LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Does GLP-1 help with endometriosis? Many patients wonder whether GLP-1 receptor agonists—medications approved for type 2 diabetes and weight management—might offer benefits for endometriosis. As of 2024, there is no established clinical connection between GLP-1 medications and endometriosis treatment. These drugs target metabolic pathways involving glucose regulation and appetite control, not the hormonal and inflammatory mechanisms underlying endometriosis. While GLP-1 receptor agonists have demonstrated anti-inflammatory effects in metabolic contexts, no evidence supports their use for endometriosis-related pain or inflammation. Understanding the science behind these medications and evidence-based endometriosis treatments helps patients make informed decisions about their care.
Quick Answer: GLP-1 receptor agonists are not indicated for endometriosis treatment and have no established clinical benefit for this condition.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists are a class of medications originally developed to manage type 2 diabetes and, more recently, approved for chronic weight management. These medications work by mimicking the action of naturally occurring GLP-1, a hormone produced in the intestines that plays multiple roles in metabolic regulation.
The primary mechanism of action involves stimulating insulin secretion in a glucose-dependent manner, meaning they promote insulin release only when blood sugar levels are elevated. This reduces the risk of hypoglycemia compared to some other diabetes medications. GLP-1 receptor agonists also slow gastric emptying, which helps control post-meal blood sugar spikes and promotes satiety. Additionally, they suppress glucagon secretion from the pancreas, further contributing to improved glycemic control.
Currently available GLP-1 medications in the United States include semaglutide (Ozempic, Wegovy, Rybelsus), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), exenatide extended-release (Bydureon BCise), and tirzepatide (Mounjaro, Zepbound)—with tirzepatide being a dual GIP/GLP-1 receptor agonist rather than a pure GLP-1 agonist. The FDA has approved these agents specifically for type 2 diabetes management and, in some formulations, for weight management in adults with obesity or overweight with at least one weight-related comorbidity.
Important safety information includes a boxed warning for risk of thyroid C-cell tumors, with contraindications in patients with personal or family history of medullary thyroid carcinoma (MTC) or Multiple Endocrine Neoplasia syndrome type 2 (MEN2). These medications are contraindicated during pregnancy and require discontinuation before planned conception (typically ≥2 months for semaglutide and ≥1 month for tirzepatide). Additional warnings include risk of diabetic retinopathy complications with rapid glucose improvement, acute kidney injury with dehydration, and gallbladder disease.
Some GLP-1 medications may reduce the effectiveness of oral contraceptives. Tirzepatide requires non-oral or backup contraception for 4 weeks after starting or increasing doses. Exenatide immediate-release requires taking oral contraceptives at least 1 hour before administration.
Common adverse effects include gastrointestinal symptoms such as nausea, vomiting, diarrhea, and constipation, which typically diminish over time. These medications are administered via subcutaneous injection (with one oral formulation available) and require patient education regarding proper administration technique and storage.
As of 2024, there is no established clinical connection between GLP-1 receptor agonists and endometriosis treatment. Endometriosis is a chronic inflammatory condition characterized by the presence of endometrial-like tissue outside the uterus, causing pain, inflammation, and potential fertility issues. The pathophysiology involves hormonal influences, immune dysfunction, and inflammatory processes—mechanisms that differ substantially from the metabolic pathways targeted by GLP-1 medications.
GLP-1 receptor agonists were not designed to address the hormonal or inflammatory components of endometriosis. Their primary therapeutic targets are glucose metabolism, insulin sensitivity, and appetite regulation. While these medications have demonstrated anti-inflammatory properties in some metabolic contexts, there is no evidence that these effects translate to meaningful benefits for endometriosis-related inflammation or pain.
Some interest in GLP-1 medications and endometriosis may stem from observations regarding weight management and metabolic health. Women with endometriosis may experience weight changes related to hormonal treatments or reduced physical activity due to pain. Some patients may have both endometriosis and polycystic ovary syndrome (PCOS), though these are distinct conditions without a proven causal relationship. However, addressing weight concerns does not directly treat the underlying endometriosis pathology.
It is important to emphasize that GLP-1 receptor agonists are not approved by the FDA for endometriosis management, and there is no official indication for their use in this condition. Any perceived benefits would be indirect at best, and patients should not expect these medications to alleviate endometriosis symptoms such as pelvic pain, dysmenorrhea, or dyspareunia. Healthcare providers prescribing GLP-1 medications for approved indications in patients who also have endometriosis should manage each condition according to evidence-based guidelines specific to that diagnosis.
