LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
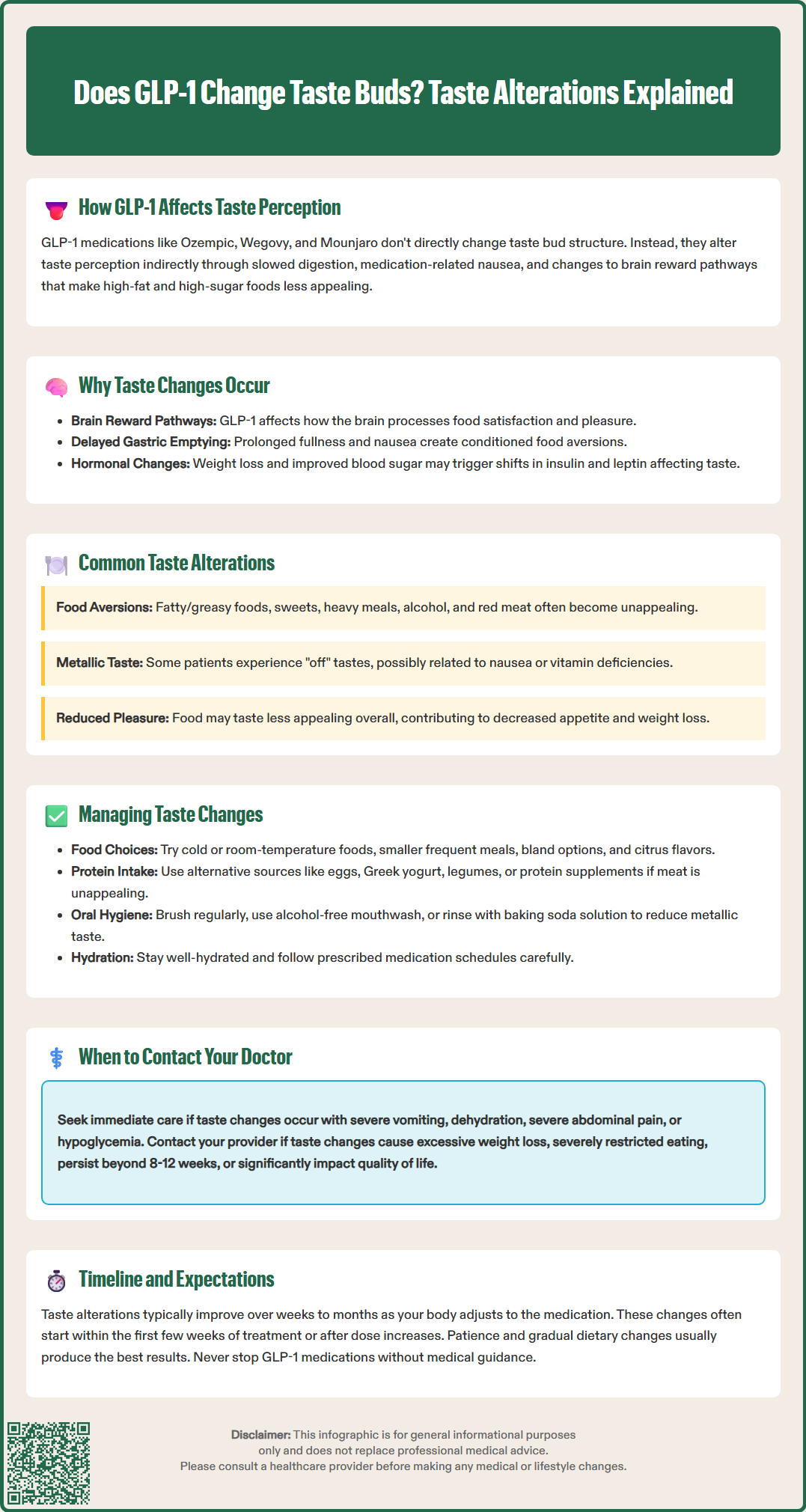
Does GLP-1 change taste buds? Many patients taking GLP-1 receptor agonists like semaglutide (Ozempic, Wegovy) or tirzepatide (Mounjaro, Zepbound) report altered taste experiences during treatment. While these medications don't directly restructure taste buds, they can significantly affect how food tastes through their effects on the brain's reward pathways, gastrointestinal function, and appetite regulation. Understanding these taste changes—from food aversions to metallic sensations—helps patients manage their treatment effectively while maintaining proper nutrition. This article explores the mechanisms behind taste alterations, common patient experiences, and practical strategies for navigating these changes during GLP-1 therapy.
