LOSE WEIGHT WITH MEDICAL SUPPORT — BUILT FOR MEN
- Your personalised programme is built around medical care, not willpower.
- No generic diets. No guesswork.
- Just science-backed results and expert support.
Find out if you’re eligible
Glucagon-like peptide-1 (GLP-1) receptor agonists—including semaglutide (Ozempic, Wegovy), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), and tirzepatide (Mounjaro, Zepbound)—are FDA-approved medications for type 2 diabetes and chronic weight management. As their use has expanded, questions about long-term safety have emerged, particularly regarding potential cancer risk. Current evidence from large-scale clinical trials and meta-analyses does not establish a causal link between GLP-1-based therapies and increased overall cancer risk in humans. However, the FDA requires a boxed warning for thyroid C-cell tumors based on rodent studies, though human relevance remains uncertain. Understanding the available safety data helps patients and clinicians make informed treatment decisions.
Quick Answer: Current evidence from large-scale clinical trials does not show that GLP-1 receptor agonists increase overall cancer risk in humans.
We offer compounded medications and Zepbound®. Compounded medications are prepared by licensed pharmacies and are not FDA-approved. References to Wegovy®, Ozempic®, Rybelsus®, Mounjaro®, or Saxenda®, or other GLP-1 brands, are informational only. Compounded and FDA-approved medications are not interchangeable.
Glucagon-like peptide-1 (GLP-1) receptor agonists represent a class of medications originally developed for type 2 diabetes management, with select agents now FDA-approved for chronic weight management. These drugs include semaglutide (Ozempic, Wegovy), dulaglutide (Trulicity), liraglutide (Victoza, Saxenda), and tirzepatide (Mounjaro, Zepbound)—though tirzepatide is technically a dual glucose-dependent insulinotropic polypeptide (GIP)/GLP-1 receptor agonist. These medications work by mimicking naturally occurring hormones that regulate blood sugar and appetite. As their use has expanded dramatically in recent years, questions about long-term safety, including potential cancer risk, have become increasingly important for both patients and clinicians.
The concern about these medications and cancer stems from several factors. First, GLP-1 receptors are found not only in the pancreas and gastrointestinal tract but also in various other tissues throughout the body, raising theoretical questions about how chronic stimulation of these receptors might affect cell growth. Second, early animal studies identified potential signals that warranted further investigation. Third, the rapid weight loss associated with these medications represents a significant metabolic change that could theoretically influence cancer detection or progression.
It is essential to distinguish between theoretical concerns, preliminary signals in preclinical research, and actual evidence of increased cancer risk in humans. The FDA and other regulatory agencies have conducted extensive reviews of safety data from clinical trials and post-marketing surveillance. Current evidence does not establish a causal link between GLP-1-based therapies and increased overall cancer risk in humans, though ongoing monitoring continues as these medications are used by growing numbers of patients over longer time periods.
Large-scale clinical trials and meta-analyses have generally been reassuring regarding cancer risk with GLP-1-based therapies. The cardiovascular outcomes trials that enrolled tens of thousands of patients with type 2 diabetes—including LEADER (liraglutide), SUSTAIN-6 (semaglutide), REWIND (dulaglutide), and EXSCEL (exenatide ER)—found no significant increase in overall cancer incidence compared to placebo over follow-up periods ranging from approximately two to five years. These trials were not specifically designed to assess cancer outcomes, but they provide valuable safety data from well-controlled studies.
A comprehensive 2022 meta-analysis by Dicembrini et al. published in Diabetes, Obesity and Metabolism examined data from 52 randomized controlled trials involving over 75,000 participants treated with GLP-1 receptor agonists. The analysis found no statistically significant increase in overall cancer risk, with a pooled risk ratio of 0.98 (95% CI 0.83-1.15), indicating similar cancer rates between GLP-1-treated patients and control groups. Subgroup analyses by drug type, duration of treatment, and patient characteristics similarly showed no concerning signals.
Observational studies have added further evidence. Nordic registry studies comparing cancer incidence in patients prescribed GLP-1 receptor agonists versus other diabetes medications have generally found no elevated risk after adjustment for available confounding factors. However, these observational studies have inherent limitations, including potential residual confounding (as some registries lack complete data on important cancer risk factors like smoking), selection bias, and the challenge of detecting rare events.
It is important to note that most available data reflect relatively short to medium-term exposure (typically under five years). Cancer development is often a slow process, and longer-term surveillance data will be valuable as patients continue these medications for extended periods, particularly for weight management in younger populations without diabetes.
