risk is increased when GLP-1 medications are combined with insulin or sulfonylureas, requiring dose adjustments of these other medications.
Open communication with healthcare providers about cancer history remains essential when considering any new medication, including GLP-1 receptor agonists. While current evidence does not support a colon cancer link, certain clinical scenarios warrant specific discussion.
Patients should inform their physician if they have:
Personal history of any cancer, including colorectal cancer or polyps
Family history of colorectal cancer, especially in first-degree relatives
Inflammatory bowel disease (Crohn's disease or ulcerative colitis)
Genetic syndromes associated with increased cancer risk (Lynch syndrome, familial adenomatous polyposis)
Previous radiation therapy to the abdomen or pelvis
These factors affect baseline colorectal cancer risk independent of medication use. Patients with personal history of colon cancer can generally receive GLP-1 agonists if otherwise appropriate, as no evidence suggests these drugs increase recurrence risk. However, individualized assessment is necessary, and coordination with the oncology team is advisable for patients with active or recent cancer.
Absolute contraindications to GLP-1 receptor agonists include:
Personal or family history of medullary thyroid carcinoma
Multiple Endocrine Neoplasia syndrome type 2
Previous serious hypersensitivity reaction to the specific GLP-1 drug
Pregnancy and breastfeeding (for medications approved for weight management: Wegovy, Saxenda, and Zepbound)
Patients should maintain age-appropriate cancer screening regardless of GLP-1 use. For colorectal cancer, current US Preventive Services Task Force guidelines recommend screening beginning at age 45 for average-risk individuals, using colonoscopy, stool-based tests, or other approved methods. GLP-1 therapy does not change these screening recommendations.
Patients scheduled for colonoscopy or other procedures requiring sedation should follow their gastroenterologist's or anesthesiologist's instructions regarding whether to hold GLP-1 medications before the procedure, as delayed gastric emptying may affect sedation safety.
Warning signs requiring prompt evaluation include:
Rectal bleeding or blood in stool
Unexplained weight loss (beyond expected medication effect)
Persistent change in bowel habits lasting more than a few weeks
New-onset abdominal pain that differs from typical GLP-1 side effects
Iron-deficiency anemia
These symptoms warrant investigation regardless of medication use, as they may indicate various gastrointestinal conditions requiring diagnosis. Patients should not attribute all abdominal symptoms to expected drug side effects without medical evaluation, particularly if symptoms are severe, persistent, or accompanied by alarm features. Shared decision-making between patients and clinicians, incorporating individual risk factors and preferences, remains the foundation of appropriate GLP-1 prescribing.
No, current evidence from large clinical trials and population studies does not show a link between GLP-1 receptor agonists and colon cancer. The FDA has not identified colorectal cancer as a confirmed risk for this medication class.
GLP-1 medications carry a boxed warning for thyroid C-cell tumors (medullary thyroid carcinoma) based on rodent studies, though no conclusive increase in human cases has been established. Patients with personal or family history of medullary thyroid carcinoma should not use these drugs.
Yes, standard colorectal cancer screening recommendations remain unchanged for patients taking GLP-1 medications. The US Preventive Services Task Force recommends screening beginning at age 45 for average-risk individuals, regardless of GLP-1 use.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.