Quick Answer: GLP-1 medications do not directly alter taste bud structure but can significantly change taste perception through effects on brain reward pathways, delayed gastric emptying, and gastrointestinal symptoms.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists, including semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), and liraglutide (Victoza, Saxenda), have become widely prescribed for type 2 diabetes management and weight loss. Tirzepatide (Mounjaro, Zepbound) is a dual GIP/GLP-1 receptor agonist that works through related mechanisms. While these medications are not officially documented to directly alter taste bud structure or function, many patients report changes in taste perception during treatment.
GLP-1 receptor agonists work by mimicking the naturally occurring incretin hormone GLP-1, which enhances glucose-dependent insulin secretion, suppresses glucagon release, and slows gastric emptying. These medications also act on receptors in the central nervous system, particularly in areas regulating appetite and food reward pathways. The FDA-approved labels for these agents list nausea, vomiting, and decreased appetite as common adverse effects, though taste alterations are not prominently featured in US prescribing information for most of these medications.
Patient-reported experiences and emerging clinical observations suggest that taste perception changes may occur indirectly through several mechanisms. The slowed gastric emptying characteristic of these therapies can lead to prolonged food retention, potentially affecting how flavors are perceived. Additionally, the medications' effects on nausea and the gastrointestinal system may create aversions to certain foods or alter the subjective experience of eating. While there is no established link between these medications and structural changes to taste buds themselves, the functional experience of taste can be significantly modified during treatment, impacting dietary preferences and eating behaviors in ways that may contribute to the therapeutic effects of these agents.
The mechanisms underlying taste perception changes during GLP-1 therapy are likely multifactorial and indirect rather than representing true gustatory dysfunction. Understanding these potential mechanisms helps clinicians counsel patients appropriately and distinguish between expected treatment effects and concerning adverse reactions.
Central nervous system effects may play a role in altered taste experiences. GLP-1 receptors are present in brain regions involved in reward processing, including the nucleus accumbens and ventral tegmental area. Research suggests these medications may influence reward pathways, potentially reducing the hedonic response to food—particularly high-fat and high-sugar items. This could make previously appealing foods taste less satisfying or even unpleasant. This neurobiological shift would represent a functional change in food reward rather than a peripheral taste bud alteration, though human evidence remains limited.
Gastrointestinal effects likely contribute substantially to taste perception changes. The delayed gastric emptying induced by these medications can cause:
Prolonged fullness and early satiety
Nausea and occasional vomiting
Altered oral and esophageal sensations
Potential changes in oral sensations
These gastrointestinal symptoms can create conditioned taste aversions, where the brain associates certain foods with discomfort, leading to reduced palatability. Additionally, nausea itself can influence taste perception through various physiological mechanisms.
Metabolic and hormonal changes during treatment may also influence taste perception. As patients lose weight and improve glycemic control, alterations in insulin sensitivity, leptin levels, and other metabolic hormones could potentially affect taste perception. While these changes are not well characterized in the literature, they represent hypothetical contributing factors to the subjective taste alterations patients report.
Patient experiences with taste changes during treatment with GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists vary considerably, but several patterns emerge from clinical practice and patient reports. It is important to note that these reports are largely anecdotal, as systematic studies specifically examining taste alterations with these medications remain limited. The prevalence of these effects is currently unknown, and they are not commonly listed as adverse effects in US prescribing information for most agents.
Food aversions represent the most frequently reported taste-related change. Patients commonly describe sudden disinterest in or active dislike of foods they previously enjoyed, particularly:
Fatty or greasy foods (fried items, heavy sauces, fatty meats)
Very sweet foods (desserts, sugary beverages, candy)
Rich or heavy meals
Alcohol
Certain protein sources, especially red meat
These aversions often develop within the first few weeks of treatment or following dose escalations. The intensity can range from mild preference changes to strong aversive reactions that make certain foods nearly intolerable.
Metallic or altered taste sensations are occasionally reported, though less commonly than food aversions. Some patients describe a persistent metallic taste, particularly noticeable when eating or drinking, or report that familiar foods taste "off" or different from usual. These sensations may be related to nausea, changes in oral sensations, or gastrointestinal reflux associated with delayed gastric emptying. It's important to consider other potential causes, including concurrent medications (such as metformin), vitamin deficiencies, or oral/dental conditions.
Reduced overall appetite and taste intensity is frequently noted. Patients may report that food simply tastes less appealing or that they experience diminished pleasure from eating. This reduction in taste reward may contribute to the weight loss effects.
Importantly, many patients find these taste changes helpful rather than problematic, as they facilitate adherence to reduced-calorie diets and support weight management goals. However, for some individuals, particularly those with already limited dietary variety or nutritional concerns, taste alterations can pose challenges to maintaining adequate nutrition.