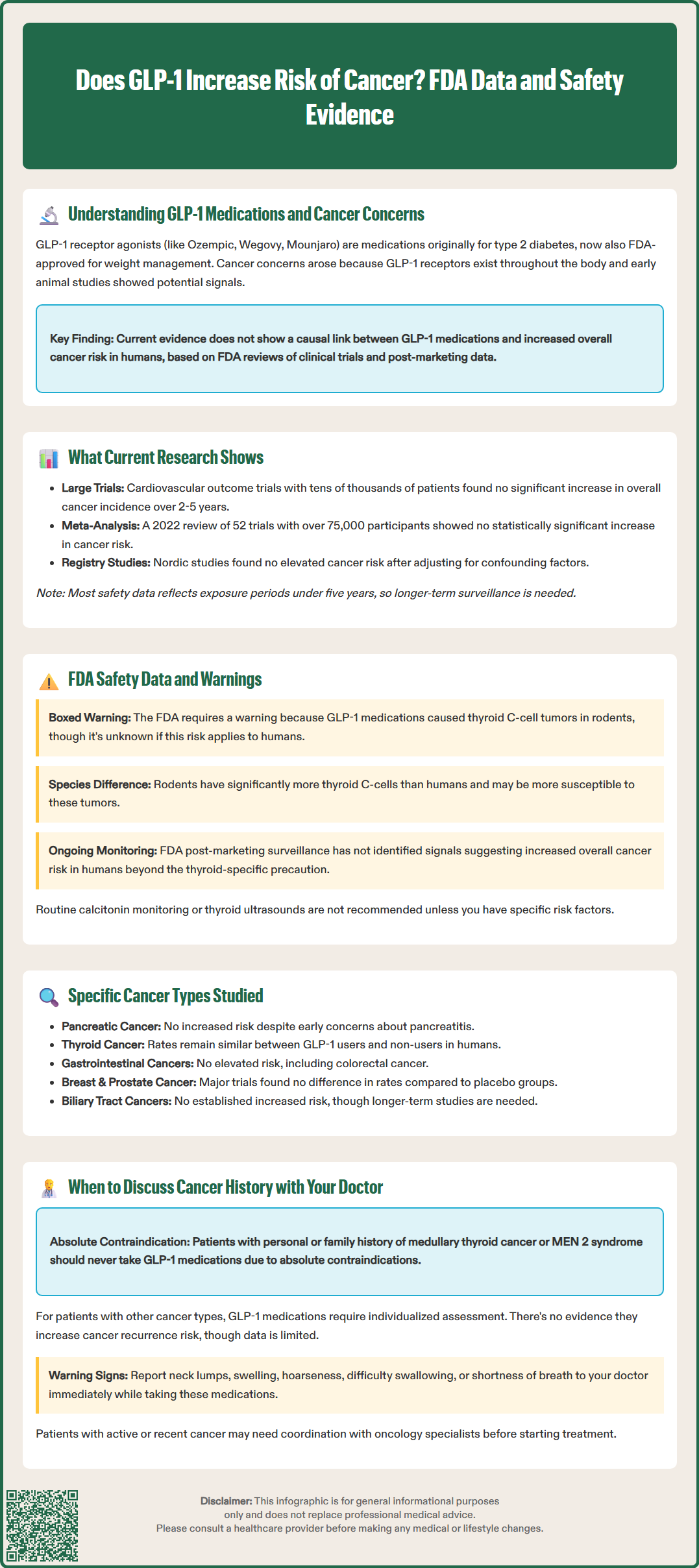
The FDA has conducted thorough reviews of cancer-related safety data for all approved GLP-1 receptor agonists and dual GIP/GLP-1 receptor agonists. These reviews include analysis of preclinical animal studies, clinical trial data, and post-marketing adverse event reports. The FDA's prescribing information (labels) for these medications reflects the agency's assessment of cancer-related risks based on available evidence.
For thyroid C-cell tumors specifically, the FDA requires a boxed warning—the agency's strongest safety warning—for several products including semaglutide (Ozempic, Wegovy, Rybelsus), liraglutide (Victoza, Saxenda), dulaglutide (Trulicity), exenatide extended-release (Bydureon BCise), and tirzepatide (Mounjaro, Zepbound). This warning is based on findings in rodent studies where these drugs caused thyroid C-cell tumors (medullary thyroid carcinoma) at clinically relevant exposures. However, the FDA label explicitly states that "it is unknown whether GLP-1 receptor agonists cause thyroid C-cell tumors, including medullary thyroid carcinoma (MTC), in humans, as the human relevance of GLP-1 receptor agonist-induced rodent thyroid C-cell tumors has not been determined." The rodent thyroid has substantially more C-cells than the human thyroid, and rodents may be more susceptible to this effect.
The FDA's post-marketing surveillance system (FAERS—FDA Adverse Event Reporting System) continuously monitors reports of cancer in patients taking these medications. While individual case reports of various cancers have been submitted, these reports do not establish causation, as patients taking these medications have multiple risk factors for cancer, including obesity, diabetes, and age. The FDA has not identified signals suggesting increased overall cancer risk that would warrant additional warnings beyond the thyroid-specific precaution.
Clinicians should be aware that the FDA contraindications for products with the thyroid C-cell tumor boxed warning include personal or family history of medullary thyroid carcinoma and multiple endocrine neoplasia syndrome type 2 (MEN 2). These contraindications are precautionary measures based on the rodent findings and the known genetic basis of these conditions. Routine monitoring of calcitonin or thyroid ultrasound is not recommended in patients without specific risk factors.
