LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 cause night sweats? Many patients starting GLP-1 medications like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) wonder about this symptom. Night sweats are not listed as a recognized side effect in FDA prescribing information for GLP-1 receptor agonists. Clinical trials have not established a direct link between these diabetes and weight management medications and nocturnal hyperhidrosis. If you experience night sweats while taking GLP-1 therapy, other medical causes should be investigated, including hypoglycemia, infections, hormonal changes, or medication interactions. Understanding the actual side effect profile of GLP-1 medications helps patients and providers distinguish between drug-related symptoms and unrelated medical conditions requiring separate evaluation.
Quick Answer: Night sweats are not a recognized side effect of GLP-1 medications according to FDA prescribing information and clinical trial data.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications primarily used to manage type 2 diabetes and, more recently, for chronic weight management. These medications include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda). Tirzepatide (Mounjaro, Zepbound) is a related but distinct medication that acts as a dual GIP/GLP-1 receptor agonist. These incretin-based therapies have gained significant attention due to their effectiveness in lowering blood glucose levels and promoting weight loss.
GLP-1 medications work by mimicking the action of naturally occurring GLP-1, a hormone released by the intestines after eating. These drugs bind to GLP-1 receptors throughout the body, triggering several beneficial effects. They stimulate insulin secretion from the pancreas in a glucose-dependent manner, meaning they promote insulin release only when blood sugar levels are elevated, which reduces the risk of hypoglycemia. Additionally, they suppress glucagon secretion, a hormone that raises blood glucose levels.
Beyond glucose regulation, GLP-1 receptor agonists slow gastric emptying, which helps people feel fuller for longer periods and reduces appetite through effects on brain centers that control hunger. This mechanism contributes to their weight loss benefits. The medications are typically administered via subcutaneous injection, with dosing frequencies ranging from daily to once weekly depending on the specific formulation. Oral semaglutide (Rybelsus) is also available.
Understanding how these medications work throughout the body is important when considering potential side effects, as GLP-1 receptors are present in multiple organ systems beyond the pancreas, including the gastrointestinal tract, cardiovascular system, and central nervous system. It's important to note that these medications carry a boxed warning for risk of thyroid C-cell tumors and are contraindicated in patients with a personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2).
The most frequently reported side effects of GLP-1 medications are gastrointestinal in nature, reflecting the drugs' effects on the digestive system. According to FDA prescribing information and clinical trial data, nausea is the most common adverse effect, occurring in 15-44% of patients depending on the specific medication and dose. Other common gastrointestinal effects include:
Vomiting (5-24% of patients)
Diarrhea (8-30% of patients)
Constipation (10-24% of patients)
Abdominal pain or discomfort (5-20% of patients)
These side effects are typically most pronounced when initiating therapy or increasing doses, and often diminish over time as the body adjusts to the medication. Healthcare providers usually recommend gradual dose escalation to minimize gastrointestinal symptoms.
Other documented side effects include injection site reactions (redness, itching, or swelling), fatigue, dizziness, headache, and increased heart rate. More serious adverse effects include pancreatitis, gallbladder disease (cholelithiasis, cholecystitis), and acute kidney injury (particularly with severe dehydration from gastrointestinal symptoms). Semaglutide has been associated with diabetic retinopathy complications in some patients with pre-existing retinopathy.
All GLP-1 receptor agonists and tirzepatide carry a boxed warning for risk of thyroid C-cell tumors and are contraindicated in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). Hypoglycemia can occur, particularly when these medications are used in combination with insulin or sulfonylureas.
Regarding night sweats specifically, this symptom is not listed as a recognized side effect in the FDA-approved prescribing information for any GLP-1 receptor agonist or tirzepatide. Clinical trials and post-marketing surveillance have not established a direct causal relationship between these medications and night sweats. While individual patients may report various symptoms while taking these medications, there is no official link between GLP-1 therapy and nocturnal hyperhidrosis (excessive nighttime sweating). If night sweats occur during treatment, other causes should be thoroughly investigated.