While taste alterations during treatment with GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists often improve over time as patients adjust to treatment, several strategies can help manage these changes and maintain adequate nutrition and quality of life.
Dietary modifications can accommodate altered taste preferences:
Experiment with different food temperatures, as cold or room-temperature foods may be better tolerated than hot meals
Try smaller, more frequent meals rather than large portions
Focus on bland, easily digestible foods during periods of heightened nausea
Incorporate tart or citrus flavors, which some patients find more palatable
Avoid strong-smelling foods that may trigger aversions
Stay well-hydrated, as adequate fluid intake can help with metallic taste sensations
Nutritional adequacy should be monitored, particularly during significant taste changes. Patients should aim to maintain protein intake despite potential meat aversions by exploring alternative sources such as eggs, Greek yogurt, legumes, or protein supplements. A multivitamin may be appropriate for individuals with significantly restricted dietary variety, though this should be discussed with a healthcare provider first. Consultation with a registered dietitian can provide personalized guidance for meeting nutritional needs while accommodating taste changes.
Medication timing and dosing considerations may help minimize taste-related side effects. Taking medications as prescribed (daily for liraglutide; weekly for semaglutide, dulaglutide, and tirzepatide) and following dose escalation schedules carefully can reduce the intensity of gastrointestinal side effects that contribute to taste changes. Patients should not adjust doses independently but may discuss timing strategies with their healthcare provider. For patients also taking insulin or sulfonylureas, medication adjustments may be necessary to prevent hypoglycemia if food intake decreases significantly.
Oral hygiene practices can address metallic taste or altered oral sensations:
Brush teeth and tongue regularly
Use alcohol-free mouthwash
Chew sugar-free gum or mints
Rinse mouth with baking soda solution (1/4 teaspoon in 1 cup water)
Taste changes often improve over weeks to months as the body adjusts to therapy, though individual experiences vary. Patience and gradual dietary adjustments typically yield the best outcomes.
While taste changes during treatment with GLP-1 receptor agonists or dual GIP/GLP-1 receptor agonists are generally benign and self-limiting, certain situations warrant medical evaluation to rule out complications or alternative diagnoses.
Immediate medical attention is required if taste changes are accompanied by:
Severe, persistent vomiting preventing adequate fluid intake
Signs of dehydration (dark urine, dizziness, decreased urination)
Severe abdominal pain, particularly if persistent or worsening
Symptoms of pancreatitis (severe upper abdominal pain radiating to the back, nausea, vomiting)
Right upper quadrant pain, fever, or yellowing of skin/eyes (possible gallbladder disease)
Symptoms of hypoglycemia (if also taking insulin or sulfonylureas): shakiness, sweating, confusion, irritability
These symptoms may indicate serious adverse effects requiring urgent evaluation, including pancreatitis, gallbladder disease, gastroparesis, or severe dehydration.
Routine consultation with your healthcare provider is appropriate when:
Taste changes lead to significant unintentional weight loss beyond treatment goals
Nutritional intake becomes severely restricted, raising concerns about deficiencies
Taste alterations persist beyond 8-12 weeks without improvement
Quality of life is substantially impacted by food aversions or taste disturbances
New or worsening symptoms develop, such as persistent metallic taste with other concerning features
Your provider can assess whether taste changes represent expected treatment effects or require investigation for alternative causes. Evaluation may include laboratory tests for vitamin B12 or zinc deficiency, medication review, and screening for conditions such as gastroesophageal reflux disease or oral/dental issues. Conditions such as vitamin deficiencies, medication interactions, or unrelated oral or neurological conditions can cause taste disturbances and should be considered in the differential diagnosis.
Medication adjustment may be necessary in some cases. If taste changes significantly impair nutrition or quality of life despite management strategies, your healthcare provider may consider dose reduction, temporary treatment interruption, or switching to an alternative medication. According to American Diabetes Association guidelines, treatment should be individualized based on patient tolerance, efficacy, and overall benefit-risk profile. Never discontinue therapy without medical guidance, as abrupt cessation can lead to loss of glycemic control or weight regain. Open communication with your healthcare team ensures that taste-related concerns are addressed while maintaining therapeutic benefits.
No, GLP-1 medications do not permanently alter taste bud structure. Most taste changes are temporary and improve over weeks to months as your body adjusts to treatment, though individual experiences vary.
These medications affect brain reward pathways that process food pleasure and cause delayed gastric emptying, which can create food aversions and alter taste perception. Nausea and gastrointestinal effects also contribute to changes in how foods taste.
Contact your healthcare provider if taste changes cause severe nutritional restriction, persist beyond 8-12 weeks without improvement, or are accompanied by concerning symptoms like persistent vomiting, severe abdominal pain, or signs of dehydration.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.