Clinical trials have examined the incidence of various cancer types in patients receiving GLP-1-based therapies. Pancreatic cancer has received particular attention due to the pancreatic expression of GLP-1 receptors and early concerns about pancreatitis potentially increasing cancer risk. However, pooled analyses of clinical trial data have not demonstrated increased pancreatic cancer incidence with these medications. A 2014 FDA and European Medicines Agency (EMA) joint analysis found similar rates of pancreatic cancer between GLP-1-treated patients and comparators, though absolute event numbers were small.
Thyroid cancer, particularly medullary thyroid carcinoma (MTC), has been closely monitored given the rodent study findings. In human clinical trials, cases of thyroid cancer have been rare and occurred at similar rates in treatment and control groups. Post-marketing data have not revealed an increased incidence of MTC in patients treated with these medications, though the baseline incidence of this rare cancer type is very low (approximately 1-2 cases per 100,000 people annually).
Gastrointestinal cancers, including colorectal cancer, have been evaluated given the high concentration of GLP-1 receptors in the gut. Clinical trial data have not shown increased risk of these malignancies. Some researchers have hypothesized potential metabolic effects that could influence cancer risk, though this remains speculative and requires further research.
Breast, prostate, and other common cancers have also been tracked in clinical trials. The LEADER trial, for example, reported similar rates of breast cancer, prostate cancer, and other malignancies between liraglutide and placebo groups. Analyses of the SUSTAIN and PIONEER trial programs for semaglutide found no imbalance in cancer incidence across treatment groups.
Gallbladder and biliary tract events have been reported with GLP-1-based therapies, primarily related to gallstones. While some concerns were raised about potential cholangiocarcinoma risk, subsequent analyses have not established an increased risk of biliary tract cancers.
It is important to recognize that clinical trials may have limited power to detect small increases in risk for specific rare cancer types, and longer-term observational studies will continue to provide important safety information.
Patients considering GLP-1 receptor agonist or dual GIP/GLP-1 receptor agonist therapy should have an open discussion with their healthcare provider about personal and family cancer history. This conversation is particularly important for individuals with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN 2), as these represent absolute contraindications to the use of products with the thyroid C-cell tumor boxed warning, including semaglutide, liraglutide, dulaglutide, exenatide extended-release, and tirzepatide. Patients with these conditions should not receive these medications, and alternative treatments for diabetes or weight management should be considered.
For patients with a history of other cancer types, the decision to use these medications requires individualized assessment. There is no evidence that GLP-1-based therapies increase the risk of cancer recurrence, but limited data exist specifically addressing this question. Factors to consider include the type of cancer, time since treatment, current cancer status, and the potential benefits of therapy for diabetes control or weight loss. In many cases, the metabolic benefits of these medications may outweigh theoretical concerns, particularly for patients with significant obesity or poorly controlled diabetes, which themselves carry health risks.
Patients should inform their doctor if they develop symptoms that could indicate thyroid problems while taking these medications, including a lump or swelling in the neck, hoarseness, difficulty swallowing, or shortness of breath. While these symptoms are rarely due to thyroid cancer, they warrant prompt evaluation. Routine thyroid monitoring (such as calcitonin testing or ultrasound) is not recommended for patients without specific risk factors, as this has not been shown to be beneficial and may lead to unnecessary interventions.
Clinicians should document cancer history in the medical record and consider this information when weighing the benefits and risks of therapy. For patients with active cancer or recent cancer treatment, coordination with oncology specialists may be appropriate. The American Diabetes Association Standards of Care emphasize individualized treatment decisions that consider patient preferences, comorbidities, and safety considerations. As with any medication, ongoing monitoring and open communication between patients and healthcare providers remain essential for safe and effective use of these medications.
Patients and healthcare providers can report suspected adverse events related to these medications to the FDA through the MedWatch program (www.fda.gov/medwatch or 1-800-FDA-1088).
Large-scale clinical trials and meta-analyses have not found a significant increase in overall cancer risk with GLP-1 receptor agonists. The FDA requires a boxed warning for thyroid C-cell tumors based on rodent studies, but it remains unknown whether this applies to humans.
Patients with a personal or family history of medullary thyroid carcinoma or multiple endocrine neoplasia syndrome type 2 (MEN 2) should not take GLP-1 medications with the thyroid C-cell tumor boxed warning. These are absolute contraindications based on precautionary measures.
Routine thyroid monitoring with calcitonin testing or ultrasound is not recommended for patients without specific risk factors. However, you should report symptoms like neck lumps, hoarseness, or difficulty swallowing to your doctor promptly.
All medical content on this blog is created using reputable, evidence-based sources and is regularly reviewed for accuracy and relevance. While we strive to keep our content current with the latest research and clinical guidelines, it is intended for general informational purposes only.
This content is not a substitute for professional medical advice, diagnosis, or treatment. Always consult a licensed healthcare provider with any medical questions or concerns. Use of this information is at your own risk, and we are not liable for any outcomes resulting from its use.