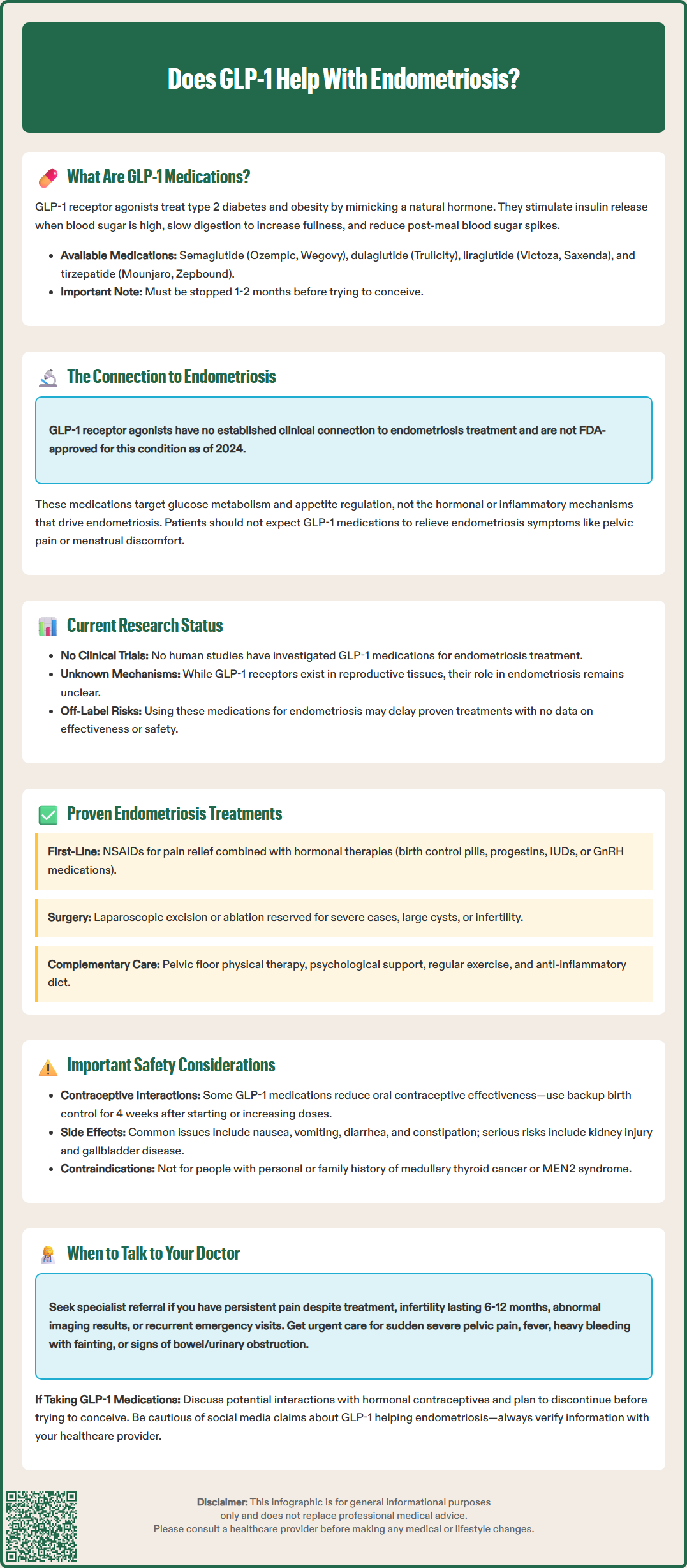
As of 2024, there are no published human clinical trials specifically investigating GLP-1 receptor agonists as a treatment for endometriosis. The absence of clinical evidence means that any claims regarding efficacy would be speculative and not supported by scientific data. Clinicians and patients should approach this topic with appropriate skepticism and rely on established treatment modalities.
Some preliminary laboratory research has explored GLP-1 receptors in reproductive tissues and their potential role in various gynecological conditions, but this work remains in early stages and has not translated to clinical applications for endometriosis. While GLP-1 receptors have been identified in the female reproductive tract, the functional significance of these receptors in endometriosis pathogenesis is unknown.
The broader anti-inflammatory effects of GLP-1 receptor agonists observed in cardiovascular and metabolic research have generated interest in potential applications beyond diabetes and obesity. However, inflammation in endometriosis involves specific immune cell populations, cytokine profiles, and hormonal interactions that differ from metabolic inflammation. Extrapolating findings from one inflammatory context to another without supporting evidence is not scientifically sound.
Patients and healthcare providers should be aware that off-label use of medications without supporting evidence carries risks and may delay appropriate treatment. The lack of research on GLP-1 medications for endometriosis means there is no data on efficacy, optimal dosing, treatment duration, or potential interactions with standard endometriosis therapies. Until well-designed clinical trials demonstrate benefit, GLP-1 receptor agonists should not be considered a treatment option for endometriosis. Women interested in emerging therapies should discuss participation in clinical trials with their healthcare providers or seek information through reputable sources such as ClinicalTrials.gov (search terms: endometriosis AND GLP-1 OR semaglutide OR tirzepatide).