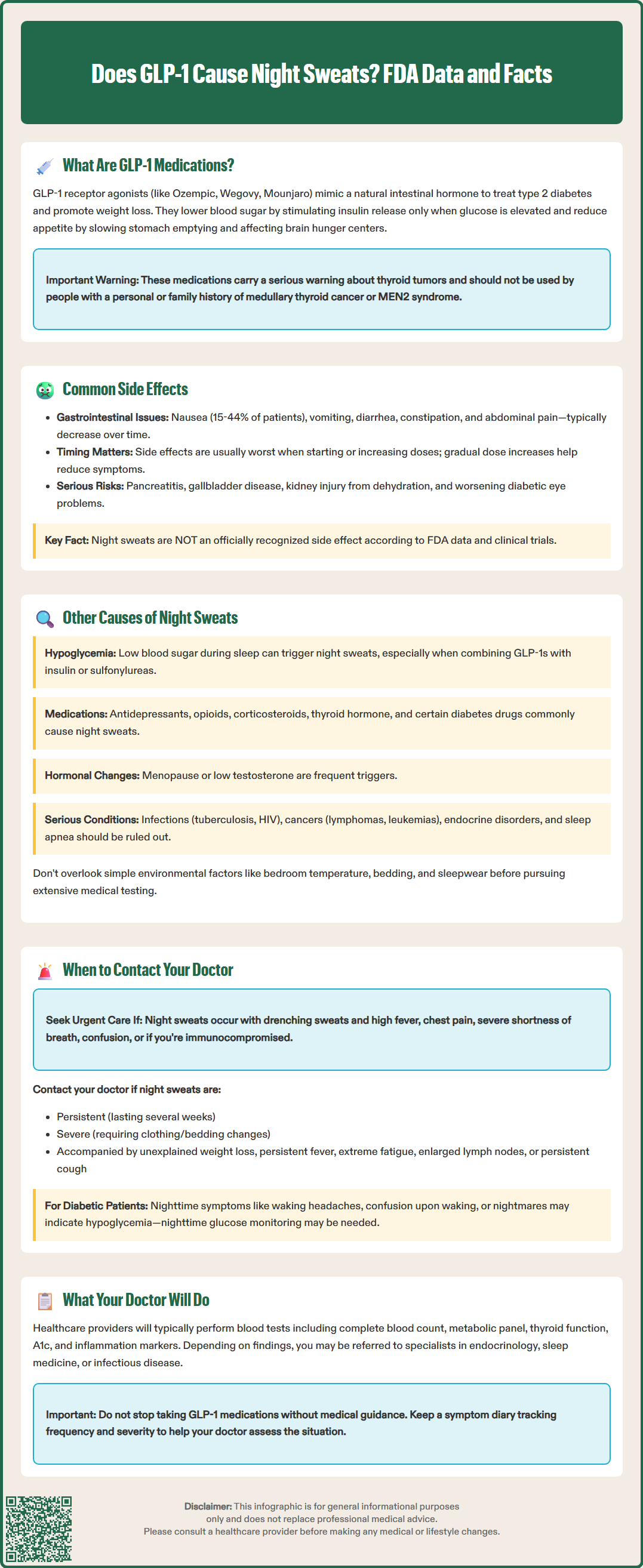
Night sweats, medically termed nocturnal hyperhidrosis, can result from numerous medical conditions and should be evaluated comprehensively. When a patient taking GLP-1 medications experiences night sweats, it is essential to consider alternative explanations rather than automatically attributing the symptom to the medication.
Hypoglycemia is an important consideration for anyone taking diabetes medications. Low blood sugar during sleep can trigger sweating, along with other symptoms such as tremors, palpitations, confusion, or nightmares. Patients taking GLP-1 medications in combination with insulin or sulfonylureas face higher risk. Checking blood glucose levels during or immediately after an episode of night sweats can help identify this cause.