Evidence-based management of endometriosis involves a multimodal approach tailored to symptom severity, fertility goals, and patient preferences. First-line medical management typically includes nonsteroidal anti-inflammatory drugs (NSAIDs) for pain relief and hormonal therapies to suppress endometrial tissue growth and reduce inflammation.
Hormonal treatment options include:
Combined oral contraceptives: Continuous or cyclic regimens can reduce menstrual flow and suppress endometrial tissue activity
Progestins: Available as oral medications, injections (depot medroxyprogesterone acetate), intrauterine devices (levonorgestrel-releasing IUD), or implants
GnRH agonists: These medications induce a temporary menopausal state, effectively suppressing endometriosis but requiring add-back hormone therapy to minimize bone loss and vasomotor symptoms
GnRH antagonists: FDA-approved oral options include elagolix (Orilissa) and relugolix/estradiol/norethindrone (Myfembree) with specific duration limits based on dosing and bone health considerations
Aromatase inhibitors: Sometimes used in refractory cases, though not FDA-approved for this indication
Bone mineral density monitoring is recommended for patients on long-term GnRH agonists or antagonists, particularly at higher doses or extended durations. Contraception is required during treatment with these agents due to potential fetal harm.
Surgical intervention may be appropriate for patients with severe symptoms unresponsive to medical management, those with endometriomas affecting ovarian function, or women experiencing infertility. Laparoscopic excision or ablation of endometriotic lesions can provide symptom relief and improve fertility outcomes in selected cases. However, endometriosis recurrence after surgery is common, and many patients require ongoing medical management.
Red flag symptoms requiring urgent evaluation include sudden severe pelvic/abdominal pain, fever, heavy bleeding with syncope, positive pregnancy test (to rule out ectopic pregnancy), or signs of bowel or urinary obstruction.
Complementary approaches that may provide additional benefit include pelvic floor physical therapy for associated muscle dysfunction, psychological support for chronic pain management, and lifestyle modifications including regular exercise and anti-inflammatory dietary patterns. The American College of Obstetricians and Gynecologists (ACOG) emphasizes individualized treatment plans that consider the patient's age, symptom severity, fertility desires, and treatment preferences. Multidisciplinary care involving gynecologists, pain specialists, and mental health professionals often provides the most comprehensive management for this complex condition.
If you have endometriosis and are curious about GLP-1 medications, it is essential to have an open, informed conversation with your healthcare provider. Begin by clarifying your treatment goals—whether you are seeking better pain control, fertility preservation, management of coexisting conditions, or weight management. Understanding your priorities will help guide appropriate treatment decisions.
Patients should ask specific questions about any proposed treatments:
What is the evidence supporting this treatment for my condition?
What are the expected benefits and potential risks?
How does this treatment interact with my current medications?
What are the alternatives if this approach is not appropriate?
What monitoring or follow-up will be necessary?
If you are taking or considering a GLP-1 receptor agonist for an approved indication such as type 2 diabetes or weight management, discuss how this medication might interact with your endometriosis treatment plan. Important considerations include:
Potential interactions with hormonal contraceptives (particularly with tirzepatide and exenatide)
Pregnancy planning (GLP-1 medications require discontinuation before conception—typically ≥2 months for semaglutide and ≥1 month for tirzepatide)
Management of gastrointestinal side effects that might overlap with endometriosis symptoms
Some hormonal therapies for endometriosis can affect weight, and addressing metabolic health may be a separate but important consideration. However, it is crucial to understand that treating one condition does not necessarily improve the other.
Be cautious about information from non-medical sources, including social media, where anecdotal reports may create unrealistic expectations. If you encounter claims about GLP-1 medications helping endometriosis, bring these to your provider's attention for professional evaluation.
Consider seeking referral to a specialist if you experience persistent pain despite first-line therapy, infertility after 6-12 months of attempting conception (earlier if age ≥35), abnormal imaging findings (such as endometriomas), or recurrent emergency department visits. Gynecologists specializing in endometriosis or reproductive endocrinologists can offer advanced treatment options and may have access to clinical trials investigating novel therapies. Comprehensive endometriosis care centers often provide multidisciplinary evaluation and can address the various dimensions of this challenging condition, ensuring you receive the most appropriate, evidence-based care available.
No, GLP-1 receptor agonists are not approved for endometriosis and have no clinical evidence supporting their use for endometriosis-related pain or inflammation. These medications target metabolic pathways rather than the hormonal and inflammatory mechanisms underlying endometriosis.
Evidence-based endometriosis treatments include hormonal therapies such as combined oral contraceptives, progestins, GnRH agonists, and GnRH antagonists (elagolix, relugolix combination), along with NSAIDs for pain management. Surgical intervention may be appropriate for severe symptoms or fertility concerns.
If you are taking a GLP-1 medication for an approved indication like type 2 diabetes or weight management, continue as prescribed and manage endometriosis separately with evidence-based treatments. Discuss any concerns with your healthcare provider, particularly regarding contraceptive interactions and pregnancy planning.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.