Infections are common culprits, with tuberculosis and HIV being classic examples, though various bacterial, viral, and fungal infections can cause night sweats. Hormonal changes, particularly menopause in women and low testosterone in men, frequently cause nocturnal sweating. Medications known to cause night sweats include antidepressants (SSRIs, SNRIs, TCAs), opioids, hypoglycemic agents, corticosteroids, thyroid hormone, tamoxifen, and niacin. Alcohol and opioid withdrawal can also cause significant night sweats.
Malignancies, especially lymphomas and leukemias, may present with night sweats as an early symptom, often accompanied by unexplained weight loss and fever. Endocrine disorders such as hyperthyroidism, pheochromocytoma, and carcinoid syndrome can cause excessive sweating. Obstructive sleep apnea is associated with night sweats in many affected individuals.
Other considerations include gastroesophageal reflux disease (GERD), anxiety disorders, and idiopathic hyperhidrosis (excessive sweating without identifiable cause). Environmental factors such as bedroom temperature, bedding materials, and sleepwear should also be evaluated before pursuing extensive medical workup.
While occasional night sweats may not warrant immediate concern, certain features should prompt medical evaluation. Patients taking GLP-1 medications who experience night sweats should contact their healthcare provider if the sweating is persistent (occurring regularly over several weeks), severe (requiring changing of nightclothes or bedding), or accompanied by other concerning symptoms.
Seek urgent medical attention if night sweats occur with:
Drenching sweats with high fever
Chest pain or severe shortness of breath
Confusion or disorientation
Severe symptoms in immunocompromised individuals
Contact your healthcare provider if night sweats occur with:
Unexplained weight loss (beyond expected weight loss from GLP-1 therapy)
Persistent fever or chills
Fatigue that interferes with daily activities
Enlarged lymph nodes
Persistent cough
Changes in bowel habits or blood in stool (if other concerning symptoms are present)
For patients with diabetes, symptoms suggesting hypoglycemia during sleep episodes require prompt evaluation. These include waking with headaches, feeling confused or disoriented upon waking, or experiencing nightmares. Healthcare providers may recommend checking blood glucose levels during the night or using continuous glucose monitoring to identify nocturnal hypoglycemia.
Your healthcare provider will likely conduct a thorough history and physical examination, asking about the timing, severity, and pattern of night sweats, as well as reviewing all medications and supplements. Initial investigations may include complete blood count, metabolic panel, thyroid function tests, hemoglobin A1c, ESR/CRP, HIV testing, and urinalysis when clinically indicated. Depending on findings, additional testing such as chest X-ray, tuberculosis screening, or hormone levels may be appropriate.
Referrals to specialists may be necessary based on the suspected cause: endocrinology for endocrine disorders or complex hypoglycemia, sleep medicine for suspected sleep apnea, hematology/oncology for suspected malignancy, or infectious disease for chronic infections.
Patients should not discontinue GLP-1 medications without medical guidance, as there is no established connection between these drugs and night sweats. However, open communication with healthcare providers about all symptoms ensures comprehensive care and appropriate investigation of potentially significant underlying conditions. Keeping a symptom diary noting the frequency, severity, and any associated symptoms can provide valuable information for clinical assessment.
No, night sweats are not listed as a recognized side effect in FDA prescribing information for any GLP-1 receptor agonist. Clinical trials have not established a direct causal relationship between these medications and nocturnal hyperhidrosis.
The most common side effects are gastrointestinal, with nausea occurring in 15-44% of patients, followed by vomiting, diarrhea, constipation, and abdominal discomfort. These symptoms typically diminish over time with gradual dose escalation.
Contact your healthcare provider for evaluation of alternative causes such as hypoglycemia, infections, hormonal changes, or other medications. Do not discontinue GLP-1 therapy without medical guidance, as night sweats are not an established side effect of these medications.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.